Abstract
Objective: To review the diagnosis, treatment, and outcome of fetal atrial flutter compared with supraventricular tachycardia.
Design: Retrospective review of published reports: 11 papers about fetal tachyarrhythmia published between 1991 and 2002 were selected for review.
Main outcome measures: All selected studies were analysed for the type of arrhythmia, degree of atrioventricular block in atrial flutter, occurrence of hydrops fetalis, gestational age at diagnosis, first and second line drug treatment, associated cardiac and extracardiac malformations, and mortality of the fetuses.
Results: Atrial flutter accounted for 26.2% of all cases of fetal tachyarrhythmias, and supraventricular tachycardia for 73.2%. Hydrops fetalis was reported in 38.6% and 40.5% of fetuses with atrial flutter and supraventricular tachycardia, respectively (NS). Hydropic fetuses with atrial flutter had higher ventricular rates (median 240 beats/min, range 240–300) than non-hydropic fetuses (220 beats/min, range 200–310) (p = 0.02), whereas the atrial rates were not significantly different (median 450 beats/min, range 370–500). Digoxin treatment resulted in a higher conversion rate in non-hydropic fetuses with fetal tachyarrhythmias than in hydropic fetuses (p < 0.001). The overall mortality of atrial flutter was similar to that of supraventricular tachycardia, at 8.0% v 8.9% (p = 0.7).
Conclusions: The prevalence of hydrops fetalis did not differ in fetal atrial flutter and supraventricular tachycardia with 1:1 conduction. There was no difference between the response rate to digoxin in fetus with atrial flutter or supraventricular tachycardia. Mortality was similar in the two types of tachyarrhythmia.
Keywords: fetus, tachyarrhythmia, atrial flutter, supraventricular tachycardia
A ccording to published reports, atrial flutter accounts for a fifth to a third of all fetal tachyarrhythmias.1,2 Fetal atrial flutter is defined as a rapid regular atrial rate of 300–600 beats/min accompanied by variable degrees of atrioventricular (AV) conduction block, resulting in slower ventricular rates. Previous data have suggested that fetal atrial flutter carries a worse prognosis than fetal supraventricular tachycardia (SVT) with 1:1 AV conduction, because of difficulties in controlling this rhythm disorder and the likelihood of associated congenital cardiac malformations.3 In contrast, Simpson and Sharland recently reported that the outcome of fetal tachyarrhythmias depends on the presence or absence of hydrops fetalis but not on the type of arrhythmia.2 Our aim in the present study was to review the diagnosis, treatment, and outcome of fetal atrial flutter compared with SVT.
METHODS
Study population
For the review, data were collected from publications about fetal tachyarrhythmias published from 1990 onwards. Eleven papers about fetal tachyarrhythmia1,2,4–12 were selected from the Medline database according to the following criteria:
only articles with more than 10 cases of fetal tachyarrhythmia were included
all publications had to contain data about consecutive cases of fetal tachyarrhythmia.
articles dealing with isolated series of subgroups of fetal tachyarrhythmias were excluded.
One paper1 provided detailed data on fetuses with atrial flutter but not on fetuses with SVT; a complementary publication13 was therefore used to analyse the data on the corresponding fetuses with SVT. When evaluation of the publications of one centre revealed case overlap, the most recent studies were selected1,2,7 and previous articles14–17 were excluded from the review.
Our data were retrieved from a recent publication12 and were completed by previously published18,19 and unpublished data. Where available, extended data were obtained by direct communication with the relevant authors.2,5,7
All selected studies were analysed for the type of arrhythmia, degree of AV block in atrial flutter, absence or presence of hydrops fetalis, gestational age at diagnosis, first and second line drug treatment, associated cardiac and extracardiac malformations, and mortality of the fetuses.
