Abstract
Background: Traditional cardiovascular risk factors have been associated with aortic stenosis and coronary artery disease. As these two conditions often co-exist, the association of cardiovascular risk factors with aortic stenosis may reflect confounding.
Objective: To compare the cardiovascular risk profile in patients with severe aortic stenosis undergoing elective coronary angiography with that of patients without aortic stenosis or calcification undergoing coronary angiography for suspected coronary artery disease.
Methods: 523 patients referred for elective diagnostic left heart catheterisation because of severe aortic stenosis formed the case population; 3925 patients without valve disease referred for elective diagnostic left heart catheterisation formed the base control population. Of the latter, 523 were pair matched to the case population for sex, age, and prevalence of relevant coronary artery disease, forming a pair matched control population. Cardiovascular risk factors (male sex, hypertension, hypercholesterolaemia, smoking, diabetes mellitus, family history of coronary artery disease) were assessed in all the patients.
Results: None of the cardiovascular risk factors was more prevalent in patients with aortic stenosis than in the base control population or in the pair matched control population. However, male sex, hypercholesterolaemia, smoking, diabetes mellitus, and a family history of coronary artery disease were significantly associated with the presence of additional coronary artery disease in patients with aortic stenosis.
Conclusions: Cardiovascular risk factors are commonly present in patients with aortic stenosis. However, when compared with controls matched for age, sex, and angiographically defined coronary artery disease, no risk factor was significantly associated with the prevalence of aortic stenosis. Thus other factors are likely to be more important in the pathogenesis of aortic stenosis.
Keywords: aortic stenosis, risk factors, coronary artery disease
Generally accepted cardiovascular risk factors for coronary artery disease are age, hypertension, hypercholesterolaemia, smoking, and diabetes mellitus.1,2 Calcific aortic stenosis is the most frequent acquired valvar disease and has a serious prognosis when it becomes symptomatic.3 Calcific aortic stenosis and coronary artery disease share many similarities. Both increase in prevalence with age, but they are not simply a normal consequence of aging.4,5
Calcific aortic stenosis is associated with the same risk factors as coronary artery disease.4,6,7 Furthermore aortic sclerosis is itself associated with a 50% increased risk of cardiovascular mortality and myocardial infarction.8 The large cardiovascular health study (CHS) showed that raised serum cholesterol is associated with the presence of aortic valve disease.4 Recent smaller studies have provided evidence of the importance of high concentrations of low density lipoprotein (LDL) cholesterol for the development of aortic stenosis,9 and lowering LDL cholesterol with statins might be an option to retard the progression of this disease.10 However, despite their similarities the two diseases are likely to have a different pathogenesis.
Aortic stenosis and coronary artery disease often co-exist, so an association of cardiovascular risk factors with aortic stenosis might be confounded by this association. Moreover, influences other than cardiovascular risk factors—genetic11,12 or inflammatory,11,13 for example—could trigger the pathogenesis of aortic stenosis. Most earlier studies4–7,9 have lacked coronary angiographic data in control patients and thus the prevalence of coincidental coronary artery disease may have been underestimated.
Our hypothesis in this study was that cardiovascular risk factors may be associated with aortic stenosis because of their confounding association with coronary artery disease. We therefore compared the cardiovascular risk profile in patients with severe aortic stenosis undergoing elective diagnostic coronary angiography with that in patients without aortic stenosis or calcification who were undergoing elective diagnostic coronary angiography for suspected coronary artery disease.
METHODS
Study population
Within an area of approximately 300 000 inhabitants, the study centre is the only reference centre undertaking coronary angiography. Consecutive patients with calcific aortic stenosis formed the case population. Inclusion criteria were first elective diagnostic coronary angiography and an invasively determined mean gradient across the aortic valve of ⩾ 40 mm Hg. Exclusion criteria were mild or moderate aortic stenosis, severe aortic regurgitation, or other relevant valvar disease. In all, 523 patients fulfilled these criteria and formed the case population.
