Abstract
Objective: To determine whether men with possible angina (from their responses to the World Health Organization angina questionnaire) but a normal exercise ECG differ in long term rates of coronary heart disease events from men with no symptoms of angina.
Design: During 1972–75, 2014 apparently healthy men aged 40–59 years underwent an examination programme including case history, clinical examination, exercise ECG to exhaustion, and various other tests. All men completed the WHO angina questionnaire.
Subjects: Of 2014 men, 68 had possible angina, 1831 had no symptoms of angina, and 115 were excluded because they had definite angina or pathological exercise ECGs. All 68+1831 had normal exercise ECGs and none developed chest pain during the exercise test.
Results: At 26 years, men with possible angina had a coronary heart disease mortality of 25.0% (17/68) v 13.8% (252/1831) among men with no symptoms of angina (p < 0.013). They also had a higher incidence of coronary artery bypass grafting (CABG) (p < 0.0004) and acute myocardial infarction (p < 0.026). The excess coronary heart disease mortality among men with possible angina only started after 15 years, whereas differences in CABG/acute myocardial infarction started early. Multivariate analysis including well recognised coronary heart disease risk factors showed that possible angina was an independent risk factor (relative risk 1.79, 95% confidence interval 1.26 to 2.10).
Conclusions: Men with possible angina, even with a normal exercise test, have a greater risk of dying from coronary heart disease, having an acute myocardial infarct, or needing a CABG than age matched counterparts with no symptoms of angina.
Keywords: WHO angina questionnaire, coronary heart disease, mortality
Chest pain on exertion detected by means of the World Health Organization angina questionnaire1 and not fulfilling all criteria for a diagnosis of definite angina (defined as “possible angina”2,3) is often encountered among middle aged and elderly people, and is of uncertain diagnostic and prognostic significance. Some recent studies2–7 claim that such individuals have a similar coronary heart disease risk to those with recognised myocardial ischaemia, though others have not found this to be the case.8–11 However, differences in definitions, materials, methods, and follow up make this an unsettled question.
In the present study, the WHO angina questionnaire1 (the relevant portion of which is reproduced in the appendix) was answered by 2014 apparently healthy middle aged men as part of a cardiovascular survey examination, primarily aimed at assessing the prevalence of chest pain or discomfort on exertion.
METHODS
In 1972, all apparently healthy men aged 40–59 years, working in five government agencies in Oslo, Norway, were invited to participate in a cardiovascular survey examination. The main aim was to look for symptoms and signs of possible latent coronary heart disease. Of 2341 eligible men, 2014 (86%) agreed to participate in the study, which started on 28 August 1972 and was finished by 30 March 1975. Eligibility was decided after scrutinising the company health records of all the men. Where recorded, the following diseases or conditions resulted in primary exclusion: known or suspected coronary heart disease or other types of heart disease, hypertension being treated with drugs, diabetes mellitus, malignancy diagnosed during the last five years, miscellaneous other serious diseases (for example, known chronic hepatic, renal, or pulmonary diseases), and any chronic drug regimen being used for any reason. Those who were judged unable to complete a symptom limited bicycle exercise test were also excluded. Men who reported acute febrile illnesses in their immediate presurvey period had to wait at least 14 days to be examined. Men who on arrival reported any of the above mentioned diseases, not recorded in the company files, were examined but were later excluded. Further details about the selection and inclusion criteria have been reported elsewhere.12
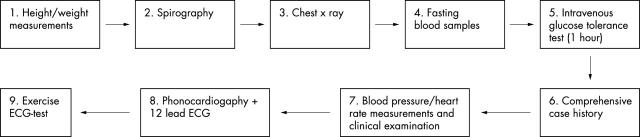
All subjects met for the examination early in the morning after at least 12 hours fasting and eight hours abstaining from smoking. All men underwent the examination programme illustrated in fig 1, and all in the same order. Detailed descriptions of the various examination procedures are given elsewhere.12,13 All had filled in an extensive health questionnaire on arrival, dealing with various health issues, including the WHO angina questionnaire1 (see appendix). The answers were thoroughly checked by the examining physician to ensure that all questions had been understood and answered, and that the answers had been given as intended.14 The WHO questionnaire was checked according accepted guidelines.1 Following the clinical examination and a resting ECG, all men completed a bicycle exercise ECG test until exhaustion, unless this had to be terminated prematurely for safety reasons. Details about the exercise test are published elsewhere.15
Figure 1.
