Abstract
This case report describes the devastating consequences of spontaneous coronary dissection in a 36 year old female patient who otherwise had a normal coronary arteriogram. Intravascular ultrasound showed coronary artery dissection and intramural haematoma at the left main stem coronary artery. Acute coronary syndrome developed and subsequently surgical revascularisation was performed successfully.
Keywords: coronary artery, left main stem, dissection, spontaneous dissection, intravascular ultrasound
Spontaneous coronary artery dissection is a rare and often fatal cause of ischaemic heart disease occurring predominantly in young or middle aged otherwise healthy patients. It is mostly recognised at postmortem examination in young victims of sudden death.1 The cause of and optimal management approach for this challenging condition are still being debated.1–10
About 250 cases of spontaneous coronary artery dissection have been reported in the literature. Spontaneous coronary artery dissection is the result of an intramural haematoma in the media of the arterial wall that creates a false lumen. Expansion of this lumen through blood or clot accumulation leads to compression of the real lumen and to myocardial ischaemia.
An intimal tear is only seldom observed. Most reports are of apparently healthy, young to middle aged patients (mean age 40 years) without overt risk for coronary artery disease and without severe coronary atheromatosis.2 More than 70% of the reported cases occurred in women.2 The aetiology remains uncertain. We present a case of a spontaneous coronary dissection in a 36 year old female patient involving the left main stem. The patient was admitted with acute coronary syndrome and ECG signs of anterior wall ischaemia. Despite optimised pharmacological treatment, recurrent ischaemia occurred. Subsequently, surgical revascularisation was performed successfully.
CASE REPORT
A previously fit 36 year old white woman was admitted with a one hour history of chest pain. Precordial discomfort started during housekeeping. The patient had a fairly unremarkable medical history. She had two healthy children. Pregnancy was excluded by β human chorionic gonadotropin testing. She used no oral contraceptives or illicit drugs. There was no history of hypertension but the patient was a current smoker (10 pack-years). On examination, her supine heart rate was 86 beats/min and blood pressure was 112/78 mm Hg. She had no clinical signs of Marfan’s syndrome or heart failure. On admission to hospital, her ECG showed ST segment elevation in the precordial leads indicating acute anterior wall myocardial infarction. Cardiac enzymes were slightly increased (creatine kinase (CK)) 204 U/l, normal range < 145 U/l; CK-MB fraction 23 U/l; troponin T 0.09 ng/ml, normal range < 0.03 ng/ml). Echocardiography showed a region of akinesia confined to the anterior wall and the apex of the left ventricle. The left ventricular lateral wall showed hypokinesia. The chest radiograph was normal. The patient was treated with aspirin, enoxaparin, metoprolol, nitrates, and opiates for acute coronary syndrome. Thirty five minutes after hospital admission urgent cardiac catheterisation was performed.
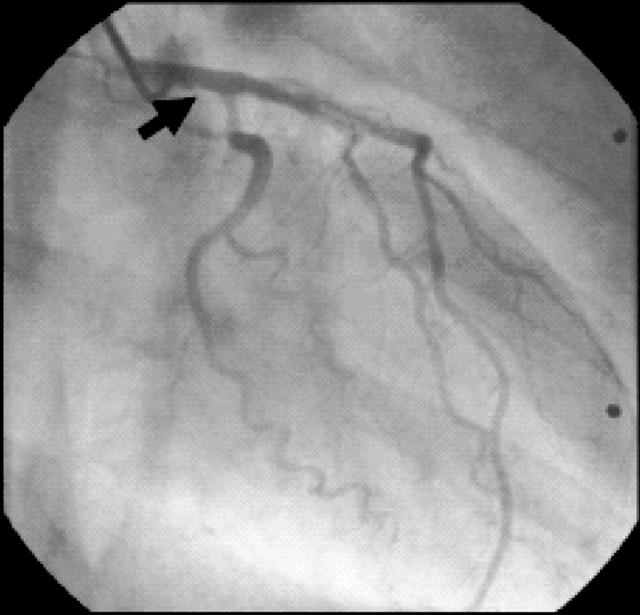
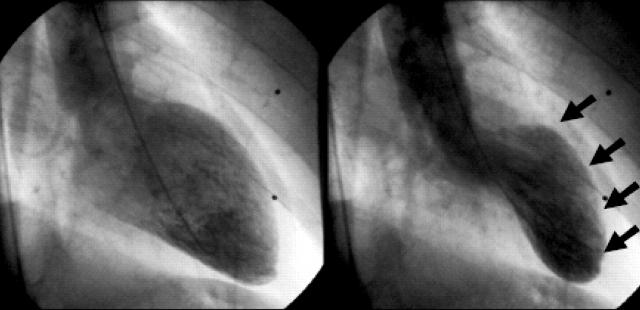
At coronary angiography she was found to have dissection of the left main stem (fig 1), no stenotic lesions, and TIMI (thrombolysis in myocardial infarction) flow grade 3. Left ventriculography showed moderately depressed left ventricular function and akinesia confined to the anterior and apical walls of the left ventricle (fig 2). Clopidogrel was added and chest pain resolved early after coronary angiography. Maximum CK concentration was 346 U/l (MB fraction 33 U/l). Twenty four hours later, repeated echocardiography showed only a limited region of hypokinesia confined to the left ventricular apex.