Consecutive patients with clinically suspected coronary artery disease referred for coronary angiography formed the control population. Inclusion criteria were first elective diagnostic coronary angiography and a normal aortic valve on fluoroscopy. Exclusion criteria were known valvar disease, calcification of the aortic valve on fluoroscopy, and a gradient of more than 5 mm Hg across the aortic valve during left heart catheterisation. In all, 3925 patients fulfilled these criteria. From this control population, 523 patients were pair matched for age, sex, and the presence of coronary artery disease and formed the matched control population.
All patients gave their written informed consent. The study was approved by the local ethics committee of the University Hospital of Aachen.
Left heart catheterisation
Coronary angiography, including at least four views of each coronary artery, was carried out in all patients. Coronary angiograms were classified as showing either no significant coronary artery disease—that is, clear coronary arteries or coronary sclerosis (signs of atherosclerosis with stenosis less than 50%)—or definite coronary artery disease (stenosis greater than 50% in at least one vessel). The gradient across the aortic valve was measured by pull back of the catheter from the left ventricle into the ascending aorta. The mean gradient was calculated by a computer assisted program (Metek, Roetgen, Germany).
Cardiovascular risk factors
Cardiovascular risk factors were as follows:
hypercholesterolaemia: serum cholesterol > 5.2 mmol/l (200 mg/dl) or medically treated
arterial hypertension: blood pressure > 140/90 mm Hg or medically treated
diabetes mellitus: overnight fasting serum glucose > 7.0 mmol/l (126 mg/dl) on at least two occasions or medically treated
smoking: regular smoking habit
positive family history of coronary artery disease: a first degree relative with known coronary artery disease at any age.
Data collection
The cardiovascular risk profile was assessed by physicians unaware of the study, and data were added to the computer record of the individual patient before angiography was done. Angiograms were interpreted by two experienced physicians.
Statistical analysis
Continuous data are presented as mean (SD), and qualitative data as frequencies. Differences between frequencies of cardiovascular risk factors were assessed by cross tabulation χ2 analysis. For estimation of chance, the odds ratios for single cardiovascular risk factors were calculated by χ2 analysis. Calculations were done using SPSS for windows, version 10.0. Significant differences were defined as a probability value of p < 0.05.
RESULTS
Cardiovascular risk factors of unmatched case and control populations
As shown in table 1, the patients referred for coronary angiography because of severe aortic stenosis were significantly older than those referred for coronary angiography for isolated coronary artery disease. Male sex, hypercholesterolaemia, smoking, and a family history of coronary artery disease were less often present in patients with aortic stenosis than in the those with normal aortic valves in the unmatched control population.
Table 1.
Traditional cardiovascular risk factors in patients with severe aortic stenosis and in controls with normal aortic valves (not matched)
| Severe aortic stenosis | Normal aortic valve | p Value | Odds ratio (95% CI) | |
| n | 523 | 3925 | ||
| Age (years) (mean (SD)) | 70 (8) | 61 (11) | <0.001 | |
| Clear coronaries or coronary sclerosis | 246 (47%) | 1426 (36%) | ||
| Stenosis of >50% in at least one coronary vessel | 277 (53%) | 2499 (64%) | ||
| Cardiovascular risk factors | ||||
| Male sex | 287 (55%) | 2642 (67%) | 0.001 | 0.59 (0.49 to 0.71) |
| Hypertension | 308 (59%) | 2282 (58%) | 0.777 | 1.03 (0.86 to 1.24) |
| Hypercholesterolaemia | 258 (49%) | 2623 (67%) | 0.001 | 0.49 (0.40 to 0.58) |
| Smoking | 213 (41%) | 1807 (46%) | 0.022 | 0.81 (0.67 to 0.97) |
| FH of coronary artery disease | 144 (28%) | 1289 (33%) | 0.015 | 0.78 (0.63 to 0.95) |
| Diabetes mellitus | 106 (20%) | 699 (18%) | 0.183 | 1.17 (0.93 to 1.47) |
Values are n (%) unless stated.