Examination programme followed by all study participants during the cardiovascular survey.
When filling in the WHO angina questionnaire before the baseline examination, 95 men had reported chest pain or discomfort on exertion (answering yes to the first two questions in the WHO angina questionnaire). Of these, 27 had definite angina according to the WHO questionnaire and 68 men did not. The chest pain in the latter was defined as “possible angina”2,3 because, although all the men answered yes to the two first questions in the WHO angina questionnaire,1 their remaining answers did not comply with the definition of angina pectoris; and because all 68 men had a normal symptom limited exercise ECG test.
In the group of healthy men with no symptoms of angina (n = 1831), a sizable proportion answered yes to the first question in the WHO questionnaire (“Have you ever had pain or discomfort in your chest?”), but no to the remaining questions. No distinction was made between these men and men who answered no to all questions in the questionnaire.
In all, 115 of the 2014 men had one or more of the following findings during the survey examination: definite angina according to the WHO questionnaire (n = 27; see above); development of typical angina during the exercise test; or a pathological exercise ECG during or after exercise. According to the initial study protocol all men with one or more of these criteria15 were offered diagnostic coronary angiography, an offer that was accepted by 109 and refused by six. Details of the angiographic study are presented elsewhere.15 All these 115 men were excluded regardless of reported chest pain or coronary angiographic findings (approximately two thirds of them had a positive exercise ECG during or after exercise as the sole abnormal finding). Of the 27 with angina according to the WHO questionnaire, 14 had a positive exercise ECG and 13 did not. Six of the 2014 men had angina during the stress test as their only “angiography qualifying” finding.
After excluding these 115 men, the remaining 1899 (2014 − 115 = 1899) were subdivided as follows:
Group A: 1831 men with no symptoms of angina and a normal exercise test
Group B: 68 men with possible angina according to the WHO questionnaire, but a normal exercise test.
Follow up procedures
Cause specific mortality data up to 31 December 1999 were obtained from Statistics Norway after permission had been granted by the Norwegian Data Inspectorate and the Norwegian Board of Health. In the present report only deaths from coronary heart disease have been included (that is, death from acute myocardial infarction, sudden unexpected death, or death from heart failure following an earlier extensive acute myocardial infarct). The mean observation time was 26 years (range 24.8–27.3 years).
In 1995 we undertook a nationwide search in the hospital files in all Norwegian hospitals for all men in the study. We again obtained permission to do this, as mentioned above. The morbidity data are complete up to 30 June 1995. The mean observation time for morbidity events was 21.5 years (range 20.3–22.8 years). Cases of acute myocardial infarction and coronary artery bypass grafting (CABG) were specifically noted. Acute myocardial infarction was recorded regardless of whether a person died later from any other cause (that is, a man might theoretically have suffered both an acute myocardial infarct and undergone CABG (two different morbidity events) before later dying from a non-cardiac cause). If subjects had sustained more than one myocardial infarct, only the first event was counted; the same applies to (the few) men who had undergone more than one CABG.
By 1995, only two subjects were living abroad, and both were alive at that time. They were later lost to follow up. Otherwise follow up appears to be complete for the remainder. A few had lived abroad for some time before 1995, but had later returned to Norway.
Statistical methods
Differences in baseline data between the groups were tested by Student’s t test, Fisher’s exact t test, and with Wilcoxon test, according to data type.
