“Life is the art of drawing sufficient conclusions from insufficient premises”—Samuel Butler
The French paradox is the observation of low coronary heart disease (CHD) death rates despite high intake of dietary cholesterol and saturated fat.1,2 The French paradox concept was formulated by French epidemiologists3 in the 1980s. France is actually a country with low CHD incidence and mortality (table 1). The mean energy supplied by fat was 38% in Belfast and 36% in Toulouse in 1985–86.4 More recently, in 1995–97, the percentage of energy from fat was 39% in Toulouse according to a representative population survey.
Table 1.
Age standardised coronary heart disease (CHD) mortality and event rate in selected European regions (men, aged 35–64 years)
| Population | Official CHD mortality rate per 100000* | CHD mortality per 100000† | Coronary events per 100 000‡ |
| Glasgow (UK) | 332 | 365 | 777 |
| Belfast (UK) | 280 | 279 | 695 |
| Lille (northern France) | 89 | 172 | 298 |
| Strasbourg (north eastern France) | 80 | 141 | 292 |
| Toulouse (south western France) | 53 | 91 | 233 |
| Barcelona (north eastern Spain) | 63 | 76 | 210 |
*Based on death certificate enumeration.
†Fatal events included definite, possible, and unclassifiable (mainly sudden deaths with no available diagnostic information) coronary deaths.
‡Coronary events included non-fatal events (definite myocardial infarction) and fatal events.
THE FRENCH PARADOX AND CAUSES OF DEATH
The first source of error could come from an underestimated CHD mortality. According to this hypothesis, French physicians may not declare all the CHD deaths as CHD. If standardised data—for example those provided by the MONICA (monitoring of trends and determinants in cardiovascular disease) project—are used, the results concerning CHD attack and mortality rates show that France is at a low risk for CHD (table 1). Under certification of CHD deaths in France is a possible bias, but after correction, it remains a low bias. Thus, validated data on CHD mortality and incidence show that France is characterised by CHD risk, corroborating the first part of the French paradox definition.
THE FRENCH PARADOX AND SATURATED FAT
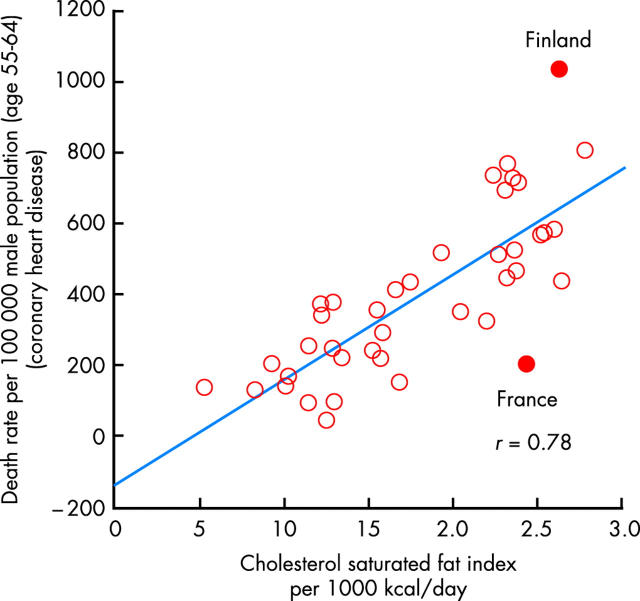
In correlation studies, measures that represent characteristics of an entire population (consumption of animal fat, daily milk, and alcohol) are used to describe disease (CHD mortality). Limitations of correlational studies are the inability to link exposure with disease in particular individuals, the lack of ability to control the effects of potential confounding factors, and the use of average exposure levels rather than actual individual values. Numerous correlation studies have been carried out in various countries concerning the relation between consumption of fat and CHD mortality.1,2 In one of the most interesting ones, Artaud-Wild and colleagues examined the relation of CHD mortality to the intake of foodstuffs and nutrients in 40 countries.2 After having defined a cholesterol–saturated fat index (CSI), they studied the relation between the CSI and CHD mortality (per 100 000 men aged 55–64 years) for all 40 countries (fig 1). France had a CSI of 24 per 1000 kcal and a CHD mortality rate of 198, whereas Finland had a CSI of 26 per 1000 kcal and a CHD mortality rate of 1031.
Figure 1.
Plot of death rate from coronary heart disease (1977) correlated with daily dietary intake (from 1976 to 1978) of cholesterol and saturated fat as expressed by the cholesterol fat index (CSI) per 1000 kcal. Reproduced from Artaud-Wild et al,2 with permission.