Figure 1.
Coronary angiography in the right anterior oblique position with a left Judkins (JL4) catheter showing irregularity of the left main coronary artery suggesting dissection (arrow), no stenotic lesions, and TIMI flow grade 3.
Figure 2.
Left ventriculography (left: diastolic view; right: systolic view; right anterior oblique projection) showing moderately depressed left ventricular function and akinesia confined to the anterior and apical wall of the left ventricle (arrows).
Chest pain at rest recurred 48 hours after admission and ECG again showed ST segment elevation in the precordial leads indicating transmural acute anterior wall ischaemia. Precordial pain and ECG changes resolved within 90 minutes with tirofiban and intravenous nitrates.
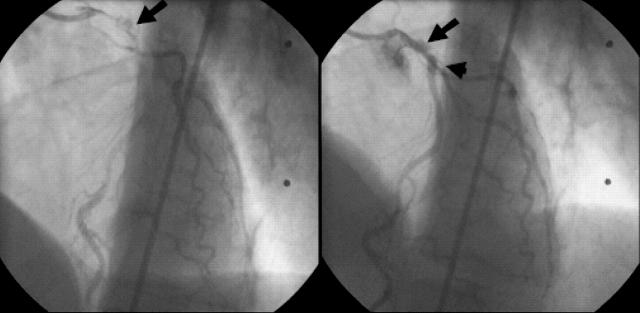
CK values were increased with a peak concentration of 638 U/l (MB fraction 96 U/l). Coronary angiography was repeated and showed disease progression and extension of the dissection to both the left anterior descending and the left circumflex arteries with subtotal occlusion and TIMI flow grade 1 of the first diagonal branch (fig 3). Intravascular ultrasound showed dissection and intramural haematoma starting from the left coronary ostium and progressing into the left anterior descending and the circumflex arteries. Intramural haematoma in the media of the arterial wall resulted in compression of the real lumen (fig 4) and myocardial ischaemia. An intimal tear was not observed. Recurrent myocardial ischaemia prompted emergency coronary artery bypass grafting (left internal mammary artery graft to the left anterior descending and vein grafts to the diagonal and circumflex arteries). The patient made an uneventful recovery.
Figure 3.
Coronary angiography in the left anterior oblique position with a left Judkins (JL4) catheter showing a lesion corresponding to a dissection of the left main stem (arrows) extending to the left anterior descending and circumflex coronary arteries and subtotal occlusion and TIMI flow grade 1 of the first diagonal branch (arrowhead).
Figure 4.
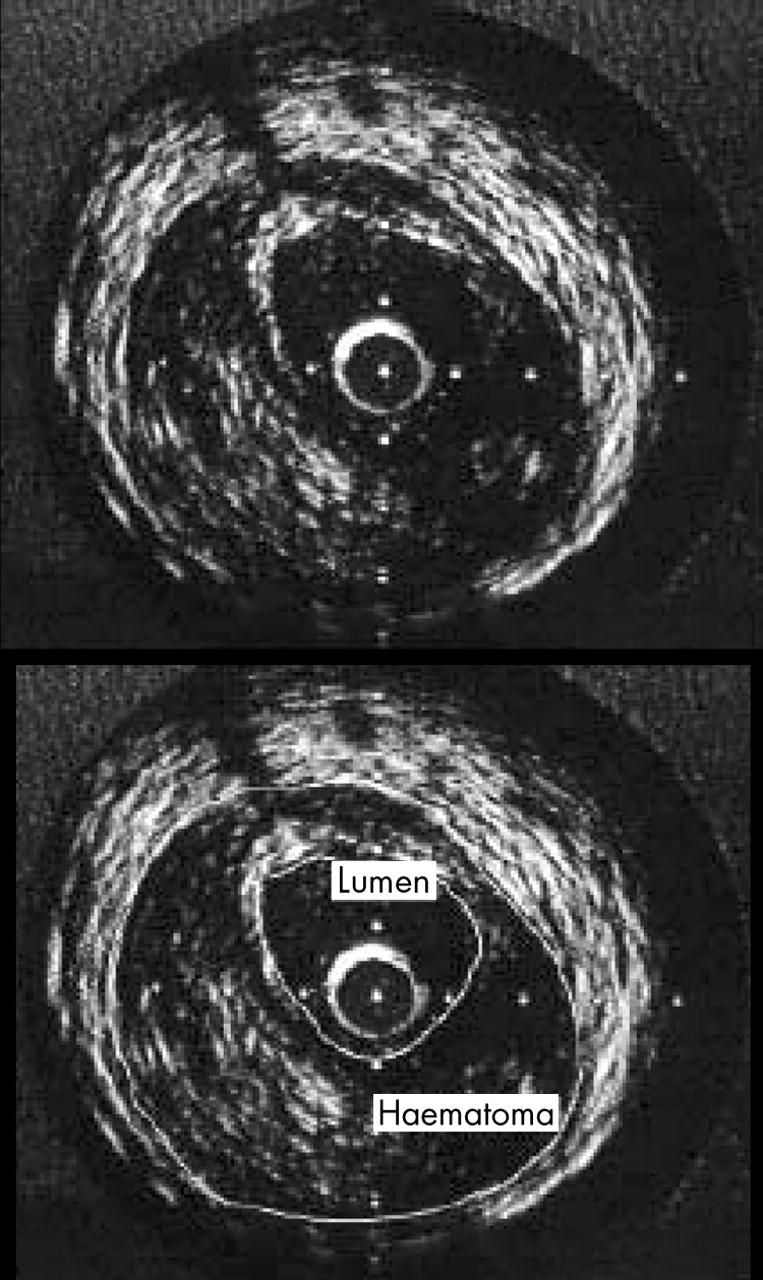
Intravascular ultrasound showing dissection and intramural haematoma starting from the left coronary ostium and progressing into the left anterior descending and the circumflex arteries. Intramural haematoma in the media of the arterial wall resulted in compression of the real lumen. An intimal tear was not observed.
DISCUSSION
Spontaneous coronary artery dissection was first described at postmortem examination in a 42 year old woman more than 70 years ago.11 It is a rare entity, mostly recognised at postmortem examination in young victims of sudden death.2 It is the result of an intramural haematoma in the media of the arterial wall that creates a false lumen. Expansion of this lumen through blood or clot accumulation leads to compression of the real lumen and myocardial ischaemia.
Most reports are of apparently healthy, young to middle aged women without overt risk for coronary artery disease and without severe coronary atheromatosis.2 In general, this disease is associated with a high mortality.2