The risk of death from coronary heart disease and of coronary heart disease events was estimated by Kaplan-Meier plots and tested with the log rank (Mantel-Cox) test.
The coronary heart disease mortality curves apparently deviated from a proportional hazards assumption. However, as only a few additional early deaths in the possible angina group would have made the assumption of proportional hazards likely, we applied the Cox analysis when further covariates were introduced in the relative risk analysis, acknowledging modest violations of the test prerequisites.
RESULTS
Compared with men from group A (healthy men with no symptoms of angina), men from group B (possible angina) had significantly higher serum cholesterol, body weight, and body mass index and lower physical fitness and maximum heart rate during exercise (table 1). All other differences were non-significant. In particular, fasting blood glucose was virtually identical in the two groups.
Table 1.
Baseline characteristics of subgroups of 1899 apparently healthy middle aged men
| Group A (n = 1831) | Group B (n = 68) | p Value, A v B | Group B | p Value, A v D | ||
| Group C (no event, n = 35) | Group D (event, n = 33) | |||||
| Age (years) | 49.6 (5.4) | 50.7 (5.9) | 0.10 | 49.5 (5.6) | 52.0 (6.0) | * |
| Smokers (%) | 44% | 35% | 0.17 | 42% | 30% | 0.45 |
| Height (cm) | 176.8 (6.2) | 175.9 (6.9) | 0.22 | 176.1 (7.0) | 175.7 (7.0) | 0.28 |
| Weight (kg) | 76.7 (9.8) | 79.8 (11.0) | ** | 78.6 (11.9) | 81.1 (10.0) | * |
| Body mass index (kg/m2) | 24.5 (2.7) | 25.8 (2.9) | *** | 25.3 (3.0) | 26.2 (2.7) | *** |
| Resting SBP (mm Hg) | 129.7 (17.6) | 131.5 (18.6) | 0.40 | 130.8 (16.9) | 132.2 (20.4) | 0.41 |
| Resting DBP (mm Hg) | 87.0 (10.4) | 88.1 (10.2) | 0.41 | 88.6 (11.0) | 87.5 (9.7) | 0.79 |
| Resting HR (beats/min) | 61.4 (9.7) | 62.1 (9.7) | 0.55 | 62.4 (10.8) | 61.7 (8.5) | 0.83 |
| MHR (beats/min) | 163.4 (13.3) | 159.4 (12.5) | * | 161.5 (12.7) | 157.3 (11.7) | *** |
| ESR (mm/h) | 7.3 (6.7) | 6.9 (5.5) | 0.60 | 6.0 (5.3) | 7.8 (5.7) | 0.68 |
| Fasting blood glucose (mmol/l) | 4.4 (0.54) | 4.5 (0.88) | 0.35 | 4.4 (0.40) | 4.6 (1.20) | 0.06 |
| Cholesterol (mmol/l) | 6.6 (1.2) | 7.1 (1.2) | ** | 6.8 (1.2) | 7.4 (1.2) | *** |
| Triglycerides (mmol/l) | 1.3 (0.7) | 1.4 (0.6) | 0.17 | 1.3 (0.5) | 1.5 (0.8) | 0.08 |
| Physical fitness (kJ/kg) | 1.97 (0.79) | 1,68 (0.57) | *** | 1.81 (0.63) | 1.54 (0.47) | *** |
| FEV1 (l) | 3.46 (0.74) | 3.44 (0.78) | 0.80 | 3.47 (0.84) | 3.40 (0.71) | 0.65 |
Group A, healthy men with no symptoms of angina at baseline; group B, men with possible angina at baseline (B). Group B is further subgrouped in subjects without (group C) and with (group D) at least one coronary heart disease event during 26 years of follow up.
*p<0.05; **p<0.01; ***p<0.001.
