Abstract
Objectives: To compare initial and one year costs of coronary artery bypass grafting (CABG) versus percutaneous coronary intervention (PCI) in the stent or surgery trial.
Design: Prospective, unblinded, randomised trial.
Setting: Multicentre study.
Patients: 988 patients with multivessel disease.
Interventions: CABG and stent assisted PCI.
Main outcome measures: Initial hospitalisation and one year follow up costs.
Results: At one year mortality was 2.5% in the PCI arm and 0.8% in the CABG arm (p = 0.05). There was no difference in the composite of death or Q wave myocardial infarction (6.9% for PCI v 8.1% for CABG, p = 0.49). There were more repeat revascularisations with PCI (17.2% v 4.2% for CABG). There was no significant difference in utility between arms at six months or at one year. Quality adjusted life years were similar 0.6938 for PCI v 0.6954 for PCI, Δ = 0.00154, 95% confidence interval (CI) −0.0242 to 0.0273). Initial length of stay was longer with CABG (12.2 v 5.4 days with PCI, p < 0.0001) and initial hospitalisation costs were higher (£7321 v £3884 for PCI, Δ = £3437, 95% CI £3040 to £3848). At one year the cost difference narrowed but costs remained higher for CABG (£8905 v £6296 for PCI, Δ = £2609, 95% CI £1769 to £3314).
Conclusions: Over one year, CABG was more expensive and offered greater survival than PCI but little added benefit in terms of quality adjusted life years. The additional cost of CABG can be justified only if it offers continuing benefit at no further increase in cost relative to PCI over several years.
Keywords: coronary angioplasty, coronary bypass surgery, health care cost
From the late 1980s to the early 1990s percutaneous transluminal coronary angioplasty (PTCA) was compared with coronary artery bypass grafting (CABG) for multivessel coronary artery disease in six major randomised clinical trials and in a meta-analysis of the available trials.1–7 The results of these trials have largely been consistent in terms of clinical outcome. Overall, there was little difference in death or myocardial infarction but more revascularisation procedures were performed in the PTCA arm during follow up.
More recently, in the late 1990s to 2001, CABG was compared with percutaneous coronary intervention (PCI) in three trials.8–10 In these more recent trials, results also were shown to be consistent in the composite of death or myocardial infarction. However, these three trials were considerably heterogeneous in term of mortality—that is, there was no difference in the rate of death between CABG and PCI in the ARTS (arterial revascularisation therapies study),8 mortality was significantly lower with PCI in ERACI II (Argentine randomised trial of percutaneous transluminal coronary angioplasty versus coronary artery bypass surgery in multivessel disease),9 and mortality was lower with CABG in the stent or surgery (SoS) trial.10 These trials also showed a decrease in the rate of repeat revascularisation after PCI compared with balloon angioplasty alone. Economic analyses conducted for several of these trials have shown that, at one to five years, much of the initial cost advantage of PTCA is lost during follow up due to the cost of additional procedures in the PTCA group.8,11–16 The purpose of the present study was to compare the economic outcome, focusing on one year cost, of PCI with stent implantation versus CABG in the SoS trial.
METHODS
Patient population
SoS is a multicentre randomised trial comparing PCI with CABG. Eligibility criteria are available in the clinical outcomes publication.10 A total of 988 patients (488 assigned to PCI and 500 to CABG) were enrolled between 1996 and 1999 from 11 European countries and Canada with 40% of patients from the UK. All patients were followed up for one year. All coronary stenting and CABG procedures were performed with standard techniques in use during the time of the study.
Data collection and costing
Demographic, clinical, angiographic, and procedural data, as well as data relating to complications and resource use over the course of follow up, were recorded prospectively on standardised forms and entered on to a computerised database. Costs were estimated by applying publicly available British unit costs to resource use for each patient in the trial.
Length of stay, measured from the time of admission, was recorded for all hospitalisations throughout the study and costed according to nationally relevant estimates of hospitalisation costs by ward type and day case procedure taken from published sources.17,18 Additional resource use data collected for the index hospitalisation were consumables and staff time associated with PCI procedures, which were costed according to published studies and supplementary data from hospitals and manufacturers.19,20 CABG was costed as the average cost of a general CABG procedure adjusted for observed length of stay.21 Additional costs associated with complications of stroke and bleeding were estimated from an unpublished clinician survey of several hospitals in the UK.19,22 No additional costs were added for myocardial infarctions associated with revascularisation procedures because any additional costs were assumed to be accounted for in the observed data on length of stay, staff time, and consumables.
