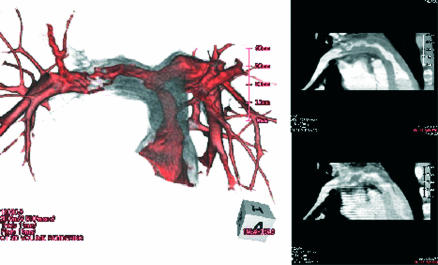
A 38 year old man without any symptoms was referred to our hospital for examination of a heart murmur. There were signs of right ventricular overload on the ECG. Doppler echocardiographic measurements demonstrated a maximum pressure gradient of 105 mm Hg across the right ventricular outflow tract. Lung perfusion scanning demonstrated reduced tracer uptake in the right lung. Although we initially suspected pulmonary thromboembolism, the computed tomographic angiography revealed severe luminal stenosis and a solid mass arising from the right ventricular outflow tract extending into both left and right pulmonary arteries (see fig), which are atypical findings for pulmonary thromboembolism. The morphological characteristics detected by computed tomography suggested the diagnosis of pulmonary artery sarcoma. After intraoperative pathologic examination of the frozen section confirmed the diagnosis of pulmonary artery sarcoma, radical resection and reconstructive surgery using a cryopreserved homograft were performed. The patient received postoperative radiotherapy and chemotherapy, and has remained well over the subsequent 10 months.
Pulmonary artery sarcoma is extremely rare and has a poor prognosis. The diagnosis is difficult and often initially misdiagnosed as pulmonary thromboembolism. It has been reported that a mean survival is only 1.5 months after diagnosis without surgical intervention. Early diagnosis and aggressive surgical treatment are the only ways of effecting a cure. Computed tomography may offer adequate information on the extent of a neoplasm, which helps us to differentiate a pulmonary artery sarcoma from pulmonary thromboembolism.