CI, confidence interval; FH, family history.
Cardiovascular risk factors of case and pair matched control populations
Comparing the cardiovascular risk profile of patients with severe aortic stenosis and pair matched controls (matched for sex, age, and the presence of coronary artery disease), patients with severe aortic stenosis but without relevant coronary artery disease less often had hypercholesterolaemia (p = 0.001) (table 2, upper part). In patients with severe aortic stenosis and coronary artery disease, the cardiovascular risk profile was similar to the controls apart from a slightly higher prevalence of a positive family history of coronary artery disease (p = 0.014) (table 2, lower part).
Table 2.
Traditional cardiovascular risk factors in patients with severe aortic stenosis and controls with normal aortic valves (pair matched for age, sex, and the presence of stenotic coronary artery disease on angiography)
| Severe aortic stenosis without CAD | Normal aortic valve without CAD | p Value | Odds ratio (95% CI) | |
| n | 246 | 246 | ||
| Male sex* | 98 (40%) | 98 (40%) | ||
| Age (years)* (mean (SD)) | 69 (8) | 69 (8) | ||
| Cardiovascular risk factors | ||||
| Hypertension | 136 (55%) | 154 (63%) | 0.119 | 0.74 (0.52 to 1.06) |
| Hypercholesterolaemia | 94 (40%) | 142 (58%) | 0.001 | 0.45 (0.32 to 0.65) |
| Smoking | 80 (33%) | 61 (25%) | 0.072 | 1.46 (0.98 to 2.16) |
| FH of CAD | 52 (21%) | 60 (24%) | 0.452 | 0.83 (0.55 to 1.27) |
| Diabetes mellitus | 39 (16%) | 39 (16%) | 1.000 | 1.00 (0.62 to 1.62) |
| Severe aortic stenosis with CAD | Normal aortic valve with CAD | |||
| Values are n (%) unless stated. | ||||
| *Matched. | ||||
| CAD, coronary artery disease; CI, confidence interval; FH, family history. | ||||
| n | 277 | 277 | ||
| Male sex* | 189 (68%) | 189 (68*) | ||
| Age (years)* (mean (SD)) | 70 (7) | 70 (7) | ||
| Cardiovascular risk factors | ||||
| Hypertension | 172 (62%) | 174 (63%) | 0.930 | 0.97 (0.69 to 1.36) |
| Hypercholesterolaemia | 164 (59%) | 167 (60%) | 0.862 | 0.96 (0.68 to 1.34) |
| Smoking | 133 (48%) | 117 (42%) | 0.200 | 1.26 (0.90 to 1.76) |
| FH of CAD | 92 (33%) | 65 (24%) | 0.014 | 1.62 (1.12 to 2.36) |
| Diabetes mellitus | 67 (24%) | 56 (20%) | 0.307 | 1.26 (0.84 to 1.88) |
Cardiovascular risk factors and prevalence of coronary artery disease in patients with severe aortic stenosis
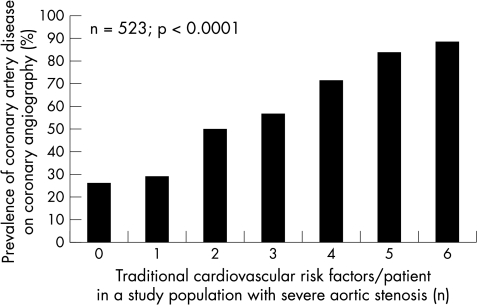
Male sex, hypercholesterolaemia, smoking, diabetes mellitus, and a family history of coronary artery disease were significantly associated with the presence of coronary artery disease in patients with severe aortic stenosis (table 3). There was only a trend for hypertension to be more frequent in patients with coronary artery disease (p = 0.131). As shown in fig 1, traditional cardiovascular risk factors had an additive effect, with the lowest prevalence of coronary artery disease in patients without these risk factors and the highest prevalence in patients with all six cardiovascular risk factors (p < 0.0001).
