Despite public apprehension over the risks of developing cancer, in most countries the public has more to fear from cardiovascular disease (CVD). Coronary heart disease (CHD) and stroke, the principal manifestations of CVD, are the first and second most common causes of death worldwide.1 The World Health Organization predicts that, by 2020, coronary heart disease will become the world’s most important cause of death and disability and, further, the most important cause of premature death. Overall CVD therefore leads to substantial patient morbidity and, through the management of stroke and heart failure, results in the highest healthcare utilisation costs for any disease in many countries. Strategies to prevent CVD therefore have global significance and should be as high a priority for healthcare systems (if for no other reason than to reduce expenditure) as for individuals. Both primary and secondary prevention strategies are essential, the former at least partly justified by one in five coronary events presenting with sudden death as the first and only symptom.
RISK FACTORS FOR CVD
CVD represents a cluster of disorders, associated with complex interactions between multiple risk factors. The risk factors, or co-morbidities, that lead to enhanced risk of developing CVD have been recognised for many years.2 The main CVD risk factors include smoking,3 hypertension,4 and dyslipidaemia.5 Further major influences relate to familial risk (premature CVD in men before 55 years old and women before 65 years old) and diabetes, which results in a gross acceleration of the pathological processes involved in CVD. Other important predisposing factors include diet, physical inactivity, obesity, and genetic influences. Although more than 200 risk factors for CHD have now been identified, the single most powerful predictor of CHD risk is abnormal lipid values. All of these risk factors are multiplicative, acting to exaggerate the damage caused by each risk factor alone.
Role of hypertension in CVD
One of the most important individual risk factors for CVD is hypertension. Current hypertension guidelines incorporate much unequivocal clinical evidence on how to treat and to what appropriate targets.6,7 One major issue for the recent guidelines is to avoid reinforcing the traditional viewpoint that hypertension is a disease in isolation, but should be viewed alongside measures to achieve overall reduction of cardiovascular risk. Global estimation of 10 year CHD or CVD risk is therefore needed in all hypertensives to determine eligibility for CHD primary prevention strategies,8 in addition to treating the hypertension. Importantly, guidelines now emphasise the necessity for differentiating thresholds for initiating treatment in hypertension, as well as setting the targets for such treatment.
Role of dyslipidaemia in CVD
A strong positive and graded relation with CHD death occurs for total cholesterol (TC) concentrations above 4.6 mmol/l (180 mg/dl).9 The individual lipid fractions, low density lipoprotein cholesterol (LDL-C), high density lipoprotein cholesterol (HDL-C), and triglycerides, are independent risk factors, with LDL-C the most significant predictor of individual CHD risk. Primary and secondary prevention trials have shown that therapeutic intervention to lower LDL-C to target values significantly reduce CHD morbidity and mortality by 22–30%, with no increase in death by non-CHD.10,11 Furthermore, the heart protection study (HPS)12 has confirmed early data from carotid atherosclerosis regression and lipid trials that high LDL-C is also a modifiable risk factor for cerebrovascular atherosclerosis and stroke.
In contrast to the adverse influence of other lipid fractions, there is a powerful protective inverse relation between HDL-C and incidence of CHD. Individuals with low HDL-C concentrations (⩽ 1.04 mmol/l (⩽ 40 mg/dl)) and average TC values (⩽ 5.2 mmol/l (⩽ 200 mg/dl)) have the same CHD risk as individuals with high TC concentrations (⩾ 6.7 mmol/l (⩾ 260 mg/dl)). There is a 2–3% reduction in CHD risk for every 0.02 mmol/l (1 mg/dl) incremental increase in HDL-C.
Simultaneous elevation of serum HDL-C concentrations and reduction of non-HDL-C concentrations resulted in 34% reduction in the incidence of CHD. Patients whose primary lipid abnormality is low HDL-C show a reduction in major coronary events when HDL-C concentrations are raised and triglyceride concentrations lowered, even when LDL-C values are not reduced.13 However, although established as an independent CHD risk factor in observational studies, the cardioprotective effect of raising HDL-C concentrations in the generality of patients at risk requires further elucidation in trials. Therefore, HDL-C remains secondary to LDL-C as a target for predicting and preventing CHD risk.
Plasma triglyceride concentration is an independent risk factor for CHD in both men and women. A meta-analysis of 17 prospective population based studies determined that for men, the overall relative risk is 1.32, which correlates with a 30% increase in risk for a 1 mmol/l increase in triglyceride concentration. The combination of high triglyceride (⩾ 1.7 mmol/l (⩾ 150 mg/dl)) and low HDL-C (⩽ 1.04 mmol/l (⩽ 40 mg/dl)) identifies groups at particular CHD risk. In women, assessing both triglyceride and HDL-C values may be the most predictive indicator of CHD risk, with a relative risk of 1.76. The Copenhagen male study concluded that high triglyceride and low HDL-C is at least as predictive of ischaemic heart disease as isolated high LDL-C and recommends interventions to optimise this ratio. Although these data suggest causal association, reducing triglyceride concentrations has not yet been shown to decrease risk of CVD.