Statistics
We used dichotomous and continuous outcome variables. The pooled effect estimate and tests for heterogeneity between studies were undertaken with the REVMAN 4.1 statistical software package (Review Manager (RevMan), version 4.1 for Windows. Oxford: The Cochrane Collaboration, 2000). In the presence of significant heterogeneity we used a random effects model, and otherwise a fixed effects model was used. Odds ratios (OR) and 95% confidence intervals (CI) were calculated for dichotomous data using the appropriate model. Continuous data were pooled with weighted mean differences (WMD). The box size of the weighted mean difference graphs represent the size and weight of the study.
The Mann-Whitney test was used to compare the ventricular rates of fetuses with atrial flutter with and without hydrops fetalis. Probability values of p < 0.05 were considered significant.
RESULTS
Population
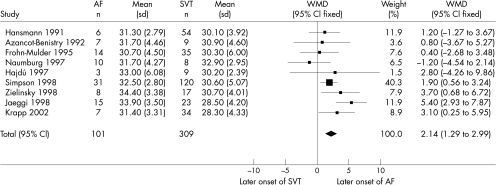
In all, 485 cases were available for analysis (table 1)1,2,4–12; 73.2% of these fetuses (range 63.6–90.0%) had SVT (n = 355) and 26.2% (range 10–61.1%) had atrial flutter (n = 127). Ventricular tachycardia (three fetuses) was rare.6,7 At diagnosis, the mean gestational age of the fetuses with atrial flutter, reported in 10 of the 11 papers,1,2,4–7,9–12 ranged between 30.7 and 34.4 weeks (table 1); in fetal SVT, the means were between 28.4 and 32.9 weeks (table 1). Atrial flutter was detected significantly later than SVT, by 2.1 weeks (95% CI 1.29 to 2.99 weeks) (p < 0.00001) (fig 1).
Table 1.
Selected publications on fetal tachyarrhythmia
| Number of fetuses | Number of hydropic fetuses | Mean (SD) GA at diagnosis | Number of cases treated with D as first line therapy (success rate in %) | Dead fetuses (hydropic) | ||||||
| Author | AF | SVT | AF | SVT | AF | SVT | AF | SVT | AF | SVT |
| Hansmann 19914 | 6 | 54 | 5 | 21 | 31.3 (2.79) | 30.1 (3.92) | 6 (16.7) | 53 (26.4) | 2 (2) | 4 (4) |
| Azancot-Benistry 19925 | 7 | 9 | 2 | 7 | 31.7 (4.46) | 30.9 (4.60) | 7 (14.3) | 9 (66.7) | 0 | 0 |
| VanEngelen 19946 | 16 | 34 | 6 | 16 | 33.0 (*) | 30.0 (*) | * | * | * | * |
| Frohn-Mulder 19957 | 14 | 35 | 3 | 13 | 30.7 (4.50) | 30.3 (6.00) | 9 (55.6) | 15 (46.7) | 3 (3) | 3 (3) |
| Soyeur 19968 | 10 | 7 | 10 | * | * | * | 8 (62.5) | * | 1 | 0 |
| Hajdú 19979 | 3 | 9 | 1 | 5 | 33.0 (6.08) | 30.2 (2.39) | 3 | 1 | 0 | 0 |
| Naumburg 199710 | 10 | 8 | 4 | 3 | 31.7 (4.27) | 32.9 (2.95) | 8 (37.5) | 7 (28.6) | 0 | 0 |
| Zielinsky 199811 | 8 | 17 | 6 | 6 | 34.4 (3.38) | 30.7 (4.01) | 5 (0) | 17 (76.5) | 0 | 3 (3) |
| Simpson 19982 § | 31 | 120 | 11 | 47 | 32.5 (2.80) | 30.6 (5.07) | 13 (69.2) | 53 (81.1) | 2 | 17 |
| Jaeggi 19981/Jaeggi 199813¶ | 15 | 28 | 1 | 5¶ | 33.9 (3.50) | 28.5 (4.20)¶ | 11 (50.0†) | 18 (50.0)¶ | 0 | 1 (1)¶ |
| Krapp 200212 ‡ | 7 | 34 | 0 | 18 | 31.4 (3.31) | 28.4 (4.33) | 7 (42.9) | 26 (30.8) | 1 (0) | 0 |
| Total | 127 | 355 | 49 (38.6) | 141 (40.5) | 75 (45.1) | 199 (51.5) | 9 | 28 | ||
*No data available.