DBP, diastolic blood pressure; ESR, erythrocyte sedimentation rate; FEV1, forced expiratory volume in one second; HR, heart rate; MHR, maximum exercise heart rate; SBP, systolic blood pressure.
When subdividing group B in men without and with events during follow up (groups C and D respectively), some differences emerged (table 1). Compared with men without events during follow up, men with events (group D) were older, had a higher body mass index, higher cholesterol, lower maximum heart rate, and lower physical fitness. Men from group C had values virtually identical to those from group A, for all variables.
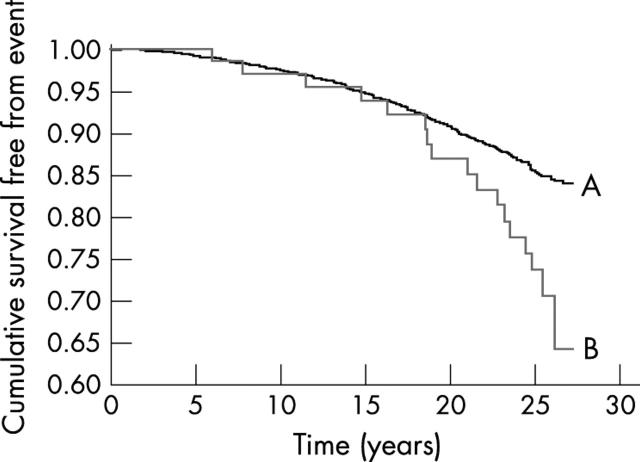
Groups A and B had almost identical survival curves up to 16–17 years, after which they started to diverge. At the end of follow up coronary heart disease mortality was significantly higher in group B than in group A (fig 2).
Figure 2.
Kaplan-Meier curves for coronary heart disease mortality in healthy men with no symptoms of angina (A) (n = 1831) and men with possible angina (B) (n = 68) (p < 0.0057).
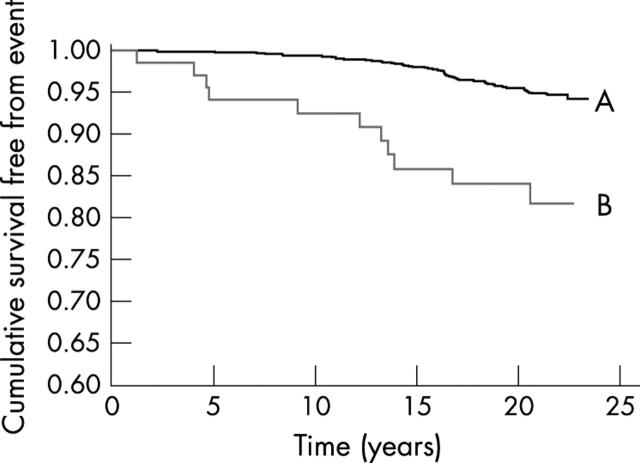
Table 2 shows that after a mean follow up period of 21.5 years, 84 subjects in group A (4.6%) and 11 (16.2%) in group B had undergone CABG (p < 0.001). There were 324/1831 (17.7%) hospital verified myocardial infarctions in group A, and 19/68 (27.9%) in group B (p < 0.05, Fisher’s exact t test) (table 2). According to a log rank test (Kaplan-Meier plot), the groups differed significantly in incidence of acute myocardial infarction (p < 0.05) (detailed data not shown).
Table 2.
Number of coronary heart disease events in healthy men with no symptoms of angina (group A) and in men with possible angina (group B)
| 1995 (30 June) | p Value | 1999 (31 December) | p Value | |||
| A (n = 1831) | B (n = 68) | A (n = 1831) | B (n = 68) | |||
| CHD, death | 184 | 8 | 0.68 | 252 | 17 | * |
| CABG | 84 | 11 | *** | ND | ND | ND |
| AMI | 324 | 19 | * | ND | ND | ND |
Follow up over 26 years for mortality and 21.5 years for morbidity events.
*p < 0.05, ***p < 0.001.
