Myocardial ischaemia is responsible for angina, unstable angina, and, less commonly, shortness of breath secondary to ischaemic left ventricular dysfunction (angina equivalent) as well as cardiac arrhythmias. This article will deal with the mechanisms of myocardial ischaemia likely to be encountered in patients presenting with the chronic coronary insufficiency and stable symptoms of angina. It will not deal with the vessel wall based mechanisms of unstable or acute coronary syndromes which are covered elsewhere in this series.
BASIC PRINCIPLES
The undergraduate, see-saw diagram showing the perfect match between myocardial oxygen consumption (MV̇o2) and oxygen delivery to the myocardium remains at the core of our understanding of myocardial ischaemia. Changes in MV̇o2, because of their relation to symptomatology and the rather more tractable nature of this parameter experimentally, have been concentrated on as a mechanism explaining myocardial ischaemia. However, not only is it plausible that changes in oxygen delivery influence the process of myocardial ischaemia, but to explain the day to day symptoms of patients with angina, changes in both MV̇o2 and oxygen delivery together or separately must occur. Accordingly, an understanding of the mechanisms involved in regulating both of these parameters is important.
MYOCARDIAL OXYGEN CONSUMPTION
MV̇o2 is determined in large part by the parameters shown in table 1.1 Some of these, on a daily basis, remain relatively fixed (for example, myocardial mass), but it is the change in myocardial workload that is the most obvious when talking to patients who give a clear story of a relation (though not precise generally) between their symptoms and exercise. Experimentally myocardial work has required instrumentation for its quantification, however, the systolic blood pressure · heart rate double-product has been demonstrated to be a useful surrogate2 and is of clinical utility. These two component parameters are useful, therefore, when considering myocardial work, and it is the lowering of both individually by drugs, such as β blockers, that explains the clinical benefit of many antianginals.
Table 1.
Determinants of myocardial oxygen consumption (MV̇o2)
| 1 | Myocardial mass |
| 2 | Myocardial work |
| –heart rate | |
| –blood pressure | |
| 3 | Pre-contraction tension |
| –left ventricle size | |
| 4 | Inotropic status |
1 is immutable at least acutely; 2 and 3 can be manipulated for therapeutic benefit; 4 cannot be used therapeutically (see text).
The myocardium, similar to most other muscle, displays a relation between velocity of contraction and the pre-contraction tension. The increased velocity, as with any increase in energy, requires an increase in oxygen consumption. Within the myocardium the pre-contraction tension (myocardial wall tension) has a clear relation with the pre-contraction ventricular volume, where even relatively small changes in volume will be associated with quite large changes in wall tension. This too is an important therapeutic parameter to consider. Nitrate drugs, long considered to exert their action via epicardial coronary vasodilatation, now appear to exert their effect by modulation of myocardial wall tension. Nitrates are profound venodilators that reduce the venous return to the heart and thus reduce left ventricular volume, reducing myocardial wall tension and thus reducing MV̇o2 at all levels of myocardial work. It is for this reason that patients often associate the onset of their headache following nitrate administration (due to venous distension) with the deffervescence of their angina attack.
Inotropic status has a more complex relation to MV̇o2 because of adaptive mechanisms. A positive inotrope undoubtedly leads to an increase in MV̇o2. However, a negative inotrope administered under basal conditions will, in general, lead to a transient reduction in stroke volume, which is then accommodated by an increase in left ventricular volume to return the stroke volume and thus cardiac output back to its basal state. The increase in left ventricular volume that occurs induces an increase in myocardial wall tension, and thus the ensuing increase in MV̇o2 (from the increase in wall tension) balances the reduction arising from the negative inotrope.3,4 As a result negative inotropic modulation is not an effective anti-ischaemic treatment.
MYOCARDIAL OXYGEN DELIVERY
Oxygen delivery to the myocardium depends upon oxygen carriage by the blood and coronary blood flow (see below). Oxygen carriage by the blood can be disrupted by a fall in haemoglobin, and a sudden worsening of symptoms of angina in a patient who has been stable for many months or years may often be explained by the development of anaemia. Indeed, in patients with severe coronary disease a pronounced and rapidly acquired anaemia may induce ischaemia to such a degree that subendocardial infarction may ensue. It is, therefore, always wise to check the haemoglobin in unstable patients.