In the seven countries study, 12 763 men from 16 cohorts in seven countries were examined for CHD risk factors in 1958. Information on diet was collected by use of seven day food records.5 The average consumption of animal food groups, with the exception of fish, was positively associated with 25 year CHD mortality rates. Furthermore, the average population intake of saturated fat was strongly related to 10 and 25 year CHD mortality rates.
It is interesting to compare the World Health Organization dietary recommendations for saturated fat (< 10% of total energy) with actual intakes in France. In representative cross sectional surveys of the French population performed in 1986–87 and 1995–97, the saturated fat intake was 15% of the total energy intake in the first survey and 16% in the latter survey. This high consumption of saturated fatty acids is such that French subjects are exposed to a high risk of CHD. Why a high consumption of saturated fatty acids does not lead to a high CHD risk in France (and maybe elsewhere) is a central question behind the French paradox concept. The French paradox is a way of presenting provocative results from epidemiological studies and does not take into account causality between risk factors and CHD mortality.
THE FRENCH PARADOX AND WINE DRINKING
Even if causality is not part of the French paradox, some authors have put forward several hypotheses in order to explain it. Debates have focused on alcohol consumption and, more specifically, on red wine. A superficial investigation of the lifestyles of south European countries, characterised by low CHD incidence, confirms wine as one of their common identifying elements. In a seminal paper,1 Renaud and De Lorgeril compared age standardised annual mortality from CHD and related risk factors in MONICA populations, including the French centres. The mean serum total cholesterol concentrations were similar in France, in the USA, and the UK. After having performed a regression analysis between death rate from CHD and consumption of dairy fat and wine, these authors concluded that the French paradox may be caused by a high consumption of wine. Their article has started a long series of research studies analysing the relation between wine and CHD.
Final results do depend on the cultural background of the countries where they have been carried out. The most striking illustration is the classic contrast between cultures with moderate and regular alcohol consumption and those where “binge” drinking is common. It would take too long to report on all the studies dealing with the relations between alcohol and CHD.6 The only clear message is that moderate alcohol drinking (two or three times a day) has a protective effect against CHD. Alcohol intake raises high density lipoprotein (HDL) cholesterol concentrations and approximately 50% of the risk reduction attributable to alcohol consumption is explained by changes in HDL cholesterol. However, the differential effects of wine, beer, and spirits have been examined. European research carried out in France and Denmark has shown that wine consumption has been associated with a decrease of 24–31% in all cause mortality; little to moderate wine drinking leads to lower mortality from cardiovascular disease than an equivalent consumption of beer or spirits.7
Which mechanisms are responsible for the potential different effects of the various types of alcohol? We have to turn towards current theories on atherogenesis. The dominant theory is the oxidative modification hypothesis. Oxidised lipids, especially phospholipids, generated during low density lipoprotein (LDL) oxidation or within oxidatively stressed cells, are the triggers for many of the events seen in developing lesions.8 Flavonoids are components of a wide variety of edible plants, fruit, and vegetables and of beverages such as tea, coffee, beer, and wine. In vitro, inhibition of LDL oxidation by flavonoids derived from red wine has been demonstrated. In men, consumption of red wine with meals reduces the susceptibility of human plasma and LDL to lipid peroxidation. Red wine contains a variety of polyphenols derived from grape skins. In free living subjects,9 concentration of catechin in plasma was threefold higher in a diet with fruit and vegetables but without wine, than a diet without fruit, vegetables, and wine, and fourfold higher than in the latter in a diet with red wine but without vegetables and fruit. It seems that red wine and the Mediterranean diet may confer an additional protective effect. It is possible that, after adjustment for total alcohol intake, wine consumption might be associated with a more favourable lipid profile than beer consumption: higher HDL cholesterol, lower triglycerides and fibrinogen concentrations. Indeed, alcohol consumption and associated lifestyles may have an effect on CHD above and beyond their impact on lipids.
The impact on haemostasis has also been debated.1,6 In the Caerphilly prospective heart disease study, platelet aggregation induced by adenosine diphosphate was inhibited in subjects who drank alcohol. Furthermore, in the Western group of the Lyon diet heart study, there was an inverse relation between ethanol (wine represented 88% of total ethanol) and ex vivo platelet aggregation; this correlation was absent in the Mediterranean group. Platelet aggregation was low and the same in both groups, suggesting that platelet aggregation was low in the Mediterranean group because of the diet (rich in α linolenic acid) and in the Western group (diet relatively rich in saturated fat) because of wine.