About one in four female patients with spontaneous coronary artery dissection are in the peripartum period. Contraceptives and the exceptional hormonal balances in the peripartum period are supposed to weaken the arterial wall and to predispose it to rupture or dissection. Spontaneous coronary artery dissection has also been described in patients with Marfan’s syndrome, with cocaine misuse, and after intense physical exercise.2,4,5,12
In women with spontaneous coronary dissection, there is a predilection for the left coronary system, whereas in men the right coronary artery is affected in about two thirds of cases.13
The aetiology and pathogenesis of spontaneous coronary artery dissection are poorly understood and remain uncertain. In the absence of an intimal tear, primary disruption of the vasa vasorum and subsequent haemorrhage into the media of the arterial wall (similar to aortic dissection) have been proposed as an underlying mechanism.13 Several papers reported the presence of periadventitial inflammatory infiltrates, with frequent preponderance of eosinophils.6 Such infiltrates may weaken the arterial wall and may induce vulnerability of the arterial wall secondary to the release of cytokines and proteolytic enzymes. The underlying disease may be primary vasculitis or abnormal tissue fragility (similar to Marfan’s syndrome) with localised injury. The patient described in the present case report had no stigmata of Marfan’s syndrome.
Cystic medial necrosis of the coronary arteries is a rare finding.1,7,8,13 Focal fragmentation of elastic fibres and loss of smooth muscle cells of the media are present.
Similar lesions can be found in the ascending aorta of patients with Marfan’s syndrome that may predispose them to aortic dissection. Additionally, chronic injury in case of long lasting arterial hypertension may result in cystic medial lesions of great vessels in elderly patients. The patient described in the present case report had no history of hypertension.
Spontaneous coronary artery dissection is associated with a high mortality due to severe myocardial ischaemia that often leads to sudden death.2 Nevertheless, medical management is safe and compatible with good long term survival in patients surviving the initial episode and who subsequently remain asymptomatic.12,14
Ongoing ischaemia refractory to medical management should prompt urgent revascularisation. The available modalities should depend on the area at risk, the number of vessels involved, and the persistence of myocardial ischaemia.9,14 Thrombolytic treatment may be effective in lysing a compressing intramural clot but it may also contribute to the expansion of an intramural haematoma. Thrombolysis may be useful in arteries where intramural haematoma is compressing the true lumen, allowing the latter to re-expand.12
In the absence of severe left ventricular impairment, symptomatic patients with single vessel dissection not involving the left main coronary artery may benefit from primary coronary stenting to decrease the chance of sudden death, reinfarction, and arrhythmia.15,16 With a complicated dissection involving thrombus and a nearly occluded lumen, however, this approach may be difficult with sometimes devastating consequences.