Coronary blood flow
The human heart receives about 1/20th of cardiac output under basal conditions.5 With exercise, coronary blood flow may rise three- to fourfold to accommodate the increase in MV̇o2. Indeed, there is an almost perfect linear relation between coronary blood flow and MV̇o2. The mandatory increase in coronary blood flow is needed by the myocardium because of near complete oxygen extraction under basal conditions (coronary sinus oxygen saturation at rest can be as low as 25–30%). This contrasts with other muscle groups where increased oxygen requirements can be met, in part, by increasing oxygen extraction and thus widening of the atrioventricular (AV) difference in oxygen saturation. One of the consequences of this balance between coronary blood flow and MV̇o2 is that it forms the basis of the practical utility of exercise testing.
Coronary blood flow, at least to the left ventricle, occurs predominantly in diastole since the resistance vessels within the heart are occluded during systolic contraction.5 The flow within the coronary vessel is determined by the driving pressure (diastolic blood pressure), the resistance (the tone within the walls of the resistance arterials—see below—and the compressive forces of the myocardium), and to a lesser extent the elastic recoil found within the conduit and capacitance vessels. The highly mutable component of these three parameters is the tone within the resistance vessels, and this accounts for a significant amount of the variability in angina symptoms and other atypical angina (see below). It is of less therapeutic potential, however, because of the absence of selective coronary microvascular vasodilator drugs.
The physiology of the myocardial resistance vessels is responsible for two important physiological phenomena:
autoregulation of coronary flow under basal conditions, maintaining a constant coronary blood flow over a wide range of diastolic pressure
the increase in coronary blood flow with exercise (metabolic regulation).
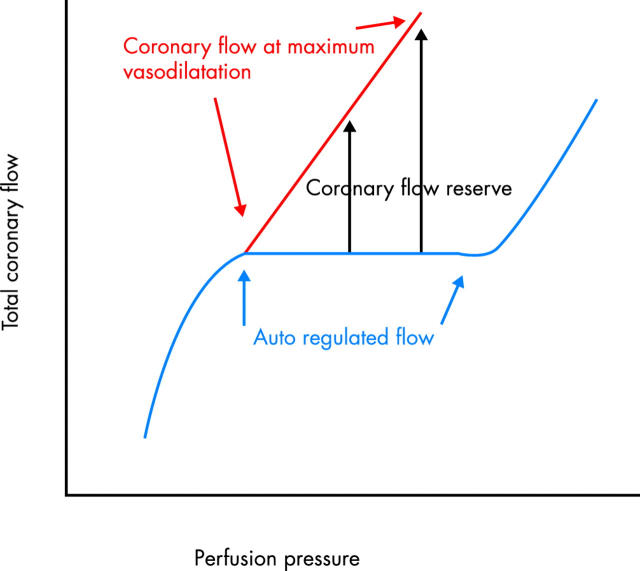
Maximum coronary blood flow induced either at maximal exercise or by pharmacological agents such as papavarine and adenosine or experimentally by transient coronary occlusions (hyperaemic flow) thus becomes a pressure driven non-autoregulated coronary flow. The difference between basal autoregulated blood flow and the maximum flow is called the coronary flow reserve (fig 1).
Figure 1.
The sigmoid line shows resting coronary blood flow which has an autoregulated range at physiological pressure. Following metabolic demands the coronary circulation undergoes vasodilatation which when maximal becomes a pressure driven system (the oblique straight line). The difference between the two lines is the coronary flow reserve which is a variable parameter depending on the perfusion pressure.