§Unpublished data of expanded series until December 1999.
¶Corresponding series of fetal SVT (n=23).
†It was only possible for the authors to to evaluate the success rate for digoxin treatment in 10 cases.
‡Completed by published18,19 and unpublished data.
AF, atrial flutter; D, digoxin; GA, gestational age; SVT, supraventricular tachycardia.
Figure 1.
Analysis of gestational age at diagnosis of fetal atrial flutter and supraventricular tachycardia. Test for heterogeneity: χ2 = 14.29, df = 8, p = 0.075. Test for overall effect: z = 4.94, p < 0.00001. AF, atrial flutter; CI, confidence interval, GA, gestational age; SVT supraventricular tachycardias; WMD, weighted mean differences.
AV block
In five studies, 2:1 AV block was observed in 83.0% (range 66.7–100%) of all cases with atrial flutter (39 of 47 cases).1,5,8,11,12 Data obtained from studies by Jaeggi and colleagues and Krapp and associates showed that fetuses with 2:1 AV block were not detected earlier in pregnancy than fetuses with higher degrees of AV block (p = 0.7).1,12 Both groups of fetuses were detected significantly later in pregnancy than fetuses with SVT (p = 0.00003 and 0.002, respectively). Of the 39 fetuses with atrial flutter and 2:1 block, 17 (43.6%) were hydropic, whereas in the remaining eight fetuses with higher degrees of AV block only two had signs of hydrops. The numbers of fetuses in these studies were too small to use statistical tests. In one study it was possible to retrieve additional data for separate statistical analysis.2 The ventricular rate was available in 25 fetuses and the atrial rate in 18. Hydropic fetuses had higher ventricular rates (median 240 beats/min, range 240–300) than non-hydropic fetuses (median 220 beats/min, range 200–310) (p = 0.02), whereas the atrial rates were not significantly different (median 450 beats/min, range 370–500).
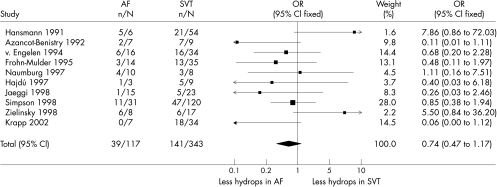
Hydrops fetalis
Hydrops fetalis was reported in 49 of 127 fetuses with atrial flutter (38.6%) and in 141 of 348 fetuses with SVT (40.5%) (table 1).1,2,4–12 There was no significant difference between atrial flutter and SVT in the occurrence of hydrops fetalis (OR 0.74, 95% CI 0.47 to 1.17; p = 0.2) (fig 2).
Figure 2.
Analysis of the occurrence of hydrops fetalis in atrial flutter and supraventricular tachycardia. Test for heterogeneity: χ2 = 15.90, df = 9, p = 0.069. Test for overall effect: z = 1.28, p = 0.2. AF, atrial flutter; CI, confidence interval, GA, gestational age; OR, odds ratio; SVT supraventricular tachycardias.
Intrauterine treatment
In 67.6% of cases with fetal atrial flutter (75 of 111 fetuses) in the publications reviewed, digoxin was used as first line treatment (table 1).1,2,4,5,7–12 In nine of the 11 studies, conversion to sinus rhythm was reported in 32 of 71 cases (45.1%) with digoxin treatment alone (table 1).1,2,4,5,7,8,10–12 In six studies it was possible to compare the success rate of digoxin treatment in fetuses with hydrops (6.3%, one of 16 cases) and in fetuses without hydrops (51.7%, 15 of 29 cases).1,4,5,7,10,11 This trend just failed to reach significance (OR 0.22, 95% CI 0.05 to 1.02; p = 0.05) because of the relatively small numbers in this group.