The effect on blood pressure is worthy of attention, deserving an analysis. In France, alcohol consumption is rather homogeneous throughout the week whereas in Northern Ireland, Fridays and Saturdays account for 66% of total alcohol consumption.10 After adjustment for all the classical risk factors, blood pressure levels are higher in drinkers in Northern Ireland on Monday and decrease until Thursday whereas blood pressure levels are constant throughout the week in French drinkers.10 One can conclude that the “binge” drinking pattern observed among drinkers in Northern Ireland leads to disadvantageous consequences regarding blood pressure levels, consistent with a higher incidence of CHD on Mondays and Tuesdays and a lower incidence on Fridays in the Belfast MONICA register. The ethanol content of alcohol beverages seems to be a determining protective factor against CHD. However, the effects of regular alcohol consumption are complex. So it can be concluded that it is difficult to compare the effects of wine consumption in populations with low intake or with different wine consumption patterns with populations of wine drinkers showing very different lifestyles (see below).
THE FRENCH PARADOX AND THE VARIABILITY OF CHD
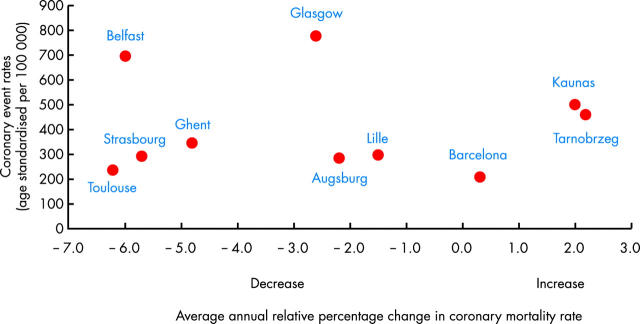
The MONICA project has provided an overview of CHD event rates in 37 populations from 1985 to 1993 and these data show a large variability in CHD event rates depending on persons, place, and time. Some countries present low or high CHD incidence and dissimilar CHD mortality trends (fig 2). Analysis of fig 2 shows that France has low CHD incidence, but not very dissimilar to that observed in other countries such as Belgium (Ghent) or Spain (Barcelona). Moreover, fig 2 shows that countries exhibit different CHD mortality trends. Some regions with rather low CHD attack rates show a significantly declining trend in CHD mortality (Ghent, Toulouse, Strasbourg) or a more limited decrease (Augsburg, Lille) or even an increase (Barcelona). Some regions with high CHD attack rates present dissimilar trends in CHD mortality, a significant decrease (Belfast), a more limited decrease (Glasgow), or even a significant increase (Kaunas, Tarnobrzeg). In a recent study in Oxfordshire,11 the CHD attack rates in men were 273 per 100 000, much lower than rates reported by MONICA centres in Glasgow and Belfast and similar to rates reported by MONICA centres in France and northern Italy. France has actually low CHD incidence and, in reality, it is very close to Germany, Italy or Spain. New paradoxes may emerge in CHD mortality and in CHD case fatality trends or in epidemiological situations within each country. In any case, whatever the terms—French paradox, North-South paradox, or Mediterranean paradox—the most difficult issue is not the description but the explanation.
Figure 2.
Relation between trends in coronary heart disease mortality rates and coronary heart disease event rates in selected MONICA populations 1985 to 1993 (men aged 35–64 years).
Recently, the Framingham risk function has been tested on other populations. In these studies, it has overestimated absolute coronary risk in diverse populations: Japanese, Hispanic males living in the USA; Italian males in Italy; Danish and French males and females.12 The general conclusion was that the Framingham models should not be used to predict absolute CHD risk in populations with different incidences. A more appropriate CHD risk function could be produced locally. However, a single risk function derived in one place at a particular time may not be applicable elsewhere and must be adjusted for geographical and temporal factors. Furthermore, the contribution of classical risk factors to the trends in CHD over 10 years across the WHO MONICA project populations has been studied: variability of CHD event rates have been explained by trends of major risk factors in only 15% in women and 40% in men. These results suggest that other CHD risk factors should be measured or discovered, particularly in countries with a low CHD incidence.