Information collected for all rehospitalisations included associated diagnoses, procedures performed, and associated pre-specified complications (myocardial infarction, stroke, bleeding). CABG and PCI procedures, myocardial infarction associated with revascularisations, and stroke and bleeding complications were costed as for the index hospitalisation; costs of admissions for other reasons were taken from the National Health Service reference costs and from previously published studies and adjusted for observed length of stay.19,20,23 For symptomatic Q wave myocardial infarctions occurring during a hospitalisation that were not associated with a revascularisation procedure, additional costs of non-interventional management were added to the observed length of stay costs. Costs associated with pharmaceutical use during the course of follow up were taken from the British National Formulary.24 A price base year of 2000 was used, with published estimates from earlier years being up-rated based on the Hospital and Community Health Services price index.25
Utility, an overall measure of health related quality of life, was measured by the EQ-5D classification at baseline, six months, and 12 months.26 The “social tariff” for the EQ-5D, estimated from a representative sample of the British population, was applied to each patient’s self reported classification across the five EQ-5D dimensions.27
Statistical analyses
Data are expressed as proportions or as mean with 95% confidence interval (CI) for non-normal continuous data. The two randomised arms were compared according to intention to treat. Follow up for mortality and repeat procedures was complete to one year or to the time of death for all patients. Differences in categorical variables were analysed by the χ2 test (or Fisher’s exact test) and differences in continuous variables were analysed by the Wilcoxon rank sum test. Because the cost data were not normally distributed, a resampling approach (5000 samples) was taken to obtain confidence intervals for the cost differences by using the empirical precentiles of the bootstrap distribution.28 Missing utility data were estimated by multiple imputation.29 Quality adjusted life years were calculated as the area under the utility curve from baseline to one year or time of earlier death. Statistical analysis was performed with SAS (SAS Institute, Cary, North Carolina, USA) and S-Plus (MathSoft Inc, Seattle, Washington, USA).
RESULTS
At one year the mortality rate was lower for the surgical group (0.8% v 2.5%, p = 0.05), but there was no difference in the composite of death plus Q wave myocardial infarction (6.9% for PCI v 8.1% for CABG, p = 0.49). Repeat revascularisation was significantly greater in the PCI arm (17.2% v 4.2%, p < 0.001).
Table 1 shows initial hospitalisation resource utilisation and unit costs. The majority of patients had their initial revascularisation procedure as planned, with a small number of crossovers. Resources are divided into PCI consumables and laboratory time, CABG, hospital length of stay, and adverse events. Length of stay, calculated as the number of days the patients spent in the intensive care unit, high dependency unit, and general ward, was longer in the CABG arm. Average postprocedural and total in-hospital stays were 8.7 days and 12.2 days for CABG and 2.7 days and 5.4 days for PCI. There were also more investigator reported myocardial infarctions in the PCI arm but more bleeding in the CABG arm. There was no difference in the incidence of stroke. During the initial hospitalisation there were more additional catheterisations and revascularisations in the PCI arm (table 2).
Table 1.
Average resource use per patient, unit cost, and average cost per patient during initial hospitalisation by treatment group*
| Resource | Average resource use | Unit costs (£) | Average cost (£) | ||
| PCI (n = 488) | CABG (n = 500) | PCI (n = 488) | CABG (n = 500) | ||
| Consumables for PCI | |||||
| Laboratory time (min) | 96.09 | 1.68 | 1.62 | 155.7 | 2.7 |
| Amount of contrast used (ml) | 380.82 | 7.06 | 0.15 | 57.1 | 1.1 |
| Number of guide catheters used | 2.05 | 0.04 | 36.62 | 74.9 | 1.5 |
| Number of guidewires used | 2.03 | 0.04 | 54.38 | 110.2 | 2.0 |
| Number of balloons used | 2.43 | 0.04 | 186.00 | 452.0 | 7.1 |
| Number of IVUS catheters used | 0.05 | 0 | 495.00 | 23.3 | 0 |
| Number of stents used | 2.57 | 0.04 | 553.00 | 1421.0 | 24.3 |
| Abciximab (vial) | 0.246 | 0 | 280.00 | 68.9 | 0 |
| Tirofiban (vial) | 0.025 | 0 | 146.11 | 3.6 | 0 |
| Number of AngioSeal devices used | 0.02 | 0 | 72 | 1.6 | 0 |
| Number of IABP procedures | 0.01 | 0 | 445 | 4.6 | 0 |
| Number of Rotablators used | 0.01 | 0 | 1007.73 | 12.4 | 0 |
| Number of Rotablator 1.25 and 1.75 | 0.004 | 0 | 1451.61 | 5.9 | 0 |
| CABG (excluding length of hospital stay) | 0.014 | 0.97 | 3403.14 | 48.8 | 3314.7 |
| Hospitalisation length of stay (days) | |||||
| Intensive care unit | 0.34 | 1.84 | 976.62/day | 330.1 | 1796.4 |
| High dependency unit | 0.61 | 0.92 | 557.12/day | 342.3 | 510.9 |
| General ward | 4.50 | 9.49 | 169.49/day | 762.6 | 1608.5 |
| Adverse events (excluding length of hospital stay) | |||||
| Non-fatal myocardial infarction† | 0.039 | 0.016 | 885.00 | 0 | 0 |
| Stroke | 0.01 | 0.01 | 533.91 | 3.3 | 5.3 |
| Bleeding at vascular puncture site from cardiovascular procedure | 0.006 | 0.002 | 153.86 | 0.9 | 0.3 |
| Bleed at gastrointestinal site | 0.002 | 0.004 | 517.00 | 1.1 | 2.1 |
| Bleeding after surgery or other procedure | 0.002 | 0.026 | 1673.74 | 3.4 | 43.5 |
*Resource use presented only for initial hospitalisation; same unit costs used for repeat revascularisation.