In 63.4% of the reported cases with fetal SVT in the publications reviewed (199/314), digoxin was used as first line treatment (table 1).2,4,5,7,9–13 The conversion rate to sinus rhythm with digoxin alone was reported as 51.5% (102 of 198 cases) in eight of the 11 studies (table 1).2,4,5,7,10–13 In eight studies it was possible to compare the success rate of digoxin treatment in fetuses with hydrops (24.6%) and without hydrops (65.4%).2,4,5,7,10–13 There was a significantly higher conversion rate in the fetuses without hydrops (OR 0.19, 95% CI 0.09 to 0.41; p < 0.001). There was no difference in the success rate of digoxin in atrial flutter and SVT (p = 0.36). Combining the data from all fetuses with atrial flutter and SVT, digoxin treatment alone converted non-hydropic fetuses better than hydropic fetuses (63.3% v 19.5%; OR 0.18, 95% CI 0.10 to 0.34; p < 0.001).1,2,4–7,10–13
In fetal atrial flutter, second line treatment with a wide range of different antiarrhythmic agents (quinidine, sotalol, amiodarone, propafenone, flecainide, verapamil, procainamide) was reported in six studies.4,5,7,10–12 Flecainide, amiodarone, and propafenone were used most often, with conversion rates of 5/6, 3/7, and 1/3, respectively.
Second line treatment was reported in eight studies with fetal SVT.2,4,5,7,10–13 Digoxin combined with flecainide, verapamil, amiodarone, or propafenone was used, with conversion rates of 9/11, 3/9, 2/2, and 0/2, respectively. Single second line treatments included flecainide, sotalol, diuretics (not specified), or verapamil, with conversion rates of 9/10, 5/6, 2/2, and 0/1, respectively.
In some studies antiarrhythmic drugs were given by cordocentesis in hydropic fetuses.2,4,6,11–13 These included amiodarone, adenosine, propafenone, diuretics (not specified), and procainamide, with conversion rates of 9/14, 0/5, 2/2, 2/2, and 0/1, respectively.
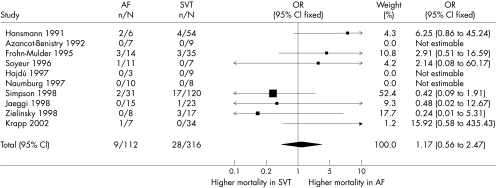
Mortality
Ten of the 11 papers reported differentiated mortality; the rates were 8.0% (nine of 112 cases) in atrial flutter and 8.9% (28 of 316 cases) in SVT.1,2,4,5,7–13 There was no significant difference between these rates (p = 0.7) (fig 3). In seven papers the presence of hydrops was mentioned in five of the six fetuses with atrial flutter and in all 10 fetuses with SVT who died postnatally.1,2,4,7,11–13 In one of five cases of atrial flutter and in 15 of 25 cases of SVT the fetus died prenatally. Analysing the data of Jaeggi and colleagues and Krapp and associates,1,12 we were not able to verify any difference in mortality between fetuses with 2:1 AV block (0/16) and fetuses with higher degrees of AV block (1/16) (p = 0.2). Furthermore, there was no difference in the mortality of these two groups compared with fetuses with SVT (1/57) (p = 0.4 and 0.16, respectively).
Figure 3.
Analysis of mortality in fetuses and neonates with atrial flutter and supraventricular tachycardia. Test for heterogeneity: χ2 = 9.35, df = 6, p = 0.15. Test for overall effect: z = 0.42, p = 0.7. AF, atrial flutter; CI, confidence interval, GA, gestational age; OR, odds ratio; SVT supraventricular tachycardias.
Association with congenital heart defects
Nine papers reported the presence and type of cardiac malformations associated with fetal atrial flutter and SVT.1,5,6,8–13 Atrial flutter was associated with atrioventricular septal defect (n = 5), hypoplastic left heart syndrome (n = 1), and pulmonary atresia (n = 1) in some fetuses.1,6,12 SVT was associated with Ebstein’s anomaly (n = 2) and ventricular septal defect (n = 2).11
Outcome
At birth 50% of fetuses with atrial flutter (23 of 46) were in sinus rhythm1,5,10–12 compared with 71.4% of fetuses with SVT (65 of 91).5,10–13 Because of the small numbers this difference was not significant.