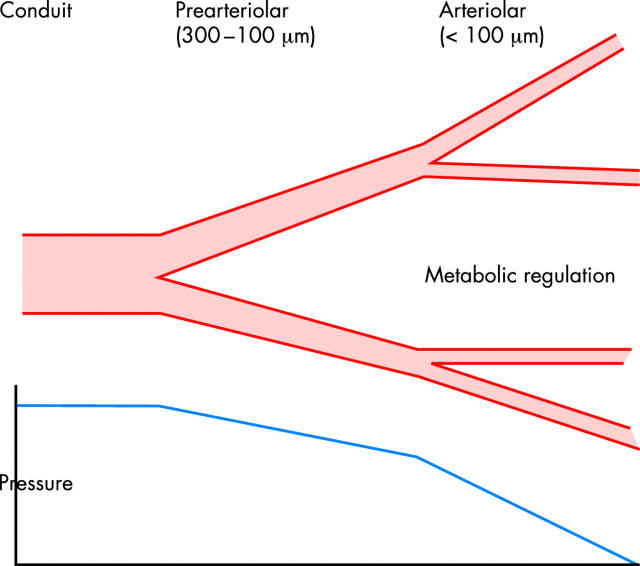
Critically important to our understanding of the regulation of coronary blood flow and thus of myocardial ischaemia is an appreciation of the site (anatomically) of the resistance within the coronary circulation, and more particularly the sites of regulated resistance responsible for autoregulation and metabolic regulation. Resistance vessels as a whole are believed to be in vessels less than 350 μm, since a fall in intracoronary pressure can be recorded in vessels below this diameter. However, it seems likely that the bulk of regulated resistance occurs in vessels less than 100 μm in diameter. These are anatomically arteriolar vessels.
Within these pre-arteriolar and arteriolar resistance vessels, some investigators have proposed a two component model for coronary resistance6 (fig 2). At the larger end of the spectrum (not precisely defined anatomically but somewhere between 350–100 μm) exist vessels that display myogenic and neurogenic responsiveness. It is probably also within this compartment that nitric oxide mediated dilatation occurs,7,8 a phenomenon that mediates the vasodilator response to the increase in coronary flow (often in turn induced by metabolic dilatation regulated by the smaller vessels). It has been speculated that dysfunction of the nitric oxide mediated dilatation in this compartment is responsible for some of the disruption of coronary blood flow seen in states where widespread endothelial cell dysfunction is seen (for example, in hypertensives). Others have also speculated that it is disruption in this compartment that is responsible for syndrome X (see below).
Figure 2.
Resistance to coronary flow is seen in two compartments. Normal epicardial coronary arteries are conduit vessels offering virtually no resistance to flow. The pre-arteriolar segments (~300–100 μm) offer variable resistance to flow and are regulated by a number of factors including nitric oxide. The arteriolar segment (< 100 μm) offers the greatest amount of resistance to flow and is the site of metabolic regulation facilitating the increase in flow with exercise.
The second compartment has been thought to reside in vessels less than 100 μm. This is the compartment that is responsible for metabolic regulation. The mechanism of metabolic regulation within the heart is still imprecisely understood, but probably involves oxygen sensing as well as a response of these vessels to adenosine released from cardiomyocytes. The flow within this second compartment, because it is in series with the first compartment, is thus not only determined by the tone within the walls of these vessels but also the driving pressure controlled by the first compartment referred to above.
PATHOPHYSIOLOGY
The relevance of the above physiological discussion is clearly related to development of angina within our patients. Broadly, angina patients can be divided into those with or without epicardial coronary disease, and certainly this is the way that these patients are managed clinically.
Angina in patients with atherosclerotic epicardial coronary disease
In general atherosclerosis in the conduit, non-resistance epicardial coronaries (1.5–4 mm) has its effect by disrupting the perfect coronary physiology outlined above, and the introduction of a new resistance to coronary flow. This acquired resistance is in series with the physiological resistors and thus has its impact on coronary flow reserve reducing this on occasions to levels not allowing sufficient oxygen delivery to the myocardium.
Atherosclerotic epicardial plaques have a complex relation to coronary resistance. Some of these (20–30%) are dynamic, albeit within a reasonably small range of reactivity where exercise or constricting agents may induce a 20% reduction in the stenosis diameter. Others, however, appear to be fixed. In addition, the longer the coronary lesion the greater the resistance and, of course, two lesions in parallel add further to stenosis significance.