†Additional costs included only for myocardial infarctions not associated with a revascularisation procedure.
CABG, coronary artery bypass grafting; IABP, intra-aortic balloon pump; IVUS, intravascular ultrasound; PCI, percutaneous coronary intervention.
Table 2.
Initial and follow up resource utilisation
| PCI (n = 488) | CABG (n = 500) | p Value | |
| Initial hospitalisation | |||
| Revascularisation as planned | 480 (98.4%) | 487 (97.4%) | 0.30 |
| Crossover revascularisation | 7 (1.4%) | 11 (2.2%) | 0.37 |
| Additional catheterisation | 5 (1.0%) | 0 (0%) | 0.029 |
| Additional CABG | 6 (1.2%) | 4 (0.8%) | 0.542 |
| Additional PCI | 6 (1.2%) | 0 (0.0%) | 0.014 |
| Rehospitalisation* | |||
| Repeat PCI | 56 | 18 | <0.0001 |
| Repeat CABG | 32 | 1 | <0.0001 |
| Cardiac catheterisation only | 62 | 11 | <0.0001 |
| Myocardial infarction | 11 | 3 | 0.028 |
| Stroke | 4 | 3 | 0.72 |
| Bleeding | 0 | 1 | 1.0000 |
| Other reasons for hospitalisation† | 64 | 131 | <0.0001 |
| Mean time in rehabilitation (days) | 0.85 | 2.36 | <0.0001 |
| 95% confidence interval | 0.42 to 1.44 | 1.78 to 3.01 |
*Total number of events.
†Other reasons (frequency) are as follows. For PCI arm: chest pain—cardiac (20), gastrointestinal (7), chest pain—non-cardiac (6), other—specify (6), genitourinary/gynaecological (4), vascular—other (4), haematological/lymphatic (2), musculoskeletal (2), respiratory (2), transient ischaemic accident (2), unable to classify (2), cancelled procedure (1), cardiac—other (1), cardiac arrhythmias—supraventricular/atrial fibrillation/atrial flutter (1), cardiac failure (1), ear, nose, throat (1), effusion—pericardial (1), ophthalmological (1). For CABG arm: cardiac arrhythmias—supraventricular/atrial fibrillation/atrial flutter (13), chest pain—cardiac (12), respiratory (12), chest pain—non-cardiac (10), effusion—pleural (10), other—specify (10), gastrointestinal (8), musculoskeletal (8), genitourinary/gynaecological (7), cardiac—other (5), vascular—other (5), cardiac arrhythmias—complete heart block/bradycardia (4), surgical wound—infection of sternum (4), unable to classify (4), ear, nose, throat (3), neurological (3), surgical wound—infection of other site (3), vascular—deep vein thrombosis/pulmonary embolism (3), surgical wound—unstable sternum (2), cancelled procedure (1), cardiac arrhythmias—ventricular tachycardia/ventricular fibrillation/arrest (1), cardiac failure (1), dermatological (1), transient ischaemic accident (1).
During follow up there were more repeat revascularisation procedures and additional cardiac catheterisations in the PCI arm (table 2). There were also more investigator reported myocardial infarctions during follow up in the PCI arm. There was no difference noted in the incidence of stroke or bleeding. The incidence of other hospitalisations and mean time in rehabilitation was higher in the CABG arm.
Table 3 summarises rehabilitation and medications. Medications usage and cost, in particular the use of the antiplatelet agents ticlopidine and clopidogrel, as well as oral nitrates and calcium blockers, were greater in the PCI arm.
Table 3.