In 14 of 23 cases with persistent atrial flutter at birth, follow up during the neonatal period was reported.1,11,12 Successful conversion to sinus rhythm was achieved postnatally by electrical conversion in six cases, by digoxin in three, by sotalol/digoxin in two, by flecainide in one, and by amiodarone/digoxin in one. One neonate died from necrotising enterocolitis before sinus rhythm was established.
In 18 of 26 cases with persistent SVT at birth, follow up during the neonatal period was reported.10–12 Successful conversion to sinus rhythm was achieved postnatally by electrical conversion in two cases, by digoxin in seven, by propafenone in five, by digoxin/propranolol in two, by propranolol in one, and with no treatment in one.
DISCUSSION
Population
The mean gestational age at diagnosis in fetuses with SVT differed significantly from that in fetuses with atrial flutter. In the largest multicentre study on fetal atrial flutter, which included 44 prenatally diagnosed cases of atrial flutter from four centres, the mean (SD) gestational age was 32.4 (5.16) weeks,20 which is comparable to our review (range of mean gestational ages 30.7–34.4 weeks). Experimental observations and the fact that atrial flutter occurs mainly during the third trimester support the hypothesis of atrial macroreentry as the underlying mechanism of fetal atrial flutter. The atrium probably reaches a critical size for establishing an intra-atrial macroreentry circuit at about 27–30 weeks of gestation, associated with a high vulnerability for triggering atrial extrasystoles.1 In some fetuses with atrial flutter, the presence of an accessory AV pathway has been demonstrated by postnatal transoesophageal electrophysiological studies in the neonatal period.21
It might be argued that the onset of atrial flutter does not occur later than SVT, but simply that the diagnosis of atrial flutter is delayed owing to difficulties in the recognition of this arrhythmia when there is a high degree of AV block. In our study, however, fetuses with a 2:1 AV block were not detected earlier in pregnancy than fetuses with higher degrees of AV block. This finding provides support for a genuinely later onset of atrial flutter in pregnancy.
Atrial dilatation resulting from severe AV valve regurgitation in rare cases of Ebstein’s anomaly and atrioventricular septal defect sometimes causes fetal atrial flutter. This is analogous to the well known finding of atrial flutter associated with left atrial dilatation caused by mitral valve dysfunction in later life.22 The findings of our study were consistent with this, in that an atrioventricular septal defect was present in five of seven fetuses with atrial flutter and a cardiac malformation.
AV blockade
There is a 2:1 AV block in over 80% of cases of fetal atrial flutter. The AV node, which is not part of the intra-atrial reentrant circuit, protects the ventricles in atrial flutter by variably blocking AV conduction, thus causing a substantially slower fixed or variable ventricular rate, depending on the degree of AV block. One study group in our review, who provided extended data on their patient cohort, was able to show that the ventricular rate of hydropic fetuses with atrial flutter was higher than in non-hydropic fetuses.2
Hydrops fetalis
Fetal hydrops was present in 38.6% of all fetuses with atrial flutter (49 of 127 cases; table 1), compared with 45.5% (20 of 44) reported by Lisowksi and colleagues.20 This discrepancy may reflect local differences in fetal screening programmes and referral patterns. Hydrops fetalis was present in 40.5% of all fetuses with SVT (141 of 348 cases; table 1). There was no significant difference in the incidence of hydrops between the atrial flutter and SVT groups in this review.