THE FRENCH PARADOX AND INTERVENTION STUDIES
In the Cochrane Collaborative meta-analysis of 27 randomised intervention trials lasting more than six months, no significant effect was shown with reduced or modified dietary fat on overall mortality, cardiovascular mortality or cardiovascular events after sensitivity analysis.13 In another review,14 Hu and Willet acknowledged that simply lowering the percentage of energy from total fat in the diet is unlikely to improve lipid profile or reduce CHD incidence. On the contrary, studies using a whole diet approach showed significant and conclusive results. The Lyon diet heart study15 randomised 605 French patients with CHD to either a diet rich in fruit, vegetables, nuts and α linolenic acid-rich margarine or their usual diet (a prudent Western diet). After two and four years, the intervention diet group had significantly reduced cardiovascular end points, although CHD risk factors were comparable between groups before and after enrolment. The Indo-Mediterranean diet heart study16 randomised 1000 patients with CHD or surrogate risk factors to either a diet rich in whole grains, fruit, vegetables, walnuts, and almonds, or their local diet. The mean intake of α linolenic acid was significantly greater in the intervention group. After two years, total cardiac end points were significantly fewer in the intervention group than the controls. The spectacular results obtained in the Lyon and the Indo-Mediterranean diet heart studies, and in other studies, concern mainly secondary prevention. Nevertheless, the French paradox refers to primary prevention and to lifestyles firmly rooted in countries with low CHD incidence. But what do we know about the relation between CHD risk factors, lifestyles, and CHD risk?
THE FRENCH PARADOX AND THE DIET–HEART HYPOTHESIS
The classical risk factors are those of CHD found in France and any other country in western Europe. However, significant differences in CHD risks are observed for similar CHD risk factor levels. In the seven countries study, at a cholesterol value of 5.2 mmol/l, the CHD mortality rates were five times higher in northern Europe than in Mediterranean southern Europe. Within Europe, similar relative risks for CHD in relation to cholesterol are to be observed, but with notably different absolute risks.17 In the same study, the authors observed that the relative increase in 25 year mortality from CHD for a given increase in blood pressure was similar among the populations. However, at systolic and diastolic blood pressure of about 140 and 85 mm Hg, respectively, 25 year rates of mortality from CHD varied by a factor of more than three among the populations, with high rates in the USA and northern Europe and low rates in Japan and Mediterranean countries. In the Gerona province (Spain), a high prevalence of risk factors contrasted with a low incidence of CHD.18 The prevalence of total cholesterol, blood pressure, smoking, and obesity in the Gerona province were lower than those of North Karelia (Finland) but higher than those of Minnesota (USA). The authors stated that the French paradox could be extended to the paradoxical coexistence of high prevalence of risk factors and low CHD incidence in southern Europe.18
Other risk factors may partly account for the differences of CHD risk between northern and southern European countries. In the MONICA project, there was a significant association between CHD mortality and plasma homocysteine, Toulouse (France) having one of the lowest values of the latter. For some researchers, France and other regions have a high consumption of fruit and vegetables, rich sources of folate, and this may explain the French paradox. Fibrinogen is a strong risk marker for CHD. In a prospective cohort (PRIME) study involving 10 600 men living in four regions (Lille, Strasbourg, and Toulouse in France, Belfast in Northern Ireland), the association of plasma fibrinogen with the incidence of CHD was significant even after adjustment for other CHD risk factors. These factors explained 25% of the excess risk of CHD in Belfast compared with France, while fibrinogen alone accounted for 30%.19 Physical activity patterns could also explain, at least partly, the gradient in CHD observed between these two countries. In the same PRIME study, subjects with higher, regular, leisure time physical activity energy expenditure had a lower incidence of CHD over a five year follow up. Although total physical activity levels were similar, French men performed more leisure time physical activity, which may contribute to their lower incidence of CHD in comparison with Northern Ireland.
The diet–heart hypothesis is a very important but rather complex concept. The above debate about the relation between wine, other alcohols, and CHD incidence is at the centre of the diet–heart hypothesis. Indeed, all the facets of wine drinkers’ behaviour cannot be summed up in wine consumption. In France, total alcohol, wine, and beer consumption was negatively related to socioeconomic status and educational level; on the other hand in Northern Ireland, total alcohol, beer, and spirits consumption was negatively related whereas wine consumption was positively related to socioeconomic status and educational level. Data indicate that even within France, the total amount and the consumption of the different types of alcoholic beverages vary considerably according to the geographical region. Thus, considering the relation between CHD and alcohol consumption per se, not taking into account the general nutritional pattern of the population studied, might lead to spurious results, since differences in alcohol consumption might also reflect differences in nutritional intake. For example, in Toulouse there is a higher consumption of wine than in Belfast, but also a higher consumption of vegetables and fruit.4 Similar results were obtained in a cross sectional study in the USA. The US researchers suggested that people who consume wine have health habits that could influence other health outcomes, and their behaviour might result in a lower incidence of cancer and all cause mortality.