Coronary artery bypass grafting is recommended for patients with dissection involving the left main stem and for patients with ongoing myocardial ischaemia refractory to medical treatment.17 Although surgical revascularisation in case of multivessel and left main stem coronary artery involvement seems to be the most controlled strategy, the anastomosis of a graft circuit on a dissected coronary artery may be hazardous.
In the case of severe heart failure, bridging to heart transplantation can be the most reasonable choice.13
In conclusion, the case described here shows that spontaneous coronary artery dissection is an important cause of myocardial ischaemia and infarction preferentially in young women without overt risk for coronary artery disease. Prompt diagnosis with coronary angiography and treatment with coronary artery revascularisation in patients with ongoing myocardial ischaemia that is refractory to medical management provides the only means of improving survival in this serious disease.
REFERENCES
- 1.Basso C , Morgagni GL, Thiene G. Spontaneous coronary artery dissection: a neglected cause of acute myocardial ischemia and sudden death. Heart 1996;75:451–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jorgensen MB, Aharonian V, Mansukhani P, et al. Spontaneous coronary dissection: a cluster of cases with this rare finding. Am Heart J 1994;127:1382–7. [DOI] [PubMed] [Google Scholar]
- 3.Klutstein MW, Tzivoni D, Bitran D, et al. Treatment of spontaneous coronary artery dissection: report of three cases. Cathet Cardiovasc Diagn 1997;40:372–6. [DOI] [PubMed] [Google Scholar]
- 4.Jaffe BD, Broderick TM, Leier CV. Cocaine-induced coronary-artery dissection. N Engl J Med 1994;330:510–1. [DOI] [PubMed] [Google Scholar]
- 5.Sherrid MV, Mieres J, Mogtader A, et al. Onset during exercise of spontaneous coronary artery dissection and sudden death: occurrence in a trained athlete: case report and review of prior cases. Chest 1995;108:284–7. [DOI] [PubMed] [Google Scholar]
- 6.Siegel RJ, Koponen M. Spontaneous coronary artery dissection causing sudden death: mechanical arterial failure or primary vasculitis? Arch Pathol Lab Med 1994;118:196–8. [PubMed] [Google Scholar]
- 7.Adkins GF, Steele RH. Left coronary dissection: an unusual presentation. Br Heart J 1986;55:411–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Glasgow BJ, Tift JP, Alexander C. Spontaneous primary dissecting coronary artery aneurysm: report of two cases. Am J Forensic Med Pathol 1984;5:155–9. [DOI] [PubMed] [Google Scholar]
- 9.Zampieri P , Aggio S, Roncon L, et al. Follow-up after spontaneous coronary artery dissection: a report of five cases. Heart 1996;75:206–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Borczuk AC, Hoeven KH, Factor SM. Review and hypothesis: the eosinophil and peripartum heart disease (myocarditis and coronary artery dissection): coincidence or pathogenetic significance? Cardiovasc Res 1997;33:527–32. [DOI] [PubMed] [Google Scholar]
- 11.Pretty HC. Dissecting aneurysm of coronary artery in a woman aged 42. BMJ. 1931;i :667.
- 12.Missouris CG, Ring A, Ward D. A young woman with chest pain. Heart 2000;84:e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Conraads VM, Vorlat A, Colpaert CG, et al. Spontaneous dissection of three major coronary arteries subsequent to cystic medial necrosis. Chest 1999;116:1473–5. [DOI] [PubMed] [Google Scholar]
- 14.Chun JH, Lee SC, Gwon HC, et al. Left main coronary artery dissection after blunt chest trauma presented as acute anterior myocardial infarction: assessment by intravascular ultrasound: a case report. J Korean Med Sci 1998;13:325–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Porras MC, Ares MA, Zucco J. Intracoronary stenting for postpartum coronary artery dissection. Ann Intern Med 1998;128:873. [DOI] [PubMed] [Google Scholar]
- 16.Hong MK, Satler LF, Mintz GS. Treatment of spontaneous coronary artery dissection with intracoronary stenting. Am Heart J 1996;132:200–2. [DOI] [PubMed] [Google Scholar]
- 17.Thistlewaite PA. Surgical management of spontaneous left main coronary artery dissection. Ann Thorac Surg 1998;45:258–60. [DOI] [PubMed] [Google Scholar]