Intrauterine treatment
Digoxin was used as first line treatment in 67.0% of cases of fetal atrial flutter (table 1), compared with 47.7% in the multicentre study by Lisowski and colleagues.20 Our review (table 1) and the article of Lisowski and colleagues showed similar conversion rates of 45.1% and 52.4%, respectively, with digoxin alone. Lisowski reported a success rate of 43.8% in hydropic fetuses and 80% in non-hydropic fetuses, whereas in our review the conversion rates were 6.3% in hydropic fetuses and 51.7% in non-hydropic fetuses. This trend almost reached significance (p = 0.05). Digoxin treatment was significantly more successful in non-hydropic fetuses with SVT and in all non-hydropic fetuses with tachyarrhythmias. In this review we were able to prove the hypothesis of better conversion rates of digoxin treatment in non-hydropic fetuses. Digoxin may be useful for its positive inotropic and negative chronotropic properties.1 In our review, only Simpson and colleagues2 and Naumburg and colleagues10 used different treatment schemes as first line treatment (digoxin + verapamil and flecainide) in a few hydropic cases. Other clinicians preferred prompt delivery followed by cardioversion in viable fetuses.1,20 Oudijk and colleagues reported 21 fetuses with tachyarrhythmia treated by sotalol in a multicentre study.23 There were 10 cases with SVT, 10 with atrial flutter, and one with ventricular tachycardia. Intrauterine mortality was 30% (3/10) in the fetuses with SVT and 10% (1/10) in the fetuses with atrial flutter. They therefore suggested the use of sotalol only for fetuses with atrial flutter, because of the proarrhythmic effects of sotalol in the fetal heart. Lisowski and colleagues used sotalol alone or combined with digoxin in 14 of 44 fetuses with atrial flutter.20 There was one intrauterine death within 24 hours after a dose increase, which could have resulted from the proarrhythmic effect of sotalol.
In fetal SVT, digoxin was used in 63.4% of cases as first line treatment. The success rate was similar to atrial flutter. Flecainide alone or in combination with digoxin was most often used as second line treatment, with a success rate of 86.7%.
In the CAST (cardiac arrhythmia suppression trial) study, proarrhythmic effects and ventricular tachycardia were demonstrated, with increased mortality in men after myocardial infarction.24 There is one reported case of intrauterine fetal death after three days of transplacental flecainide treatment.25 The investigators discussed the possibility of a proarrhythmic effect of flecainide in this case, but the fetus had died within 24 hours after cordocentesis. Simpson and colleagues reported three cases of intrauterine fetal death within 24 hours of the introduction of flecainide.2 Although it is difficult to draw conclusions about a potentially adverse effect of flecainide in this population of fetuses at increased risk of prenatal demise, the occurrence of fetal death within 24 hours of the initiation of flecainide raises the question of a proarrhythmic effect of this drug. We therefore always use digoxin in combination with flecainide, which may protect the fetus from adverse effects of flecainide while potentiating the converting effects of this agent.25
Mortality
The overall mortality of fetal atrial flutter was 8.0% (table 1), comparable with the figure of 6.8% in the study by Lisowski and colleagues.20 Twenty per cent of the deaths from atrial flutter occurred prenatally, compared with 60% of the deaths from SVT. Mortality in fetal SVT was 8.9%, which was not significantly different from atrial flutter. This contrasts with the view that fetal atrial flutter has a worse prognosis than fetal SVT because of difficulties in controlling atrial flutter in utero and the high incidence of associated congenital cardiac malformations.3 Lisowski reported 45 fetuses with atrial flutter, of whom only one had a cardiac malformation.20
Postnatal treatment
Postnatally, fetal atrial flutter can be controlled by various antiarrhythmic drugs such as digoxin, sotalol, amiodarone, or flecainide, and by direct current cardioversion.1,11,12 Spontaneous termination of atrial flutter may occur directly after birth. When sinus rhythm has been established, recurrence of atrial flutter is rare.1 Therefore a wait and see policy is justifiable.26 According to Naumburg and colleagues, there may be late recurrences.10 These investigators therefore recommend a follow up period of at least six months.10 Alternatively, prophylactic antiarrhythmic treatment beyond the neonatal period may be prolonged for 6–12 months.1,20
Conclusions
Fetal atrial flutter is the second most common tachyarrhythmia. The detection or onset of this arrhythmia is about two weeks later than SVT with 1:1 AV conduction. Overall, fetal atrial flutter has the same outcome as SVT, but atrial flutter with higher degrees of AV block seems to have a better prognosis than fetal SVT with 1:1 AV conduction or atrial flutter with 2:1 AV block.