The assessment of the relation between the degree of epicardial coronary narrowing and the measured coronary flow reserve is complex and generalisations are difficult. Within instrumented animals the classic work of Gould and Lipscomb in the 1970s suggests that a stenosis in a conduit vessel of less than 50% is unlikely to be of haemodynamic significance.9 For stenoses with luminal narrowing greater than 50% there is a complex and curvilinear relation to the reduction in maximum coronary flow. Lesion length also affects the coronary flow reserve, with longer lesions producing greater haemodynamic changes.10
Assessment of coronary stenosis and impact on coronary flow
Assessments of patients by angiography have, in general, shown a very imprecise relation between the degree of coronary narrowing and coronary flow reserve.11,12 However, the use of positron emission tomography (PET) scanning to measure coronary flow reserve has increased our ability to measure this difficult parameter accurately under basal conditions in humans.13 These studies have confirmed a complex relation, again curvilinear, between coronary stenosis diameter and coronary flow reserve, but it should be noted that the individual points for patients studied show remarkable scatter around any statistically defined relation. Nonetheless the PET data would not wildly disagree with the animal data indicating that stenoses less than 50% in diameter are unlikely to be of functional haemodynamic significance.
The advent of intracoronary wires able to carry Doppler and pressure transducers has allowed cardiologists to “interrogate” epicardial coronary stenoses that appear to be of borderline significance. It is not possible within this article to review these in detail. Broadly, however, these devices all rely on the induction of maximal hyperaemia with a microvascular vasodilating drug (usually adenosine) administered either intravenously or intracoronary. Devices either record the change in coronary blood velocity (Doppler wires) or measure the pressure gradient induced across the lesion (pressure wires, RADI). Doppler wires, because of technical considerations and the influence of side branches and the variability of signal if moved, have been largely an experimental tool. The pressure wire appears more stable and is easier to use. The important work of Pijls in this area has suggested that a ratio of mean distal coronary blood pressure to mean proximal coronary blood pressure following maximum hyperaemia of less than 0.75–0.8 indicates a stenosis that is of functional significance.14
Widely dynamic epicardial coronary stenosis and Prinzmetal’s variant angina
A small percentage of usually mild coronary stenoses display intense vasoconstrictive responses.15 Such constriction may be to a degree sufficient to occlude the epicardial coronary entirely, and under these circumstances ST elevation may arise. This is the pathological basis of so-called Prinzmetal’s variant angina.16 This diagnosis usually manifests itself by the complete resolution of ST elevation by the administration of nitrates or, in the catheter room, by the complete disappearance of an epicardial coronary stenosis following the administration of intracoronary nitrates. Specialist centres have advocated the use of the administration of intracoronary vasoconstrictors, particularly ergonovine, for the induction of coronary spasm as a test for this condition. In expert hands this has been used safely to induce epicardial coronary stenosis in these patients at very low doses of ergonovine (the induced constriction always responds to intracoronary nitrates). Complete or near complete constriction with myocardial ischaemia in response to ergonovine is the hallmark of variant angina patients, with non-variant angina patients displaying only a diffuse 15–20% epicardial constriction without ischaemia.17 Variant angina patients clinically describe intense angina with ST elevation or very widespread ST depression on their ECG during pain. Often the patient will describe clusters of pain for periods of a few days separated by months of pain-free periods. The reason for the exquisite sensitivity of these coronary lesions is not understood.
Chest pain with normal coronary arteries, syndrome X, and microvascular angina
Patients who present with chest pain and normal coronary arteries have a number of possible pathophysiological explanations for their symptoms. These include:
inaccuracy of coronary angiography—that is, epicardial coronary disease exists but has not been appreciated
instability of microvascular tone on exercise—so-called microvascular angina
undiagnosed Prinzmetal’s variant angina
non-coronary cardiac pain (pericardial disease, aortic stenosis, hypertrophic cardiomyopathy)
non-cardiac pain (arising from either diagnosable disease in thoracic or extra-thoracic structures or from somatosisation of psychological problems).
The first of these usually identifies itself by the presence of an unequivocally positive exercise test or isotope perfusion scan in someone with minor irregularity somewhere on the coronary angiogram. Intravascular ultrasound (IVUS) assessment has been reported to be useful. The third, Printzmetal’s variant angina, is diagnosed by the 12 lead ECG recorded “in pain” which invariably suggests significant ischaemia either as ST elevation or widespread dramatic ST depression. The fourth and fifth are beyond the scope of this article.