Average resource use for rehabilitation and outpatient medication use during one year follow up by treatment group
| Resource | Average resource use (days) | Unit costs (£/day) | Costs (£) | ||
| PCI (n = 488) | CABG (n = 500) | PCI (n = 488) | CABG (n = 500) | ||
| Rehabilitation | |||||
| Other hospital for rehabilitation or further treatment | 0.819 | 2.321 | 175 | 143.3 | 406.1 |
| Residential or nursing home care on a temporary basis | 0.029 | 0.042 | 53.97 | 1.5 | 2.3 |
| Medication | |||||
| Antiplatelet | |||||
| Aspirin | 347.72 | 332.08 | 0.05 | 17.40 | 16.60 |
| Ticlopidine | 81.72 | 20.13 | 3.34 | 272.94 | 67.23 |
| Other (clopidogrel) | 20.86 | 3.79 | 0.59 | 12.31 | 2.24 |
| Other (dipyridamole) | 0.20 | 7.02 | 0.11 | 0.02 | 0.77 |
| Anticoagulants | |||||
| Warfarin | 4.18 | 11.34 | 0.11 | 0.46 | 1.25 |
| Heparin | 0 | 1.84 | 3.44 | 0 | 6.33 |
| Low molecular weight heparin (dalteparin sodium) | 4.78 | 2.42 | 11.30 | 54.01 | 27.35 |
| Antianginal agents | |||||
| β Blockers (atenolol) | 215.30 | 178.24 | 0.03 | 6.46 | 5.35 |
| Calcium channel antagonists (diltiazem) | 132.65 | 75.76 | 0.30 | 39.80 | 22.73 |
| Nitrates (isosorbide mononitrate) | 151.20 | 53.75 | 0.40 | 60.48 | 21.50 |
| Potassium channel activators (nicorandil) | 9.93 | 1.39 | 0.26 | 2.58 | 0.36 |
| Lipid lowering agents | |||||
| Fibrates (bezafibrate) | 23.94 | 19.57 | 0.20 | 4.79 | 3.91 |
| HMG-CoA reductase inhibitors (simvastatin) | 231.41 | 194.02 | 1.06 | 245.29 | 205.66 |
| Other (nicotinic acid) | 1.16 | 0 | 1.11 | 1.29 | 0 |
| Other cardiac treatment | |||||
| ACE inhibitor (lisinopril) | 113.52 | 89.59 | 0.65 | 73.79 | 58.23 |
| Diuretics (furosemide) | 56.56 | 93.19 | 0.08 | 4.52 | 7.46 |
| Digoxin | 6.61 | 15.13 | 0.02 | 0.13 | 0.30 |
| Antiarrhythmic (amiodarone) | 6.62 | 12.24 | 0.23 | 1.52 | 2.82 |
| Antiarrhythmic (propafenone) | 0.42 | 1.88 | 0.71 | 0.30 | 1.33 |
| Antiarrhythmic—β blocker (sotalol hydrochloride) | 0.79 | 1.01 | 0.18 | 0.14 | 0.18 |
| Antiarrhythmic—calcium channel antagonist (verapamil) | 0.65 | 0 | 0.30 | 0.20 | 0 |
| Other cardiac agents | |||||
| Antihypertensive (clonidine hydrochloride) | 0.31 | 0 | 0.17 | 0.05 | 0 |
| α Adrenoceptor blocker (doxazosin) | 3.63 | 0.88 | 0.63 | 2.29 | 0.55 |
| α Adrenoceptor blocker (indoramin) | 0 | 0.15 | 0.40 | 0 | 0.06 |
| Angiotensin II antagonist (candesartan cilexetil) | 2.54 | 2.06 | 0.53 | 1.35 | 1.09 |
| Angiotensin II antagonist (irbesartan) | 0.36 | 1.04 | 0.59 | 0.21 | 0.61 |
| Angiotensin II antagonist (losartan potassium) | 2.34 | 1.69 | 0.62 | 1.45 | 1.05 |
| Angiotensin II antagonist (valsartan) | 0.72 | 0 | 0.56 | 0.40 | 0 |
ACE, angiotensin converting enzyme; HMG-CoA, hydroxymethyl glutaryl coenzyme A.
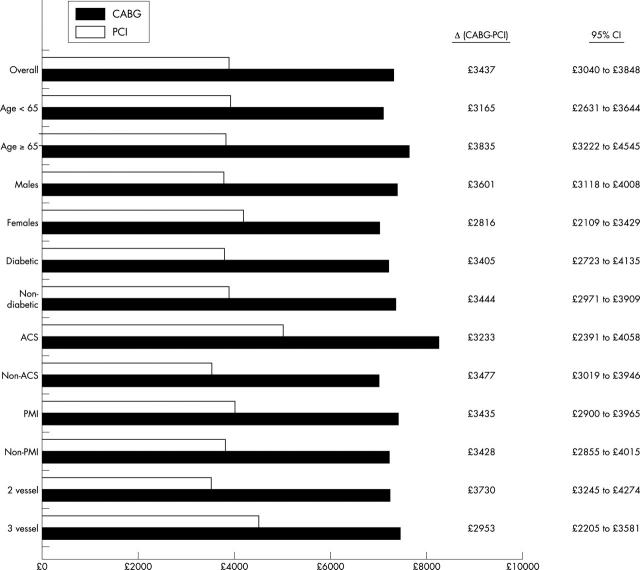
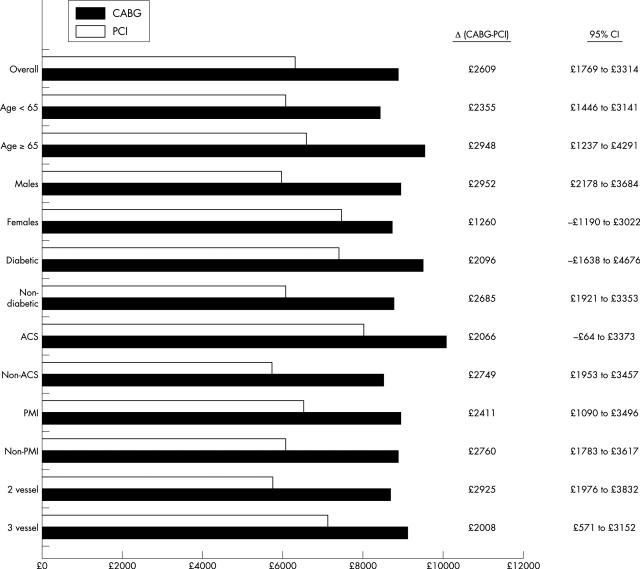
Table 4 summarises costs. Initial hospitalisation costs were higher in the CABG arm. These higher initial costs are largely attributable to higher costs associated with the procedure and longer stay in the intensive care unit and wards. Higher initial hospitalisation costs were found for CABG in each of the major subgroups (according to age, sex, presence of diabetes, presence of an acute coronary syndrome, history of a previous myocardial infarction, and number of diseased coronary vessels) (fig 1). Follow up costs were higher overall for PCI because of higher