Central to the diet–heart hypothesis are the attitudes to food and its role in life. In an interesting study,20 adults and college students from Flemish Belgium, France, USA, and Japan were surveyed and questioned about beliefs and attitudes concerning the diet–health link. Generally, the US group associated food most with health and least with pleasure, while the French group were the most food–pleasure orientated and the least food–health orientated. The authors concluded that diet–health and food concerns do differ across cultures and may exert a negative influence on health.20
So far, in this article, we have barely mentioned the roles played by social epidemiology and psychology in CHD. A recently published study exploring the question of whether psychosocial variables could partly explain the French paradox, within the Northern Irish-French PRIME study, provided little support for the psychosocial risk hypothesis. However, other interesting studies suggest that cardiovascular reactivity can predict the development of some preclinical states and perhaps new clinical events.
THE FRENCH PARADOX AND PUBLIC HEALTH IMPLICATIONS
Some facts cited in this article are inconsistent with the known risk factors for CHD and are thus paradoxical. These paradoxes are neither linked to a specific country nor to specific mechanisms operating in atherosclerosis. This review has not discussed the role of genetic factors, despite the fact that gene–environmental interactions are probably fundamental in atherosclerosis. However, currently available data and, more specifically, the changing trends in CHD incidence and mortality rates support the hypothesis of a fundamental role played by environmental and behavioural factors. The French paradox concept discusses classical risk factors and probably numerous protective factors which are specific to determined regions and largely unidentified. The French paradox does not teach other countries any lessons since each country has probably its own appropriate preventive solutions. Like Butler, we must end by “drawing sufficient conclusions from insufficient premises”. In primary prevention, adherence to lifestyle guidelines is associated with a very low risk of CHD. The French paradox concept should foster research on protective CHD risk factors while conveying, in primary prevention, messages promoting healthy behaviour such as regular physical exercise, optimal diet, and life without smoking. Time is still needed to define new factors in the field of gene–environment interactions or social epidemiology, or to provide an even better definition of optimal diet and regular physical exercise.
The French paradox: key points.
A high intake of dietary cholesterol and saturated fat but low CHD death rates define the French paradox
Variability of CHD rates is the rule, and low CHD rates are observed in southern or Mediterranean European countries
Classical risk factors do not embrace the totality of CHD risk, particularly in France and in other southern European countries
Complex behaviour concerning wine drinking and attitudes to food could lower CHD incidence
The French paradox suggest that the promotion of primary prevention, based on an optimal diet rich in fruit and vegetables, regular physical exercise, and life without smoking, is worthwhile
The French paradox is an incentive for more research in countries with low CHD incidence and probably more protective CHD risk factors
Supplementary Material
REFERENCES
- 1.Renaud S, de Lorgeril M. Wine, alcohol, platelets, and the French paradox for coronary heart disease. Lancet 1992;339:1523–6. ▸ This reference gives the definition of the French paradox and suggests the inhibition of platelet reactivity by wine may be one explanation for protection from CHD in France. [DOI] [PubMed] [Google Scholar]
- 2.Artaud-Wild SM, Connor SL, Sexton G, et al. Differences in coronary mortality can be explained by differences in cholesterol and saturated fat intakes in 40 countries but not in France and Finland. A paradox. Circulation 1993;88:2771–9. ▸ France and Finland have similar intakes of cholesterol and saturated fat, but consumption of vegetables and vegetable oil containing monounsaturated and polyunsaturated fatty acids is greater in France than in Finland. [DOI] [PubMed] [Google Scholar]
- 3.Richard JL, Cambien F, Ducimetière P. Epidemiologic characteristics of coronary disease in France. Nouv Presse Med 1981;10:1111–4. [PubMed] [Google Scholar]
- 4.Evans A, Ruidavets JB, McCrum E, et al. Autres pays, autres coeurs ? Dietary patterns, risk factors and ischaemic heart disease in Belfast and Toulouse. QJM 1995;88:469–77. ▸ The classical CHD risk factors do not explain the large differences in CHD between Belfast (UK) and Toulouse (France), and total fat consumption do not differ between the centres. [PubMed] [Google Scholar]
- 5.Kromhout D, Keys A, Aravanis C, et al. Food consumption patterns in the 1960s in seven countries. Am J Clin Nutr 1989;49:889–94. [DOI] [PubMed] [Google Scholar]
- 6.Chadwick DJ, Goode JA.eds. Alcohol and cardiovascular diseases: Novartis Foundation Symposium 216. New York: John Wiley and Sons, 1998:272.