AMI, acute myocardial infarction; CHD, coronary heart disease; CABG, coronary artery bypass grafting; ND, no data available.
When investigated by Kaplan–Meier plot (fig 3) group B showed a significantly increased risk of needing CABG compared with group A.
Figure 3.
Kaplan-Meier curves for coronary arterial bypass grafting in healthy men with no symptoms of angina (A) (n = 1831) and men with possible angina (B) (n = 68) (p < 0.0004).
Mean age at the time of CABG was 58 years in group B and 63 years in group A (p < 0.001). One man in group B had already had CABG within one year of the primary examination, and three within five years. The first two deaths in group B (both from acute non-heralded myocardial infarction) occurred approximately six years after the baseline examination. Only three of the 17 who died within group B had had an earlier CABG (death occurred 10, 12, and 17 years after the procedure, respectively).
Possible angina was a strong predictor of coronary heart disease mortality in a univariate analysis; it remained a strong and independent predictor when introduced in a multivariate Cox regression model which included age, total serum cholesterol, systolic blood pressure, smoking, physical fitness, and forced expiratory volume in one second (FEV1) as covariates (all of which were also predictors of death from coronary heart disease) (table 3). Thus only a modest change in predictive power appeared for the covariate “possible angina” after adjustment for the variables listed above.
Table 3.
Relative risk of death from coronary heart disease according to Cox analysis among 1899 apparently healthy middle aged men followed up for 26 years
| RR | 95% CI | p Value | |
| Univariate analysis | |||
| Possible angina (yes/no) | 1.97 | 1.21 to 3.22 | 0.0068 |
| Multivariate analysis | |||
| Possible angina (yes/no) | 1.79 | 1.26 to 2.10 | 0.0220 |
| Age (1 SD = 5.46 years) | 1.31 | 1.14 to 1.51 | 0.0002 |
| Smoking (yes/no) | 1.63 | 1.26 to 2.10 | 0.0002 |
| Cholesterol (1 SD = 1.19 mmol/l) | 1.20 | 1.07 to 1.34 | 0.0015 |
| SBP (1 SD = 17.59 mm Hg) | 1.26 | 1.13 to 1.42 | <0.0001 |
| MHR (1 SD = 13.3 beats/min) | 0.79 | 0.69 to 0.90 | 0.0004 |
| Physical fitness (1 SD = 0.785 J/kg) | 0.83 | 0.70 to 0.99 | 0.0360 |
| FEV1 (1 SD = 0.741 l) | 0.86 | 0.75 to 0.98 | 0.0270 |
Data are given for eight variables collected during the baseline examination, including possible angina.
CI, confidence interval; FEV1, forced expiratory volume in one second; MHR, maximum heart rate on exercise; RR, relative risk; SBP, systolic blood pressure.
When a similar model was used to predict the need for CABG, possible angina proved also to be a strong and independent predictor (relative risk 3.53, 95% confidence interval 1.86 to 6.69; p < 0.01).
Eleven men with possible angina (16.1%) had developed diabetes mellitus type 2 by the 30 June 1995, compared with 137 (7.5%) among men from group A (p < 0.05).
DISCUSSION
The 68 men who answered yes to the two first questions in the WHO questionnaire had reported that their chest pain was triggered by exertion. Despite answering no to the remaining questions in the questionnaire, it is suggested—in line with prevailing views2,3—that such chest pain should be labelled “possible angina”.
Analysis of coronary heart disease mortality at 10 and 15 years from baseline suggested initially that possible angina was of little clinical significance. However, by extending the observation period further and by also considering morbidity data we have reached a different view. Thus when comparing the 68 men with possible angina and the 1831 men with no symptoms of angina, our data show, first, that possible angina appeared to be a strong predictor of coronary mortality, even after accounting for age, smoking, systolic blood pressure, total cholesterol, maximum heart rate during exercise, FEV1, and physical fitness; and second, that possible angina appeared to be a strong and independent predictor of the need for CABG.
