Abstract
Antiplatelet medications such as clopidogrel and tirofiban (glycoprotien IIb/IIIa inhibitors) are associated with a reduction in mortality and morbidity and are therefore recommended in the treatment of acute coronary syndromes. Massive pulmonary haemorrhage is a rare complication of both clopidogrel and tirofiban. Pulmonary haemorrhage may easily be mistaken for acute pulmonary oedema, a condition commonly seen in patients with acute coronary syndrome. Physicians need to be aware of this diagnostic dilemma because early treatment increases the chances of patient survival.
Keywords: pulmonary haemorrhage, acute coronary syndrome, clopidogrel, tirofiban
A 62 year old man presented to the emergency department with a three hour history of severe central chest pain associated with sweating and radiating to the neck. He had previously been well. He had smoked five cigarettes a day for 40 years. On examination the patient was in distress with blood pressure 110/82 mm Hg and pulse 110 beats/min in sinus rhythm. His ECG showed widespread ST depression. Acute coronary syndrome (unstable angina pectoris/non-ST segment elevation myocardial infarction (NSTEMI)) was diagnosed. He was given intravenous morphine, glyceryl trinitrate, heparin, and propranolol. Oral loading with aspirin 300 mg and clopidogrel 300 mg was given, followed by maintenance doses of 100 mg and 75 mg, respectively. Despite adequate analgesia the patients’ pain did not resolve and the ECG showed persistent widespread ST depression. Intravenous tirofiban infusion was started with view to emergency cardiac catheterisation. However, the patients’ pain resolved and ECG returned to normal within half an hour.
Seven hours later the patient was noted to be slightly dyspnoeic at rest and repeat chest radiography (fig 1, upper panel) showed new alveolar shadowing especially in the upper zone compared with a normal admission chest radiography. An echocardiogram showed a left ventricular function ejection fraction of 17% and no valvar dysfunction. He was treated for heart failure. On the second day the patient became hypotensive and haemoglobin had dropped from 14.5 g/l on admission to 11.6 g/l. A Swan-Ganz catheter was inserted and the following readings obtained: heart rate 85 beats/min, mean arterial blood pressure 70 mm Hg, central venous pressure 2 mm Hg (normal range 0–5 mm Hg), pulmonary capillary wedge pressure 2 mm Hg (normal range 8–12 mm Hg), cardiac index 2.4 l/min/m2 (normal range 2.5–4.5 l/min/m2), and systemic vascular resistance 1826 dyne/s/cm5 (normal range 800–1200 dyne/s/cm5). These findings were suggestive of hypovolaemia and the patient was given intravenous fluid resuscitation. There was no haematemesis and faecal occult blood was negative. There was no evidence of intra-abdominal bleeding on computed tomography of the abdomen. Computed tomography of the thorax showed bilateral pulmonary airspace opacity (fig 1, lower panel) consistent with the chest radiography finding of pulmonary oedema. The patient suddenly developed recurrent chest pain with bifascicular block on his ECG. He went into cardiac arrest and during intubation a large volume of blood was aspirated from the endotracheal tube. The patient could not be resuscitated.
Figure 1.
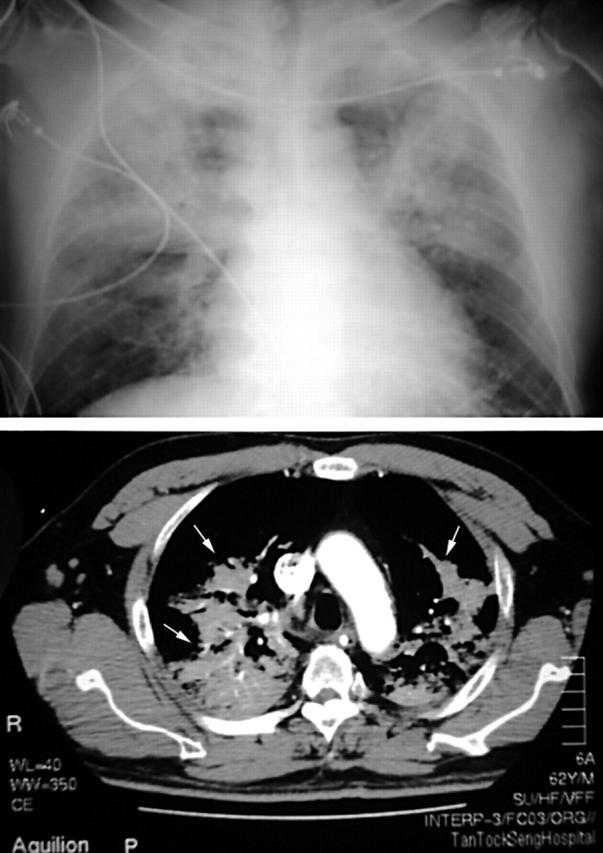
Chest radiograph (upper panel) showing bilateral “batwing” shadowing of pulmonary oedema, and computed tomography of the chest (lower panel) showing extensive airspace shadowing in both lung fields (arrows). These features are consistent with both acute pulmonary oedema and pulmonary haemorrhage.
DISCUSSION
Clopidogrel and glycoprotein IIb/IIIa inhibitors are recommended in the treatment of patients with unstable angina pectoris and NSTEMI.1 In patients with acute coronary syndromes, pulmonary infiltrates on chest radiography may be caused by pneumonia and pulmonary oedema. Anaemia and hypovolaemia are usually attributed to gastrointestinal bleeding. In our patient the signs on chest radiography were attributed to pulmonary oedema, in view of the classic appearance and the low left ventricular ejection fraction. There was clinical evidence of blood loss (hypotension, tachycardia, rising urea concentration, and falling haemoglobin) but no obvious source of bleeding.
Spontaneous massive pulmonary haemorrhage is a rare and frequently overlooked complication of both clopidogrel2 and the IIb/IIIa platelet inhibitors3 such as tirofiban. Early recognition and treatment of this complication would increase the chances of patient survival. Early diagnostic bronchoscopy may be necessary to confirm the diagnosis. Treatment consists of stopping the drugs and infusing platelets and fresh frozen plasma to correct coagulopathy. Tirofiban can also be removed by haemodialysis.
Pulmonary haemorrhage can easily be mistaken for pulmonary oedema, a condition that is common in patients with acute coronary syndromes. Physicians need to be aware of this diagnostic dilemma.
REFERENCES
- 1.Braunwald E, Antman EM, Beasley JW, et al. ACC/AHA guidelines for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction. A report of the American College of Cardiology/American Heart Association task force on practice guidelines. J Am Coll Cardiol 2000;36:970–1062. [DOI] [PubMed] [Google Scholar]
- 2.Sitges M, Villa FP. Massive pulmonary haemorrhage in a patient treated with a platelet glycoprotein IIb/IIIa inhibitor. Int J Cardiol 1997;62:269–71. [DOI] [PubMed] [Google Scholar]
- 3.Kilaru PK, Schweiger MJ, Kozman HA, et al. Diffuse alveolar haemorrhage after clopidogrel use. J Invasive Cardiol 2001;13:535–7. [PubMed] [Google Scholar]