rehospitalisation and medication costs. Costs for rehabilitation were higher with CABG. The total cost at one year remained higher with CABG, both overall and for each of the major subgroups (fig 2). There was a significant advantage to CABG over PCI in life years gained (0.9943 v 0.9805, Δ = 0.0138, 95% CI 0.0012 to 0.0268), with the difference in mean life years between groups translating into five days over the one year follow up. Utility was missing, and thus imputed, at one or more of the three time points for 30% of the overall sample. There was no significant difference in utility found at any of the three time points during the first year for both the imputed and the unimputed data. The difference between treatment groups in quality adjusted life years at one year was very small and non-significant (0.6954 for CABG v 0.6938 for PCI, Δ = 0.00154, 95% CI −0.0242 to 0.0273), with a point estimate translating into 13 hours, favouring CABG. The cost per life year gained for CABG compared with PCI in the first year is £189 982 (95% CI £75 654 to £1 064 986).
Table 4.
Initial, follow up, and total costs
| PCI (n = 488) | CABG (n = 500) | Δ(CABG−PCI) | 95% CI | |
| Initial hospitalisation costs (£) | 3884 | 7321 | 3437 | 3040 to 3848 |
| Procedure costs (£) | 2440 | 3353 | 913 | 804 to 1018 |
| Ward costs (£) | 1435 | 3915 | 2480 | 2105 to 2839 |
| Complication costs (£) | 9 | 51 | 42 | 19 to 69 |
| One year follow up costs (£) | 2412 | 1584 | −828 | −1436 to −332 |
| Rehospitalisation costs (£) | 1463 | 721 | −742 | −1263 to −308 |
| Rehabilitation costs (£) | 145 | 408 | 263 | 120 to 396 |
| Medication costs (£) | 804 | 455 | −349 | −405 to −295 |
| Total one year costs (£) | 6296 | 8905 | 2609 | 1769 to 3314 |
Figure 1.
Initial hospitalisation costs for the percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG) arms in major subgroups. ACS, acute coronary syndromes; CI, confidence interval; PMI, previous myocardial infarction.
Figure 2.
Total one year costs for the PCI and CABG arms in major subgroups.
DISCUSSION
CABG offered significantly lower mortality and less angina at one year10 but the increase in quality adjusted life years compared with PCI was negligible and came at a considerable increase in cost, at least in the first year. Greater follow up costs associated with PCI were not enough to make up for the higher initial hospitalisation costs with CABG. Exploratory subgroup analyses suggest that these differences are consistent for all the obvious subgroups.
The mortality results, with CABG being significantly better than PCI, probably reflect the play of chance. In the ARTS trial, the one year mortality rate for both PCI and CABG was the same as the PCI mortality in the present trial.8 In contrast, ERACI II showed a significant survival benefit for stenting.9 This considerable uncertainty about what the real difference is in mortality and in utility between CABG and PCI makes problematic a formal estimate of a one year time horizon, as well as long term incremental cost effectiveness analysis. The in-trial mortality advantage for CABG would result in a favourable incremental cost effectiveness ratio in cost per life year saved extended long term. However, whether this result may be considered meaningful depends entirely on the generalisability of the mortality data in this trial, which favoured CABG.
