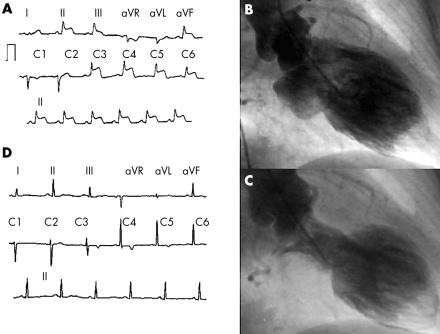
A 64 year old woman under antidepressant treatment, but with no coronary risk factors, was admitted to our institution with a two day history of continuous atypical chest pain. The ECG showed pronounced ST segment elevation in leads II, III, aVF and V2–V6 (panel A). Coronary angiography revealed normal coronary arteries and left ventriculography demonstrated apical asynergy with basal hyperkinesia (“apical ballooning”). A striking filling defect—highly suggestive of a thrombus—was also viewed at the apex (panel B, diastole; panel C, systole). Left ventricular ejection fraction (LVEF) was 40%. The apical ballooning, intraventricular thrombus, and a dynamic intraventricular pressure gradient of 70 mm Hg were confirmed by transthoracic echocardiography (TTE). Maximal creatine phosphokinase and troponin I values were 159 U/l (normal 0–170 U/l) and 7.4 ng/ml (normal 0–0.1 ng/ml), respectively. Nevertheless, pathologic Q waves developed from V1 to V3. The patient was discharged under anticoagulant treatment. Three months later the ECG showed no Q waves but just negative T waves on V3–V6 (panel D). TTE showed absolutely normal left ventricular wall motion, an LVEF of 62%, and complete resolution of the apical thrombus and intraventricular pressure gradient. Anticoagulation was discontinued.
Apical ballooning has been recently described. Clinical presentation includes chest pain, ST segment elevation on ECG, and minimal or no rise of cardiac enzymes in patients with normal angiographic coronary arteries, but with a peculiarly shaped left ventricle. Full recovery of left ventricular wall motion should occur within weeks. Although some major complications have been associated with this entity (namely, heart failure and arrhythmias) the clinical course and prognosis is favourable in most cases. Apical thrombus has not been previously described in patients with apical ballooning.