Table 3.
Traditional cardiovascular risk factors in patients with severe aortic stenosis with and without coronary artery disease
| Severe aortic stenosis without CAD | Severe aortic stenosis with CAD | p Value | Odds ratio (95% CI) |
|
| n | 246 | 277 | ||
| Age (years) (mean (SD)) | 69 (8) | 70 (7) | ||
| Cardiovascular risk factors | ||||
| Male sex | 98 (40%) | 189 (68%) | <0.001 | 3.24 (2.26 to 4.65) |
| Hypertension | 136 (55%) | 172 (62%) | 0.131 | 1.32 (0.93 to 1.88) |
| Hypercholesterolaemia | 94 (40%) | 164 (59%) | <0.001 | 2.35 (1.65 to 3.34) |
| Smoking | 80 (33%) | 133 (48%) | <0.001 | 1.92 (1.34 to 2.74) |
| FH of CAD | 52 (21%) | 92 (33%) | 0.002 | 1.86 (1.25 to 2.76) |
| Diabetes mellitus | 39 (16%) | 67 (24%) | 0.022 | 1.69 (1.09 to 2.63) |
Values are n (%) unless stated.
CAD, coronary artery disease; CI, confidence interval; FH, family history.
Figure 1.
Relation between total number of traditional cardiovascular risk factors per patient (male sex, hypertension, hypercholesterolaemia, smoking, diabetes mellitus, and family history of coronary artery disease) and the prevalence of stenotic coronary artery disease on angiography (diameter stenosis > 50% in at least one vessel).
DISCUSSION
Male sex, hypertension, hypercholesterolaemia, smoking, diabetes mellitus, and a family history of the condition are established risk factors for coronary artery disease.1,2 A large echocardiographic study showed that the risk factors associated with the prevalence of aortic sclerosis and aortic stenosis were similar.4 However, because of the strong linkage between aortic stenosis and coronary artery disease,8 these risk factors may not be related to calcification of the aortic valve but rather to atherosclerosis of the coronary arteries. It is possible that cardiovascular risk factors are associated with aortic stenosis purely because of an association between aortic stenosis and coronary artery disease. Thus, when defining risk factors for aortic stenosis, it is essential to control for atherosclerosis of the coronary arteries.
Our major finding in this study was that none of the traditional cardiovascular risk factors was more prevalent in patients with severe aortic stenosis than in controls. However, cardiovascular risk factors predicted the presence of coronary artery disease in patients with severe aortic stenosis. This finding may indicate that traditional cardiovascular risk factors are associated with aortic stenosis purely on the basis of its link with coronary artery disease.
In this study population there was a lower prevalence of hypercholesterolaemia in patients with aortic stenosis than in those without aortic stenosis. This is of particular interest because there is evidence for an association between serum cholesterol concentrations and calcification of the aortic valve.9,10 Despite the fact that most patients with hypercholesterolaemia do not develop aortic stenosis, cholesterol may be of special importance for calcification in that valve. However, the simple presence of this cardiovascular risk factor does not seem to be a reliable predictor of severe aortic stenosis. Other mechanisms might be important for deposition of cholesterol in the aortic valve. For example, a case report in 1993 described a family with immunological abnormalities and severe aortic valve calcification.11 Furthermore it is known that stenotic aortic valves contain infiltrates of macrophages and T lymphocytes as well as an accumulation of plasma lipoproteins.14,15 Genetic factors and inflammation may be key factors in the initiation and progression of aortic stenosis.
Our study cannot fully prove that cardiovascular risk factors are not involved in the pathogenesis of aortic stenosis, but the study showed that many patients with the same burden of cardiovascular risk factors as patients with aortic stenosis have normal aortic valves, whereas the association of cardiovascular risk factors with coronary artery disease remains strong, and in patients with severe aortic stenosis cardiovascular risk factors are highly predictive of the presence of coronary artery disease.
