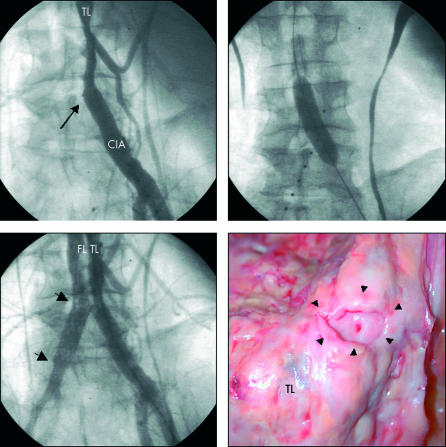
A 61 year old man with a history of systemic hypertension was admitted with severe chest and back pain of acute onset. Contrast enhanced computed tomography (CT) revealed acute Stanford type B aortic dissection extending to the iliac arteries. The patient was initially stabilised by intravenous antihypertensive medication, but soon developed critical right sided limb ischaemia. For restoration of perfusion, percutaneous balloon fenestration was considered. Angiography showed complete occlusion of the right common iliac artery (CIA) at the level of the aortic bifurcation (arrow; upper panel, left; TL, true lumen). The intimal flap was punctured from the true lumen using a Brockenborough needle and a guide wire was passed into the false lumen. A balloon with a diameter of 14 mm was used to enlarge the puncture site within the intimal flap (upper panel, right). Although aortography demonstrated communication between true and false lumen, flow into the right common iliac artery remained impaired. Additional stent placement (arrows) into the right common iliac artery was required to re-establish limb perfusion (lower panel, left; FL, false lumen). Following the procedure, the patient developed reperfusion syndrome with a maximal myoglobin of 155 742 μg/l requiring transient haemodialysis.
After recovery of the patient, endovascular stent–graft placement was performed to seal the proximal entry tear in the thoracic aorta. The patient was finally discharged six months after the initial event. However, he died from septic complications six weeks after discharge. At necropsy, the large tear in the intimal flap created by balloon fenestration could be seen (arrows; lower panel, right).