Other randomised trials comparing PCI with CABG have been carried out during the past 15 years. In the RITA-1 (randomised intervention treatment of angina) trial, 1011 patients with coronary artery disease (45% single vessel, 55% multivessel) were randomly assigned between May 1988 and November 1991 to an initial strategy of PTCA or CABG.1,14 No difference was noted in the incidence of death or the composite of death plus myocardial infarction. There were more repeat interventions and a greater degree of angina in the PTCA group. Total health care costs over five years, derived by similar methods to those used for SoS, were not significantly different between groups (mean difference £426, 95% CI −£383 to £1235, p = 0.30).14 BARI (bypass angioplasty revascularisation investigation) and EAST (Emory angioplasty versus surgery trial) compared state of the art PTCA with CABG from the late 1980s.2,3 In each of these studies there was similar survival in both arms but more revascularisations with PTCA. While both studies reported higher costs initially with CABG, this cost difference narrowed over five years in BARI and over eight years in EAST.12,16 Both PTCA (or PCI) and CABG have changed dramatically since the time of those trials, especially with the introduction of coronary stents30,31 and minimally invasive or off pump CABG.32 Costs, on an inflation adjusted basis, have fallen, at least in one study from the USA, for both forms of coronary revascularisation.33,34 The older trials that compared balloon PTCA with CABG are less relevant to the current situation, in which the standard practice of PCI has come to include the use of intracoronary stents and glycoprotein IIb/IIIa inhibitors. The other major multinational trial with an economic analysis besides SoS that has been conducted since the late 1990s, comparing PCI with CABG, is ARTS.8 In ARTS, costs were similar to those in SoS. The in-hospital costs averaged $10 652 (£7531) with CABG and $6441 (£4553) with PCI, a difference of $4212 (£2977) (p < 0.001). This difference narrowed due to repeat revascularisation in the PCI arm to a one year cost of $13 638 (£9638) with CABG and $10 665 (£7537) with PCI, a difference of $2973 (£2101) (p < 0.001).
A potential change in the practice of PCI in the near future may have economic as well as clinical consequences. In early trials, drug eluting stents have been shown to reduce dramatically the restenosis rate after PCI.35,36 If these early results are borne out and restenosis is largely eliminated, then the economic advantage of CABG over PCI during follow up may be attenuated. However, any economic advantage in follow up may not overcome increased initial costs if these new stents are expensive. While this technical advance may shift decision making further towards PCI, its economic consequences remain uncertain.
As important as changes in revascularisation are, medical treatment has also changed, with efforts to control risk factors aggressively, including lipids, blood pressure, diabetes, exercise, diet, and smoking cessation. This will be addressed in detail in the COURAGE (clinical outcomes utilising revascularisation and aggressive drug evaluation) trial that began enrolment in June 1999 and will compare coronary intervention with aggressive medical management versus aggressive medical management alone.37 Changes in medical treatment will also have profound economic consequences with cost of more intense treatment offset by savings from reduced events.
Given the availability of only one year outcomes for all patients in SoS, the conclusions are inherently limited. In addition, CABG is, in the absence of complications, associated with a more difficulty period of recovery. While this was not captured in the utility data, as the first postprocedural measurement was at six months, such a difference is short lived and unlikely to translate into a substantial difference in quality adjusted life years. Both forms of revascularisation appear to be good forms of treatment for angina. While CABG offers better relief of chest pain initially, with time and additional procedures as needed, patients treated with PCI can achieve similar results. For patients equally suitable to either procedure, CABG is initially much more expensive, but this difference may be reduced or disappear over time if additional procedures are performed in the PCI arm. CABG may look more favourable in the longer term, as there will be little reason to expect greater long term induced costs with CABG than with PCI, and over several years patients who have undergone CABG may continue to have less angina.16,38 Thus, the in-trial ratio of cost per life year gained provides a very restricted picture of the relative cost effectiveness of the two procedures: a more meaningful picture requires reliable estimates of long term relative cost and benefit.
The economics of CABG and PCI have changed over the past 10–15 years with technical advances and secular trends. Continuing change in both procedures will lead to an ongoing need for high quality randomised studies measuring clinical and economic outcomes of the two forms of revascularisation, as well as inevitably more speculative modelling of possible longer term costs and effects.
Acknowledgments
The SoS economics writing committee thanks Helen Campbell, Health Economic Research Group, Brunel University for work on the EQ-5D analysis plan.
The SoS trial was supported by funding from a consortium of stent manufacturers: Bard (now Medtronic), Tolochennaz, Switzerland; Guidant, Santa Clara, USA; Schneider (now Boston Scientific), Ratingen, Germany.
Abbreviations
ARTS, arterial revascularisation therapies study
BARI, bypass angioplasty revascularisation investigation
CABG, coronary artery bypass grafting
COURAGE, clinical outcomes utilising revascularisation and aggressive drug evaluation
EAST, Emory angioplasty versus surgery trial
ERACI, Argentine randomised trial of percutaneous transluminal coronary angioplasty versus coronary artery bypass surgery in multivessel disease
PCI, percutaneous coronary intervention
PTCA, percutaneous transluminal coronary angioplasty
RITA-1, randomised intervention treatment of angina
SoS, stent or surgery
STENT OR SURGERY STEERING COMMITTEE
Rodney H Stables (Co-Principal Investigator), Ulrich Sigwart (Co-Principal Investigator), Jean Booth, Raimund Erbel, Peter Währborg, Jacobus Lubsen, Petros Nihoyannopoulos, John Pepper, Spencer B King III, William Weintraub, Peter Sleight.