CURRENT PRACTICE IN PREVENTION OF CVD
The sheer scale of CVD in most countries, linked to repeated surveys demonstrating under management of CHD patients across specialist centres in Europe,14 has resulted in the identification of CVD as one of the main priorities for improved care across healthcare systems. For example, UK government targets are to reduce cardiovascular mortality by 40% by 2010 from the rates in 1995, via the National Service Framework for coronary heart disease (NSF CHD) in England and SIGN CHD guidelines in Scotland. The main aim for all countries is to identify the various at-risk populations more accurately, and to initiate and sustain treatment more consistently in those identified at risk. For CVD there is an enormous evidence base to guide the most appropriate interventional strategies to reduce risk in patients with established disease (secondary prevention) and attenuate risk in those patients at highest risk who have not yet established the disease (primary prevention).
However, the scale of under management in CVD prevention remains enormous in most countries. For example, despite recent improvements, only 16% of 24 431 CHD patients were on a statin in general practice in 1998, rising to 29% of 646 men with CHD in the British regional heart study in 2000, and 53% of 11 996 CHD patients in general practice by the end of 2002. Indeed, a huge 2003 audit of 78 600 patients with CHD in UK general practice showed only 48% had a valid cholesterol measurement, 55% were taking statin, and of these only 53% were at their cholesterol target. Furthermore, only 6% of the current hypertension population in England achieve target blood pressures below 140/90 mm Hg.
This serious under treatment of CVD risk is not confined to the UK. A study of 4888 patients of 619 primary care physicians in the USA found that only 37% of hypercholesterolaemic patients reached the LDL-C goals set by the US clinical guidelines, and only 5.2% of CHD patients met the total cholesterol goal of under 5.2 mmol/l (200 mg/dl). Management of secondary CHD prevention is no better in Europe, even in specialist settings. Further, there were only limited improvements in care in Europe between 1996/97 and 1999/2000.14
Factors leading to physician underperformance in CVD prevention include gaps in knowledge and confusion over recommendations, such as whether to select patients for primary or secondary prevention, how to use risk equations, whether for hypertension or CVD risk, and what the target levels are for lipid fractions during treatment. Indeed, 18% of primary care physicians in a large survey across five European countries volunteered that a major barrier to their improved delivery of CHD prevention guidelines was that they were confused and needed more education on clinical recommendations for lipid management. Although we may think that all these messages are well understood by doctors, the evidence from physician surveys highlights the continued relevance of clinical reviews in this area.
So, since the aetiologies for CVD are well elucidated, the interactions of risk factors identified, and effective evidence based interventions well known, whether for primary or secondary prevention, are different strategies needed? There is much in common, especially over what interventions to employ in at-risk individuals, but we probably underestimate just how confusing or difficult it is for clinicians to deliver what are essentially different prevention strategies. The principal difference lies in how patients are identified and deemed to be at-risk and therefore eligible for primary or secondary prevention. Practitioners need discrete systems to deal with incident cardiovascular risk cases, whether through case finding for primary prevention or post-event monitoring in secondary prevention, but might operate combined strategies for prevalent cases once identified. This paper therefore considers the rationale for differing case identification strategies initially, before summarising the evidence base for the common interventions.
IDENTIFYING PEOPLE ELIGIBLE FOR SECONDARY PREVENTION OF CVD
All CVD prevention guidelines highlight that the people with most to gain from treatment are those at greatest risk of CHD. These are also the groups in whom treatment is most cost effective. The individuals at most risk are those who have current symptoms of heart disease (such as have suffered a heart attack, suffer angina, or have received coronary revascularisation) or those with symptoms of other arterial disease (such as stroke, transient ischaemic attack, or peripheral vascular disease). All of these patients are automatically eligible for secondary prevention measures (secondary for they already have established CVD and the aim is to prevent progression) to reduce their risk of repeat events or death. In addition to automatically meeting the threshold for treatment of risk factors, secondary prevention guidelines also provide the specific targets for treatment, whether for blood pressure control or for TC or LDL-C. Multiple antihypertensives and statin monotherapy will be necessary in the majority of secondary prevention patients to achieve these targets. The main interventions advocated for CVD secondary prevention are listed in the box above; as stated, most also apply to primary prevention. All interventions recommended are relevant to the prevention of overall CVD.