Our current analysis shows that the survival curves of the group of men with no symptoms of angina (group A) and with possible angina (group B) started to diverge at approximately 16 to 17 years, and at 26 years group B had almost twice as high a coronary mortality as group A. This substantial difference might have been even more pronounced and possibly observable earlier if the CABG rate had not been more than three times as high within group B as within group A.
The additional and significantly higher incidence of non-fatal acute myocardial infarction in group B further highlights the high coronary heart disease risk encountered among men with possible angina compared with those with no symptoms of angina.
For validity reasons, only “hard” coronary heart disease end points have been included in this study (coronary heart disease deaths, CABG, and hospital verified acute myocardial infarction).
Three possible explanations might account for our findings. First, the high incidence of coronary heart disease events over the 26 year period in group B mainly reflected their high coronary heart disease risk profile at baseline (table 1). Second, the symptoms were misinterpreted at baseline—that is, the chest pain often represented unrecognised symptoms of coronary heart disease, and the men were left untreated until clinical progression or death occurred. Third, the chest pain reported initially was in fact of non-coronary origin, but by being told the benign nature of these symptoms, the men later chose to ignore the development of coronary symptoms, often with deleterious effects. Any or all of these explanations may be involved.
In relation to the first explanation, the baseline characteristics indicated a high coronary heart disease risk in group B and it should not therefore be surprising that some of these men already showed subtle signs and symptoms of coronary heart disease (for example, chest pain on exertion, even though modest and atypical). The follow up findings are in accordance with what would be expected in a group of men with high cholesterol values, poor physical fitness, and so on.16 The differences in risk factor distribution between those with and without coronary heart disease events during follow up (subgroups D and C, table 1) further supports this suggestion. Our findings are unlikely to have a primary pulmonary origin, as chest pain remained a strong risk indicator even after accounting for FEV1.
In relation to the second explanation, the early occurrence of clinical events also indicates that misinterpretation of the chest pain had probably often taken place at baseline. However, the survey reports sent to the company doctors for all men with this type of chest pain were flagged with a query. This should have facilitated the early recognition of “true” coronary heart disease symptoms if they developed subsequently, and would have favoured early treatment with drugs and coronary interventions rather than the reverse. The large numbers of early CABGs in group B favours this explanation and may also in part explain why it took 16 to 17 years before we observed differences in coronary heart disease mortality between groups A and B.
In relation to the third explanation, the large number of men without coronary heart disease events during 26 years of follow up also indicates that a substantial number of them probably did not have coronary chest pain, as assumed initially. The different risk factor pattern between the non-event group (C) and the event group (D) within group B (table 1) suggests that this explanation may also in part be correct. From a risk factor point of view, the subgroup of men without coronary heart disease events (group C) is identical to the group of men with no symptoms of angina (group A) (table 1).
In any observational study one should also consider the problem of confounding—that is, that factors or diseases not considered in the protocol may explain some (or most) of the survey findings. One example of such possible confounders in our study may be diabetes mellitus, which occurred more than twice as often among the 68 men with possible angina than among the 1831 men with no angina symptoms. However, in view of the large number of known coronary heart disease risk factors not accounted for, there may well be other confounding variables.
Earlier follow up studies of subjects with chest pain have mainly focused on those found during mass screening of large unselected populations and with all kinds of coronary heart disease events.2–11 Our study differs by having a selected and apparently healthy baseline population. In particular, we were careful to exclude all men with a clinical history suggesting the presence of coronary disease at baseline (see Methods). We also excluded any who had definite angina or who developed chest pain during the exercise test, or who had a pathological exercise ECG.15 Even after these primary and secondary exclusions, “possible angina” on the WHO angina questionnaire proved to be an independent warning symptom.