Syndrome X is the finding of normal coronary arteries with a positive exercise test or, on occasions, transient ST depression with pain on a 12 lead ECG. These patients have been reported to have patchy defects on very sensitive isotope scans but invariably have negative stress echocardiograms.18,19 The negative stress echo data are usually negative in the sense that though chest pain is induced there is no ischaemic left ventricular dysfunction, usually viewed as an early manifestation of ischaemia and one that may precede chest pain in the context of atherosclerotic epicardial coronary disease.
Not only is the pathogenesis of syndrome X debated but also its very existence. Those against the bona fide nature of this as a specific syndrome have either argued that the exercise tests have been over-interpreted, or that using validated techniques for the measurement of coronary blood flow no disturbance in coronary blood flow can be documented with exercise, or even that the problem is in central pain processing.20 Those who are supportive of the syndrome’s existence suggest that the so-called “definitive” tests used (often PET based) have too large a sample volume for the identification of what must be patchy ischaemia, and if magnetic resonance based techniques are used changes can be seen.21 They also point out that there is no explanation for the ischaemic ECG. The debate will run but it is the opinion of the author that the syndrome does exist though it is probably significantly overdiagnosed. Certainly, however, the epidemiology of the group of patients is not debated, and uniformly it is reported that the prognosis for these patients is excellent, though there may be many repeat attendances.
The believed pathophysiological basis is microvascular instability that dysregulates coronary blood flow. It is speculated that the disruption may be in segments where there is nitric oxide mediated vasodilatation. The absence of good coronary microvascular dilator drugs (nitrates do not dilate this segment) make conclusive testing, and treatment, difficult in this condition.
Microvascular tone, stable angina, and variability of symptoms
Whatever one’s opinion of syndrome X there is no doubt about the highly variable nature of the angina experienced by patients with proven atherosclerotic epicardial coronary disease.22 In contrast to leg claudication, where claudication distances are very predictable, angina is a symptom of variable intensity and threshold in over two thirds of patients.22 There is a large literature that indicates that this variability in symptoms is not determined by variability in the determinants of myocardial ischaemia—for example, heart rate.23
CONCLUSION
The mechanisms of myocardial ischaemia may differ between patients and within the same patient. An understanding of these different mechanisms is of considerable help in understanding patients’ symptomatology and their management.
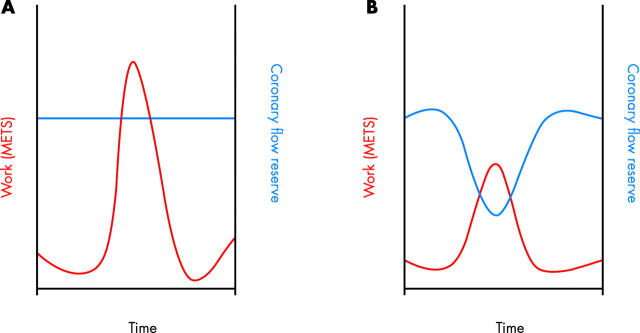
Figure 3.
(A) Coronary flow reserve is fixed and an increase in metabolic demand causes ischaemia when not accommodated by the coronary flow reserve. (B) Coronary flow reserve is variable because of microvascular influences and now a lesser amount of myocardial demand also produces ischaemia.