Successful treatment of non-hydropic fetuses with atrial flutter can be achieved with digoxin alone in 50–55% of cases. If atrial flutter persists, close intrauterine follow up and postnatal conversion may be preferred in these non-hydropic cases, rather than starting second line intrauterine antiarrhythmic drug treatment. In hydropic fetuses digoxin treatment is associated with a low conversion rate. Thus intrauterine treatment with digoxin combined with flecainide, sotalol, or amiodarone, respectively, is required as first line treatment.1,20 Sotalol and flecainide may have proarrhythmic effects in fetuses with atrial flutter and SVT, respectively. According to published reports, sotalol should be restricted to fetuses with atrial flutter,23 whereas in fetal SVT flecainide may have a major role.12 The end point of intrauterine treatment should be the restoration of sinus rhythm and not merely the reduction of ventricular rate by increasing the degree of AV blockade. In hydropic fetuses with treatment-refractory atrial flutter who are too immature to benefit from premature delivery, transoesophageal overdrive stimulation by a percutaneous fetoscopic technique may become an option in the future.27 Premature delivery and postnatal conversion to sinus rhythm should be restricted to hydropic fetuses at late gestation (more than 34 weeks) with treatment-refractory atrial flutter with 2:1 block.
REFERENCES
- 1.Jaeggi E, Fouron JC, Drblik SP. Fetal atrial flutter: diagnosis, clinical features, treatment, and outcome. J Pediatr 1998;132:335–9. [DOI] [PubMed] [Google Scholar]
- 2.Simpson JM, Sharland GK. Fetal tachycardias: management and outcome of 127 consecutive cases. Heart 1998;79:576–81. [PMC free article] [PubMed] [Google Scholar]
- 3.Kleinman CS, Nehgeme R, Copel JA. Fetal cardiac arrhythmias: diagnosis and therapy. In: Creasy RK, Resnik R, eds. Maternal-fetal medicine, 4th ed. Philadelphia: WB Saunders Co, 1999:301–18.
- 4.Hansmann M, Gembruch U, Bald R, et al. Fetal tachyarrhythmias: transplacental and direct treatment of the fetus – a report of 60 cases. Ultrasound Obstet Gynecol 1991;1:162–70. [DOI] [PubMed] [Google Scholar]
- 5.Azancot-Benistry A, Jacqz-Aigrain E, Guirgis NM, et al. Clinical and pharmacologic study of fetal supraventricular tachyarrhythmias. J Pediatr 1992;121:608–13. [DOI] [PubMed] [Google Scholar]
- 6.van Engelen AD, Weijtens O, Brenner JI, et al. Management, outcome and follow-up of fetal tachyarrhythmia. J Am Coll Cardiol 1994;24:1371–5. [DOI] [PubMed] [Google Scholar]
- 7.Frohn-Mulder IM, Stewart PA, Witsenburg M, et al. The efficacy of flecainide versus digoxin in the management of fetal supraventricular tachycardia. Prenat Diagn 1995;15:1297–302. [DOI] [PubMed] [Google Scholar]
- 8.Soyeur D. Atrial flutter in the human fetus: diagnosis, hemodynamic consequences, and therapy. J Cardiovasc Electrophysiol 1996;7:989–99. [DOI] [PubMed] [Google Scholar]
- 9.Hajdu J, Szabo I, Papp C, et al. [Treatment of haemodynamically significant fetal arrhythmias]. Orv Hetil 1997;138:2335–8. [PubMed] [Google Scholar]
- 10.Naumburg E, Riesenfeld T, Axelsson O. Fetal tachycardia: intrauterine and postnatal course. Fetal Diagn Ther 1997;12:205–9. [DOI] [PubMed] [Google Scholar]