The Clinical Trials and Evaluation Unit, The Royal Brompton Hospital, London, UK.
The Emory Center for Outcomes Research, Department of Medicine, Emory University, Atlanta, Georgia, USA.
Health Economics Research Group, Brunel University, Uxbridge, UK.
MEDTAP International Inc, London, UK.
REFERENCES
- 1.Anon. Coronary angioplasty versus coronary artery bypass surgery: the randomised intervention treatment of angina (RITA) trial. The RITA Investigators. Lancet 1993;341:573–80. [PubMed] [Google Scholar]
- 2.King SB III, Lembo NJ, Weintraub WS, for the EAST Investigators. A randomised trial comparing coronary angioplasty with coronary bypass surgery. N Engl J Med 1994;331:1044–50. [DOI] [PubMed] [Google Scholar]
- 3.Anon. Comparison of coronary bypass surgery with angioplasty in patients with multivessel disease. The BARI Investigators. N Engl J Med 1996;335:217–25. [DOI] [PubMed] [Google Scholar]
- 4.Anon. First-year results of CABRI (coronary angioplasty versus bypass revascularisation investigation). CABRI Trial Participants. Lancet 1995;346:1179–84. [PubMed] [Google Scholar]
- 5.Hamm CW, Reimers J, Ischinger T, et al. A randomised study of coronary angioplasty compared with bypass surgery in patients with symptomatic multivessel coronary artery disease. N Engl J Med 1994;331:1037–43. [DOI] [PubMed] [Google Scholar]
- 6.Rodriguez A , Boullon F, Perez-Balino N, et al. Argentine randomised trial of percutaneous transluminal coronary angioplasty versus coronary artery bypass surgery in multivessel disease (ERACI): in-hospital results and 1-year follow-up. J Am Coll Cardiol 1993;22:1060–7. [DOI] [PubMed] [Google Scholar]
- 7.Pocock SJ, Henderson RA, Rickards AF, et al. Meta-analysis of randomised trials comparing coronary angioplasty with bypass surgery. Lancet 1995;3435:1184–9. [DOI] [PubMed] [Google Scholar]
- 8.Serruys PW, Unger F, Sousa E, for the Arterial Revascularisation Therapies Study Group. Comparison of coronary-artery bypass surgery and stenting for the treatment of multivessel disease. N Engl J Med 2001;344:1117–24. [DOI] [PubMed] [Google Scholar]
- 9.Rodriguez A , Bernardi V, Navia J, et al. Argentine randomised study: coronary angioplasty with stenting versus coronary bypass surgery in patients with multiple-vessel disease (ERACI II): 30-day and one-year follow-up results. J Am Coll Cardiol 2001;37:51–8. [DOI] [PubMed] [Google Scholar]
- 10.Anon. Coronary artery bypass surgery versus percutaneous coronary intervention with stent implantation in patients with multivessel coronary artery disease (the stent or surgery trial): a randomised trial. The SoS Investigators. Lancet 2002;360:965–70. [DOI] [PubMed] [Google Scholar]
- 11.Weintraub WS, Mauldin PD, Becker E, et al. A comparison of the costs of and quality of life after coronary angioplasty or coronary surgery for multivessel coronary artery disease. Results from the Emory angioplasty versus surgery trial (EAST). Circulation 1995;92:2831–40. [DOI] [PubMed] [Google Scholar]
- 12.Hlatky MA, Rogers WJ, Johnstone I, et al. Medical care costs and quality of life after randomization to coronary angioplasty or coronary bypass surgery. N Engl J Med 1997;336:92–9. [DOI] [PubMed] [Google Scholar]
- 13.Sculpher MJ, Seed P, Henderson RA, et al. Health service costs of coronary angioplasty and coronary artery bypass surgery: the randomised intervention treatment of angina (RITA) trial. Lancet 1994;344:927–30. [DOI] [PubMed] [Google Scholar]
- 14.Henderson RA, Pocock SJ, Sharp SJ, et al. Long-term results of RITA-1 trial: clinical and cost comparisons of coronary angioplasty and coronary-artery bypass grafting. Lancet 1998;352:1419–25. [DOI] [PubMed] [Google Scholar]
- 15.Rodriguez A , Mele E, Peyregne E, et al. Three-year follow-up of the Argentine randomised trial of percutaneous transluminal coronary angioplasty versus coronary artery bypass surgery in multivessel disease (ERACI). J Am Coll Cardiol 1996;27:1178–84. [DOI] [PubMed] [Google Scholar]
- 16.Weintraub WS, Becker ER, Mauldin PD, et al. Costs of revascularisation over eight years in the randomised and eligible patients in the Emory angioplasty versus surgery trial (EAST). Am J Cardiol 2000;86:747–52. [DOI] [PubMed] [Google Scholar]
- 17.Anon. Chartered Institute of Public Finance and Accountancy. The health service financial database 1999. Croydon: Institute of Public Finance, 1999.