REFERENCES
- 1.Braunwald E. Control of myocardial oxygen consumption. Am J Cardiol 1971;27:416–32. [DOI] [PubMed] [Google Scholar]
- 2.Rooke GA, Feigl EO. Work as a correlate of canine left ventricular oxygen consumption, and the problem of catecholamine oxygen wasting. Circ Res 1982;50:273–86. [DOI] [PubMed] [Google Scholar]
- 3.Graham TP, Ross J, Covell JW, et al. Myocardial oxygen consumption in acute experimental cardiac depression. Circ Res 1967;XXI:123–38. [DOI] [PubMed] [Google Scholar]
- 4.Graham TP, Covell JW, Sonnenblick EH, et al. Control of myocardial oxygen consumption: relative influence of contractile state and tension development. J Clin Invest 1968;47:375–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Feigl EO. Coronary physiology. Physiological Rev 1983;63:1–205. [DOI] [PubMed] [Google Scholar]
- 6.Uren NG, Crake T. Resistive vessel function in coronary artery disease. Heart 1996;76:299–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Griffith TM, Edwards DH, Davies RL, et al. EDRF coordinates the behaviour of vascular resistance vessels. Nature 1987;329:442–5. [DOI] [PubMed] [Google Scholar]
- 8.Jones CJ, Kuo L, Davis MJ, et al. Role of nitric oxide in the coronary microvascular responses to adenosine and increased metabolic demand. Circulation 1995;91:1807–13. [DOI] [PubMed] [Google Scholar]
- 9.Gould KL, Lipscomb K. Effects of coronary stenoses on coronary flow reserve and resistance. Am J Cardiol 1974;34:48–55. [DOI] [PubMed] [Google Scholar]
- 10.Feldman RL, Nichols WW, Pepine CJ, et al. Hemodynamic significance of the length of a coronary arterial narrowing. Am J Cardiol 1978;41:865–71. [DOI] [PubMed] [Google Scholar]
- 11.White CW, Creighton B, Wright MD, et al. Does visual interpretation of the coronary arteriogram predict the physiologic importance of a coronary stenosis? N Engl J Med 1984;310:819–24. [DOI] [PubMed] [Google Scholar]
- 12.Folland ED, Vogel RA, Hartigan P, et al. Relation between coronary artery stenosis assessed by visual, caliper, and computer methods and exercise capacity in patients with single-vessel coronary artery disease. Circulation 1994;89:2005–14. [DOI] [PubMed] [Google Scholar]
- 13.Uren NG, Melin JA, de Bruyne B, et al. Relation between myocardial blood flow and the severity of coronary-artery stenosis. N Engl J Med 1994;330:1782–8. [DOI] [PubMed] [Google Scholar]
- 14.Pijls NH, De Bruyne B, Peels K, et al. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med 1996;334:1703–8. [DOI] [PubMed] [Google Scholar]
- 15.Crea F, Kaski JC, Maseri A. Key references on coronary artery spasm. Circulation 1994;89:2442–6. [DOI] [PubMed] [Google Scholar]
- 16.Prinzmetal M, Kennamer R, Merliss R, et al. Angina pectoris. I. A variant form of angina pectoris. Am J Med 1959;27:375–88. [DOI] [PubMed] [Google Scholar]
- 17.Feldman RL, Curry C, Pepine CJ, et al. Regional coronary hemodynamic effects of ergonovine in patients with and without variant angina. Circulation 1980;62:149–59. [DOI] [PubMed] [Google Scholar]
- 18.Nihoyannopoulos P, Kaski JC, Crake T, et al. Absence of myocardial dysfunction during stress in patients with syndrome X. J Am Coll Cardiol 1991;18:1463–70. [DOI] [PubMed] [Google Scholar]
- 19.Zouridakis EG, Cox ID, Garcia-Moll X, et al. Negative stress echocardiographic responses in normotensive and hypertensive patients with angina pectoris, positive exercise stress testing, and normal coronary arteriograms. Heart 2000;83:141–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosen SD, Paulesu E, Frith CD, et al. Central nervous pathways mediating angina pectoris. Lancet 1994;344:147–50. [DOI] [PubMed] [Google Scholar]
- 21.Panting JR, Gatehouse PD, Yang GZ, et al. Abnormal subendocardial perfusion in cardiac syndrome X detected by cardiovascular magnetic resonance imaging. N Engl J Med 2002;346:1948–53. [DOI] [PubMed] [Google Scholar]
- 22.Nesto RW, Zarich SW, Kowalchuk GJ, et al. Frequency of symptoms suggestive of dynamic coronary artery disease in patients referred for coronary angiography. Am J Cardiol 1989;64:1374–6. [DOI] [PubMed] [Google Scholar]
- 23.Chierchia S, Gallino A, Smith G, et al. Role of heart rate in pathophysiology of chronic stable angina. Lancet 1984;ii:1353–7. [DOI] [PubMed] [Google Scholar]
- 24.Pupita G, Maseri A, Kaski JC, et al. Myocardial ischemia caused by distal coronary-artery constriction in stable angina pectoris. N Engl J Med 1990;323:514–20. [DOI] [PubMed] [Google Scholar]