- 7.Gronbaek M, Becker U, Johansen D, et al. Type of alcohol consumed and mortality from all causes, coronary heart disease, and cancer. Ann Intern Med 2000;133:411–9. ▸ A study of the relation between different types of alcohol and mortality. Wine may have a beneficial effect on all cause mortality attributable to a reduction in death from both CHD and cancer. [DOI] [PubMed] [Google Scholar]
- 8.Steinberg D. Atherogenesis in perspective: hypercholesterolemia and inflammation as partners in crime. Nat Med 2002;8:1211–7. [DOI] [PubMed] [Google Scholar]
- 9.Ruidavets JB, Teissedre PL, Ferrières J, et al. Catechin in the Mediterranean diet: vegetable, fruit or wine? Atherosclerosis 2000;153:107–17. [DOI] [PubMed] [Google Scholar]
- 10.Marques-Vidal P, Arveiler D, Evans A, et al. Different alcohol drinking and blood pressure relationships in France and Northern Ireland. The PRIME study. Hypertension 2001;38:1361–6. ▸ In France, alcohol consumption is rather homogeneous throughout the week. “Binge” drinking patterns observed among Northern Ireland drinkers leads to high blood pressure, consistent with a higher incidence of myocardial infarction on Mondays and Tuesdays. [DOI] [PubMed] [Google Scholar]
- 11.Volmink JA, Newton JN, Hicks NR, et al. Coronary event and case fatality rates in an English population: results of the Oxford myocardial infarction incidence study. The Oxford myocardial infarction incidence study group. Heart 1998;80:40–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Menotti A, Lanti M, Puddu PE, et al. Coronary heart disease incidence in northern and southern European populations: a reanalysis of the seven countries study for a European coronary risk chart. Heart 2000;84:238–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hooper L, Summerbell CD, Higgins JP, et al. Reduced or modified dietary fat for preventing cardiovascular disease. Cochrane Database Systematic Revue 2001; (3):CD002137. [DOI] [PubMed]
- 14.Hu FB, Willett WC. Optimal diets for prevention of coronary heart disease. JAMA 2002;288:2569–78. [DOI] [PubMed] [Google Scholar]
- 15.de Lorgeril M, Renaud S, Mamelle N, et al. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet 1994;343:1454–9. ▸ The first demonstration of the efficacy of a Mediterranean diet on various outcomes in secondary prevention. [DOI] [PubMed] [Google Scholar]
- 16.Singh RB, Dubnov G, Niaz MA, et al. Effect of an Indo-Mediterranean diet on progression of coronary artery disease in high risk patients (Indo-Mediterranean diet heart study): a randomised single-blind trial. Lancet 2002;360:1455–61. ▸ A final confirmation that a Mediterranean diet rich in α linolenic acid induces a better prognosis in patients with CHD. [DOI] [PubMed] [Google Scholar]
- 17.Kromhout D. On the waves of the seven countries study: a public health perspective on cholesterol. Eur Heart J 1999;20:796–802. ▸ Within Europe, similar relative risks for CHD in relation to cholesterol are observed, but with notably different absolute risks: high risks in northern Europe and low risks in the Mediterranean southern Europe. [DOI] [PubMed] [Google Scholar]
- 18.Masia R, Pena A, Marrugat J, et al. High prevalence of cardiovascular risk factors in Gerona, Spain, a province with low myocardial infarction incidence. REGICOR investigators. J Epidemiol Community Health 1998;52:707–15. ▸ The prevalence of CHD risk factors in Gerona (Spain) is higher than that of Minnesota (USA), where the CHD incidence is three times higher. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Scarabin PY, Arveiler D, Amouyel P, et al. Plasma fibrinogen explains much of the difference in risk of coronary heart disease between France and Northern Ireland. The PRIME study. Atherosclerosis 2003;166:103–9. [DOI] [PubMed] [Google Scholar]
- 20.Rozin P, Fischler C, Imada S, et al. Attitudes to food and the role of food in life in the U.S.A., Japan, Flemish Belgium and France: possible implications for the diet-health debate. Appetite 1999;33:163–80. ▸ A study of the attitudes to food in different countries. The Americans, who do the most to alter their diet, are the least likely to classify themselves as healthy eaters. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.