- 18.Netten A , Rees T, Harrison G. The unit costs of health and social care 2001. Canterbury: Personal Social Services Research Unit, University of Kent, 2001.
- 19.Henderson R , Brown RE. The costs of routine eptifibatide use in acute coronary syndromes in western Europe: an economic substudy of the PURSUIT trial. Eur Heart J Suppl 1999;1 (suppl N) :N35–41. [Google Scholar]
- 20.Berry E , Kelly S, Hutton J, et al. Intravascular ultrasound-guided interventions in coronary artery disease: a systematic literature review, with decision analytic modelling, of outcomes and cost-effectiveness. Health Technol Assess 2000;4:1–117. [PubMed] [Google Scholar]
- 21.McKenna M , Wheeldon N, Buxton MJ. Costing cardiac revascularisation for economic evaluation: micro-costing vs routine data. Br J Med Econ 1997;11:65–79. [Google Scholar]
- 22.Chambers M , Hutton J, Gladman J. Cost-effectiveness analysis of antiplatelet therapy in the prevention of recurrent stroke in the UK. Pharmacoeconomics 1999;16:577–93. [DOI] [PubMed] [Google Scholar]
- 23.Anon. NHS Executive. The new NHS reference costs. Leeds 2000.
- 24.Anon. British national formulary. London: British Medical Association and Royal Pharmaceutical Society, 2000.
- 25.Anon. NHS Executive The hospital and community health services index 2000. Leeds, 2000.
- 26.Rabin R , De Charro F. EQ-5D: a measure of health status from the EuroQoL group. Ann Med 2001;33:337–43. [DOI] [PubMed] [Google Scholar]
- 27.Dolan P , Gudex C, Kind P, et al. The time trade-off method: results from a general population survey. Health Econ 1996;5:141–54. [DOI] [PubMed] [Google Scholar]
- 28.Efron B , Tibshirani RJ. An introduction to the bootstrap. New York: Chapman and Hall, 1993.
- 29.Rubin DB. Multiple imputation after 18+ years. J Am Stat Assoc 1996;91:473–89. [Google Scholar]
- 30.Fischman DL, Leon MB, Baim DS, et al. for the Stent Restenosis Study Investigators. A randomised comparison of coronary-stent placement and balloon angioplasty in the treatment of coronary artery disease. N Engl J Med 1994;331:496–501. [DOI] [PubMed] [Google Scholar]
- 31.Serruys PW, de Jaegere P, Kiemeneij F, et al. for the Benestent Study Group. A comparison of balloon-expandable-stent implantation with balloon angioplasty in patients with coronary artery disease. N Engl J Med 1994;331:489–95. [DOI] [PubMed] [Google Scholar]
- 32.Rosengart TK. New approaches to the surgical therapy of atherosclerotic coronary artery disease. Am J Cardiol 1999;83:40B–5B. [Google Scholar]
- 33.Weintraub WS, Craver JM, Jones EL, et al. Improving cost and outcome of coronary surgery. Circulation 1998;98:23–8. [PubMed] [Google Scholar]
- 34.Weintraub WS, Ghazzal ZMB, Douglas JS Jr, et al. Trends in outcome and costs of coronary intervention in the 1990’s. Circulation 1997;96:I456. [DOI] [PubMed] [Google Scholar]
- 35.Sousa JE, Costa MA, Abizaid A, et al. Lack of neointimal proliferation after implantation of sirolimus-coated stents in human coronary arteries: a quantitative coronary angiography and three-dimensional intravascular ultrasound study. Circulation 2001;103:192–15. [DOI] [PubMed] [Google Scholar]
- 36.Morice MC, Serruys PW, Sousa JE, et al. for the RAVEL Study Group. A randomised comparison of a sirolimus-eluting stent with a standard stent for coronary revascularisation. N Engl J Med 2002;346:1773–180. [DOI] [PubMed] [Google Scholar]
- 37.Blumenthal RS, Cohn G, Schulman SP. Medical therapy versus coronary angioplasty in stable coronary artery disease: a critical review of the literature. J Am Coll Cardiol 2000;36:668–73. [DOI] [PubMed] [Google Scholar]
- 38.King SP III, Barnhard HX, Kosinski AS and the EAST Investigators. Angioplasty or surgery for multivessel coronary artery disease: comparison of eligible registry and randomised patients in the EAST trial and influence of treatment selection on outcomes. Am J Cardiol 1997;79:1453–9. [DOI] [PubMed] [Google Scholar]