We conclude that further studies are necessary to clarify the pathogenesis of aortic stenosis. Assessment of cardiovascular risk factors alone is not sufficient to identify the mechanisms of valve calcification, and further factors need to be considered.
REFERENCES
- 1.Kannel WB, Dawber TR, Kagan A, et al. Factors of risk in the development of coronary heart disease – six year follow up experience: the Framingham study. Ann Intern Med 1961;55:33–50. [DOI] [PubMed] [Google Scholar]
- 2.Kannel WB, Wilson PW. An update on coronary risk factors. Med Clin North Am 1995;79:951–71. [DOI] [PubMed] [Google Scholar]
- 3.Ross J, Braunwald E. Aortic stenosis. Circulation 1968;38(suppl 1): 61–7. [DOI] [PubMed] [Google Scholar]
- 4.Stewart BF, Siscovick D, Lind BK, et al. Clinical factors associated with calcific aortic valve disease. J Am Coll Cardiol 1997;29:630–4. [DOI] [PubMed] [Google Scholar]
- 5.Lindroos M, Kupari M, Heikkila J, et al. Prevalence of aortic valve abnormalities in the elderly: an echocardiographic study of a random population sample. J Am Coll Cardiol 1993;21:1220–5. [DOI] [PubMed] [Google Scholar]
- 6.Boon A, Cheriex E, Lodder J, et al. Cardiac valve calcification: characteristics of patients with calcification of the mitral annulus or aortic valve. Heart 1997;78:472–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aronow WS, Schwartz KS, Koenigsberg M. Correlation of serum lipids, calcium, and phosphorus, diabetes mellitus and history of systemic hypertension with presence or absence of calcified or thickened aortic cusps or root in elderly patients. Am J Cardiol 1987;59:998–9. [DOI] [PubMed] [Google Scholar]
- 8.Otto CM, Lind BK, Kitzman DW, et al. Association of aortic-valve sclerosis with cardiovascular mortality and morbidity in the elderly.N Engl J Med 1999;341:142–7. [DOI] [PubMed] [Google Scholar]
- 9.Pohle K, Mäffert R, Ropers D, et al. Progression of aortic valve calcification. Association with coronary atherosclerosis and cardiovascular risk factors. Circulation 2001;104:1927–32. [DOI] [PubMed] [Google Scholar]
- 10.Novaro GM, Tiong IY, Pearce GL, et al. Effect of hydroxymethylglutaryl coenzyme A reductase inhibitors on the progression of calcific aortic stenosis. Circulation 2001;104:2205–9. [DOI] [PubMed] [Google Scholar]
- 11.Tentolouris C, Kontozoglou T, Toutouzas P. Familial calcification of aorta and calcific valve disease associated with immunologic abnormalities. Am Heart J 1993;126:904–9. [DOI] [PubMed] [Google Scholar]
- 12.Ortlepp JR, Hoffmann R, Ohme F, et al. The vitamin D receptor genotype predisposes the development of calcific aortic valve stenosis. Heart 2001;85:635–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang AY, Woo J, Wang M, et al. Association of inflammation and malnutrition with cardiac valve calcification in continuous ambulatory peritoneal dialysis patients. J Am Soc Nephrol 2001;12:1927–36. [DOI] [PubMed] [Google Scholar]
- 14.O’Brien KD, Reichenbach DD, Marcovina SM, et al. Apolipoprotein B, (a) and E accumulate in the morphological early lesion of “degenerative” valvular aortic stenosis. Arterioscler Thromb Vasc Biol 1996;16:523–32. [DOI] [PubMed] [Google Scholar]
- 15.Olsson M, Thyberg J, Nilsson J. Presence of oxidized low density lipoprotein in nonrheumatic stenotic aortic valves. Arterioscler Thromb Vasc Biol 1999;19:1218–22. [DOI] [PubMed] [Google Scholar]