- 11.Zielinsky P, Dillenburg RF, de Lima GG, et al. [Fetal supraventricular tachyarrhythmias. Experience of a fetal cardiology reference centre]. Arq Bras Cardiol 1998;70:337–40. [DOI] [PubMed] [Google Scholar]
- 12.Krapp M, Baschat AA, Gembruch U, et al. Flecainide in the intrauterine treatment of fetal supraventricular tachycardia. Ultrasound Obstet Gynecol 2002;19:158–64. [DOI] [PubMed] [Google Scholar]
- 13.Jaeggi E, Fouron JC, Fournier A, et al. Ventriculo-atrial time interval measured on M mode echocardiography: a determining element in diagnosis, treatment, and prognosis of fetal supraventricular tachycardia. Heart 1998;79:582–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maragnés P, Fournier A, Lessard M, et al. [Evaluation and prognosis of fetal arrhythmia]. Pediatrie 1991;46:481–8. [PubMed] [Google Scholar]
- 15.Maxwell DJ, Crawford DC, Curry PVM, et al. Obstetric importance, diagnosis, and management of fetal tachycardias. BMJ 1988;297:107–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Allan LD, Chita SK, Sharland GK, et al. Flecainide in the treatment of fetal tachycardias. Br Heart J 1991;65:46–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stewart PA, Wladimiroff JW. Cardiac tachyarrhythmia in the fetus: diagnosis, treatment and prognosis. Fetal Ther 1987;2:7–16. [DOI] [PubMed] [Google Scholar]
- 18.Gembruch U, Krapp M, Baumann P. Changes of venous blood flow velocity waveforms in fetuses with supraventricular tachycardia. Ultrasound Obstet Gynecol 1995;5:395–9. [DOI] [PubMed] [Google Scholar]
- 19.Gembruch U, Krapp M, Germer U, et al. Venous Doppler in the sonographic surveillance of fetuses with supraventricular tachycardia. Eur J Obstet Gynecol Reprod Biol 1999;84:187–92. [DOI] [PubMed] [Google Scholar]
- 20.Lisowski LA, Verheijen PM, Benatar AA, et al. Atrial flutter in the perinatal age group: diagnosis, management and outcome. J Am Coll Cardiol 2000;35:771–7. [DOI] [PubMed] [Google Scholar]
- 21.Naheed ZJ, Strasburger JF, Deal BJ, et al. Fetal tachycardia: mechanisms and predictors of hydrops fetalis. J Am Coll Cardiol 1996;27:1736–40. [DOI] [PubMed] [Google Scholar]
- 22.Gembruch U, Hansmann M, Bald R. [Fetal atrial flutter in complete atrioventricular canal and trisomy 18]. Geburtshilfe Frauenheilk 1988;48:445–7. [DOI] [PubMed] [Google Scholar]
- 23.Oudijk MA, Michon MM, Kleinman CS, et al. Sotalol in the treatment of fetal dysrhythmias. Circulation 2000;101:2721–6. [DOI] [PubMed] [Google Scholar]
- 24.Echt DS, Liebson PR, Mitchell LB, et al. Mortality and morbidity in patients receiving encainide, flecainide, or placebo. The cardiac arrhythmia suppression trial. N Engl J Med 1991;324:781–8. [DOI] [PubMed] [Google Scholar]
- 25.Allan LD, Chita SK, Sharland GK, et al. Flecainide in the treatment of fetal tachycardias. Br Heart J 1991;65:46–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dunnigan A, Benson WD, Benditt DG. Atrial flutter in infancy: diagnosis, clinical features and treatment. Pediatrics 1985;75:725–9. [PubMed] [Google Scholar]
- 27.Kohl T, Kirchhof PF, Gogarten W, et al. Fetoscopic transesophageal electrocardiography and stimulation in fetal sheep: a minimally invasive approach aimed at diagnosis and termination of therapy–refractory supraventricular tachycardias in human fetuses. Circulation 1999;100:772–6. [DOI] [PubMed] [Google Scholar]