Ever since Mirowski implanted a defibrillator into a patient, the implantable cardioverter-defibrillator (ICD) has evolved to be the treatment of choice in patients with life threatening ventricular arrhythmias.1 Unlike in adults, the indication and benefit from ICD treatment is not well established in children. Children mainly differ from adult patients treated with an ICD by the underlying heart disease, the degree of heart failure and left ventricular function. The most common types of associated underlying cardiac diseases associated with sudden death in children are cardiomyopathies (often without a severe haemodynamic deterioration of the left ventricle), primary electrical diseases and corrected congenital heart defects, which are associated with a 25–100 fold increased risk for sudden cardiac death.2 Thus, this study was performed to analyse the potential benefit of ICDs in children and young adolescents who have a history of life threatening ventricular arrhythmias or are at high risk of an arrhythmic sudden cardiac death.
METHODS
Between 1989 and 2001, all patients aged 18 years or younger who were treated with an ICD with extended memory function (storage of electrogram and/or RR intervals from treated episodes) were included in the study. All the children had a history of sustained ventricular tachyarrhythmia, aborted sudden cardiac death, syncope attributed to ventricular tachyarrhythmias, or were at high risk of sudden cardiac death.
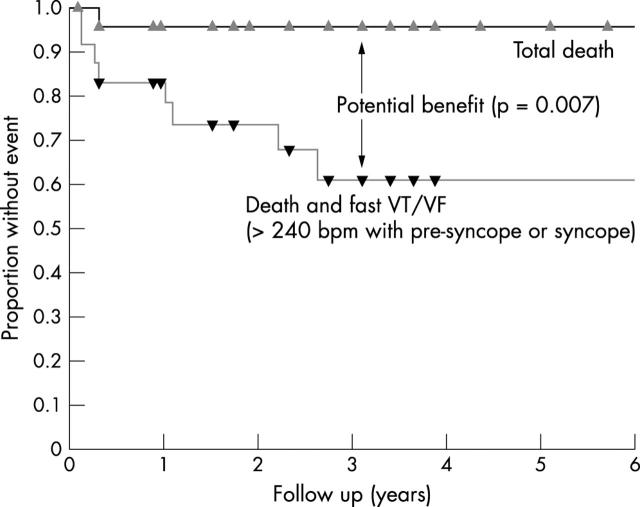
The following end points were used: (1) total death; (2) any ventricular tachycardia (VT); (3) fast highly symptomatic polymorphic VT or ventricular fibrillation (VF) (> 240 bpm with presyncope or syncope) as indicating rhythm for a potential lethal event; (4) combined end point—total death plus recurrence rate of fast symptomatic polymorphic VT or VF (> 240 bpm; presyncope or syncope) representing a high probability of death (assuming that ICD treatment would not prevent non-arrhythmic cardiac death or non-cardiac death); and (5) inappropriate episodes of any cause (supraventricular tachycardias, oversensing). The Kaplan-Meier method was used to generate survival curves for each group. Benefit of implantation of an ICD was estimated by the difference between the curves for total death and the combined end point total death and recurrences of fast symptomatic VT or VF using log rank testing.
RESULTS
Overall 25 children and young adolescents were included in the study; median age was 15.3 (9–18) years, median size 168 (125–187) cm, median weight 55 (22–85) kg. In the group of 25 patients, three patients presented with congenital heart disease, three with dilated cardiomyopathy, four with hypertrophic cardiomyopathy, four with arrhythmogenic right ventricular cardiomyopathy, three with long QT syndrome, four with idiopathic ventricular tachycardias/fibrillation, one with coronary artery disease, one with endocardial fibroelastosis, one with mitral valve disease, and one with Brugada syndrome. Mean (range) left ventricular ejection fraction was 68% (36–81%). Fourteen patients (56%) presented with VF or polymorphic VT. Six children (24%) had monomorphic VT. In five patients (20%), no sustained tachycardia was documented before ICD implantation.