The possible angina group was identified by their answers to the WHO angina questionnaire, which was developed mainly for epidemiological and not for clinical purposes. In the clinical setting the questionnaire has been criticised for having low sensitivity and low specificity,17–20 translation difficulties, and between-country variation in the prevalence of chest pain as a hard indicator of coronary heart disease. Also, as the likelihood of obtaining positive responses to the questionnaire is twice as high when completed by the subject himself as when a history is taken by a trained technician or a physician,6,14,21 one may well question its clinical value. However, despite the limitations of the questionnaire, our data show that it could identify a group of apparently healthy middle aged Norwegian men with notably increased coronary heart disease mortality and morbidity during long term follow up. The data therefore suggest that “possible angina”, as defined by the WHO questionnaire, probably often represents coronary chest pain despite not fulfilling textbook descriptions of angina, and despite the presence of a normal response to a symptom limited exercise ECG. In populations with a high prevalence of endemic coronary heart disease, the WHO angina questionnaire appears therefore to define subjects who deserve to be followed carefully.
When the primary focus is on coronary heart disease mortality, our data also suggest that 10 years of follow up may be too short a period to reveal the true clinical course. Coronary atherosclerosis is, after all, a chronic and often slowly progressive degenerative/inflammatory disease.
Although the sensitivity and specificity aspects of the WHO angina questionnaire may vary considerably among countries, and point prevalence data on angina may underestimate the population burden of coronary heart disease,22 this questionnaire still seems to represent a simple, valuable, and standardised screening tool for detecting high risk populations—at least in countries or regions with a high pre-test probability of having coronary heart disease, in accordance with standard probability theory.23
APPENDIX
LONDON SCHOOL OF HYGIENE CARDIOVASCULAR QUESTIONNAIRE
Section A: Chest pain on effort
- Have you ever had any pain or discomfort in your chest?
- – Yes
- – No
- Do you get it when you walk uphill or hurry?
- – Yes
- – No
- – Never hurry
- Do you get it when you walk at an ordinary pace at the level?
- – Yes
- – No
- What do you do if you get it while you are walking?
- – Stop or slow down
- – Carry on
- If you stand still, what happens to it?
- – Relieved
- – Not relieved
- How soon?
- – 10 minutes or less
- – More than 10 minutes
- Will you show me where it was?
- – Sternum (upper or middle)
- – Sternum (lower)
- – Left anterior chest
- – Left arm
- – Other
- Do you feel it anywhere else?
- – Yes
- – No
- Did you see a doctor because of this pain (or discomfort)?
- – Yes
- – No
If yes, what did he say it was?
Diagnostic criteria for angina pectoris:
1. Yes
2. or 3. Yes
4. Stop or slow down
5. Relieved
6. 10 minutes or less
7. (a) Sternum (upper or middle, or lower), or (b) left anterior chest and left arm.