The mean (SD) follow up time was 4.3 (3.4) years (range 1 month to 12 years). Two patients died during follow up; one child died 3.7 months after ICD implantation due to progressive heart failure, the second patient died nearly 11 years after ICD implantation due to acute pulmonary arterial bleeding after erosion of the upper left bronchus by an epicardial patch electrode. The total mortality rate was 4.2%, 4.2%, and 4.2% after 1, 3, and 5 years of follow up, respectively. The recurrence rate of any ventricular tachycardia was 28.9%, 52.9%, and 68.7% and the recurrence rate of fast highly symptomatic polymorphic ventricular tachyarrhythmias 12.5%, 35.9%, and 35.9% after 1, 3, and 5 years of follow up, respectively. The combined end point of total death and recurrences of fast polymorphic symptomatic VT or VF occurred in 16.7%, 49.0%, and 49.0% of patients after 1, 3, and 5 years of follow up, respectively. The potential survival benefit from ICD treatment (that is, the difference between the curves for total deaths and the combined end point of total death plus recurrences of fast symptomatic ventricular tachycardia) increased from 12.5% at 1 year to 34.8% at 3 years and then remained constant throughout the remaining follow up period (p = 0.007), respectively (fig 1). The rate of inappropriate ICD treatments was as high as 28.4%, 38.3%, and 48.6% after 1, 3, and 5 years, respectively. Ten children received inappropriate ICD treatment (seven patients with sinus tachycardia (mean heart rate 188 (22) bpm), two patients with concomitant atrial tachycardia, and one patient with lead related oversensing). The mean (SD) number of inappropriate shock treatments was 11.6 (14.7) per patient (1 to 37 shocks per patient).
Figure 1.
Actuarial survival rates for freedom from death of any cause and combined end point defined as total deaths plus occurrence of fast symptomatic ventricular tachyarrhythmias (> 240 bpm with presyncope or syncope). Benefit from ICD implantation is estimated as the difference between total mortality and the combined end point (p = 0.007).
DISCUSSION
This study provides evidence that children and young adolescents with a history of cardiac arrest, VT refractory to drug treatment, and children at high risk from sudden cardiac death may benefit from the implantation of cardioverter-defibrillators. Total survival was excellent (95.8% at 10 years). The overall rate of appropriate ICD discharges was comparable to the results of Silka et al (68.7% in 3 years compared to 68% in 31 (12) months).2 In contrast to Silka et al we calculated the potential benefit from ICD treatment based on the recurrences of fast highly symptomatic polymorphic VT or VF. The proportion of children with recurrences of fast, presumably fatal, VTs/VF was at least as high as in adults.1–3 Children are more likely to present with VF or polymorphic VT rather than monomorphic VT. Also, children are more likely to have no specific arrhythmic substrate (for example, myocardial scar from a healed myocardial infarction) and a more preserved left ventricular function. Thus, the potential benefit from ICD treatment seems to be at least as high in children and young adolescents as it is in adults.
The rate of inappropriate ICD treatments is higher in children compared to adults (38.3% v 24% after three years).4 Atrial fibrillation with rapid ventricular response is the most common cause of inappropriate ICD shocks in adults.4 In children, inappropriate ICD shocks are most often due to sinus tachycardia (70%) during sports or physical activities (6/7 children).
This study is limited in that it was carried out retrospectively with patients serving as their own controls and also because a surrogate end point was used.
The outcome of children and young adolescents treated with an ICD is excellent. Analysis of stored electrogram data suggests that ICD treatment most probably leads to a high survival benefit and prolongation of life in children and young adolescents. However, ICDs may contribute significantly to morbidity mainly due to inappropriate shock delivery in children and young adolescents.
Abbreviations
ICD, implantable cardioverter-defibrillator
VF, ventricular fibrillation
VT, ventricular tachycardia
REFERENCES
- 1.Connolly SJ, Hallstrom AP, Cappato R, on behalf of the investigators of the AVID, CASH, and CIDS studies. Meta-analysis of implantable cardioverter defibrillator secondary prevention trials. Eur Heart J 2000;21:2071–8. [DOI] [PubMed] [Google Scholar]
- 2.Silka MJ, Kron J, Dunnigan A, for the Pediatric Electrophysiology Society. Sudden cardiac death and the use of implantable cardioverter-defibrillators in pediatric patients. Circulation 1993;87:800–7. [DOI] [PubMed] [Google Scholar]
- 3.Böcker D, Bänsch D, Heinecke A, et al. Potential benefit from ICD-therapy in patients with and without heart failure. Circulation 1998;98:1636–43. [DOI] [PubMed] [Google Scholar]
- 4.Weber M, Block M, Brunn J, et al. Inadäquate Therapien durch implantierbare Cardioverter-Defibrillatoren—Inzidenz, Ursachen, prädiktive Faktoren und Vermeidungsstrategien (Inappropriate ICD-therapies—Incidence, causes, risk factors, and prevention). Z Kardiol 1996;85:809–19. [PubMed] [Google Scholar]