REFERENCES
- 1.Rose GA, Blackburn H. Cardiovascular survey methods. Monogr Ser WHO 1968;56:1–188. [PubMed] [Google Scholar]
- 2.Lampe FC, Whincup PH, Wannamethee SG, et al. Chest pain on questionnaire and prediction of major ischaemic heart disease events in men. Eur Heart J 1998;19:63–73. [DOI] [PubMed] [Google Scholar]
- 3.Cook DG, Shaper AG, MacFarlane PW. Using the WHO (Rose) angina questionnaire in cardiovascular epidemiology. Int J Epidemiol 1989;18:607–13. [DOI] [PubMed] [Google Scholar]
- 4.Sigurdsson E, Sigfusson N, Agnarsson U, et al. Long-term prognosis of different forms of coronary heart disease: the Reykjavik Study. Int J Epidemiol 1995;24:58–68. [DOI] [PubMed] [Google Scholar]
- 5.Zeiner-Henriksen T. Six year mortality related to cardiorespiratory symptoms and environmental risk factors in a sample of the Norwegian population. J Chron Dis 1976;29:15–33. [DOI] [PubMed] [Google Scholar]
- 6.Wilhelmsen L, Rosengren A, Hagman M, et al. “Nonspecific” chest pain associated with high long-term mortality: results from the primary prevention study in Goteborg, Sweden. Clin Cardiol 1998;21:477–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Murabito JM, Anderson KM, Kannel WB, et al. Risk of coronary heart disease in subjects with chest discomfort: the Framingham Heart Study. Am J Med 1990;89:297–302. [DOI] [PubMed] [Google Scholar]
- 8.Bulpitt CJ, Shipley MJ, Demirovic J, et al. Predicting death from coronary heart disease using a questionnaire. Int J Epidemiol 1990;19:899–904. [DOI] [PubMed] [Google Scholar]
- 9.Wilcox RG, Roland JM, Hampton JR. Prognosis of patients with “chest pain ?cause”. BMJ 1981;282:431–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Madhavan S, Cohen H, Alderman MH. Angina pectoris by Rose questionnaire does not predict cardiovascular disease in treated hypertensive patients. J Hypertens 1995;13:1307–12. [DOI] [PubMed] [Google Scholar]
- 11.Bruce RA, Hossack KF, DeRouen TA, et al. Enhanced risk assessment for primary coronary heart disease events by maximal exercise testing: 10 years’ experience of Seattle heart watch. J Am Coll Cardiol 1983;2:565–73. [DOI] [PubMed] [Google Scholar]
- 12.Erikssen J. Aspects of latent coronary heart disease. A prevalence and methodological validation study in apparently healthy, working middle aged men. Oslo: Oslo University, 1978. [Thesis.]
- 13.Sandvik L, Erikssen J, Thaulow E, et al. Physical fitness as a predictor of mortality among healthy, middle-aged Norwegian men. N Engl J Med 1993;328:533–7. [DOI] [PubMed] [Google Scholar]
- 14.Zeiner-Henriksen T. Comparison of personal interview and postal inquiry methods for assessing prevalence of angina and possible infarction. J Chron Dis 1972;25:433–40. [DOI] [PubMed] [Google Scholar]
- 15.Erikssen J, Enge I, Forfang K, et al. False positive diagnostic tests and coronary angiographic findings in 105 presumably healthy males. Circulation 1976;54:371–6. [DOI] [PubMed] [Google Scholar]
- 16.Erikssen G, Liestol K, Bjornholt J, et al. Changes in physical fitness and changes in mortality. Lancet 1998;352:759–62. [DOI] [PubMed] [Google Scholar]
- 17.Wilcosky T, Harris R, Weissfeld L. The prevalence and correlates of Rose questionnaire angina among women and men in the lipid research clinics program prevalence study population. Am J Epidemiol 1987;125:400–9. [DOI] [PubMed] [Google Scholar]
- 18.Bass EB, Follansbee WP, Orchard TJ. Comparison of a supplemented Rose Questionnaire to exercise thallium testing in men and women. J Clin Epidemiol 1989;42:385–94. [DOI] [PubMed] [Google Scholar]
- 19.Greene AF, Schocken DD, Spielberger CD. Self-report of chest pain symptoms and coronary artery disease in patients undergoing angiography. Pain 1991;47:319–24. [DOI] [PubMed] [Google Scholar]
- 20.Garber CE, Carleton RA, Heller GV. Comparison of “Rose questionnaire angina” to exercise thallium scintigraphy: different findings in males and females. J Clin Epidemiol 1992;45:715–20. [DOI] [PubMed] [Google Scholar]
- 21.Rose G, McCartney P, Reid DD. Self-administration of a questionnaire on chest pain and intermittent claudication. Br J Prev Soc Med 1977;31:42–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rose G. Variability of angina. Some implications for epidemiology. Br J Prev Soc Med 1968;22:12–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N Engl J Med 1979;300:1350–8. [DOI] [PubMed] [Google Scholar]