Interventions for people with clinical evidence of vascular disease.
Advice on how to stop smoking, including use of nicotine replacement therapy (PP&SP)
Information on modifiable risk factors and personal advice on how they can be reduced (including physical activity, diet, alcohol consumption, weight, and diabetes) (PP&SP)
Advice and treatment to maintain blood pressure below 140/85 mm Hg (140/80 or even 130/80 mm Hg in patients with diabetes) (PP&SP)
Low dose aspirin (75 mg daily) for all those tolerant (SP)
Statins and dietary advice to lower serum cholesterol concentration either to < 5 mmol/l (or < 25% of pre-treatment values, whichever is greater in the NSF) or LDL-C to < 3 mmol/l (or < 30% pre-treatment, whichever is greater) (PP&SP)
β Blockers for people who also have had a myocardial infarction (SP)
Angiotensin converting enzyme (ACE) inhibitors for people post-myocardial infarction who also had left ventricular dysfunction (SP)
Warfarin or aspirin for people over 60 years who also have atrial fibrillation (PP&SP)
Meticulous control of blood pressure and glucose in people who also have diabetes (PP&SP)
β Blockers for people who also have had a myocardial infarction (SP)
PP, primary prevention; SP, secondary prevention.
The failure to implement secondary prevention strategies adequately is initially perplexing—after all, these patients have identified themselves to clinicians by suffering a major cardiovascular event, such as stroke or myocardial infarction, or presenting with significant symptoms, such as angina. Screening for those at risk is therefore not necessary. However, in addition to rapid assessment and treatment of patients presenting with established CVD (to confirm the diagnosis and limit the immediate risks to patients), formalising their subsequent follow up is necessary to maximise secondary prevention. Essential strategies for hospitals therefore include formal, protocol driven discharge or outpatient clinic policies that ensure patients have received the appropriate advice and secondary prevention interventions before discharge from the ward or clinic. It is also essential that follow up arrangements, be they for cardiac or stroke rehabilitation, smoking cessation, or treatment monitoring, are transmitted to the family doctor as well as the patient. Such procedures are more likely to be adhered to if structured discharge or outpatient letters including check lists are used, and the process is completed by trained staff whose performance is audited with feedback.
The essential first step for secondary CVD prevention in primary care is the accurate identification of those patients at greatest risk, by establishing disease registers for CHD and stroke. Having established registers, practices need to initiate, conduct, and repeat clinical audit to ensure that the stipulated interventions are actually offered to those on the CVD registers. Furthermore, internal mechanisms are needed that routinely update the registers as incident cases present. These recommendations are essentially pragmatic, for few data exist on trials to test whether such policies actually work. Limited data suggest that recall of secondary prevention patients to either a general practitioner or a nurse CHD clinic is more effective at improving adequate recording of risk factors at 18 months compared to audit and feedback (76%, 85%, and 53%, respectively). However, none of these interventions influenced clinical outcomes (blood pressure or cholesterol values, smoking status, or prescriptions for antihypertensives or statins).
IDENTIFYING PEOPLE ELIGIBLE FOR PRIMARY PREVENTION OF CVD
Interventions for those individuals at high risk without established CVD are similar to those proposed in secondary prevention (see box). The biggest difference with secondary prevention, with huge implications for clinical practice, is how to determine those at most risk who should be offered interventions. European guidelines emphasise the importance of incorporating regular CHD risk factor assessment into clinical practice. Since the whole adult population is potentially at risk, responsibility for formalising primary prevention of CVD rests on primary care.
All adults are potentially eligible for cardiovascular screening; in practice, however, it is reasonable to focus on adults from the age of 40 years onwards, and on the basis of formally risk scoring anyone with a single CHD risk factor such as hypertension or current smoker. However, anyone with premature CVD (established CVD before 55 years in men and 65 years in women) in a first degree relative should be screened for elevated cholesterol as early as is practical, to exclude familial hypercholesterolaemia. Whether individuals are screened repeatedly will vary by country: the American Heart Association recommends at least two-yearly risk factor updating and five-yearly global risk estimation.
Initial information needed
Initial risk assessment should question lifestyle (smoking status, physical activity level, alcohol use/abuse, oral contraception use) and family history (relatives with premature CHD, hypertension, or diabetes). Body mass index, waist circumference, and blood pressure should be measured. Lipid concentrations should also be assessed in any individual with any CHD risk factor, such as raised blood pressure, obesity, family history, or diabetes. Most laboratories measure TC and HDL-C, and then calculate LDL-C by using the Friedewald formula: LDL-C = TC − HDL-C − (0.45 × triglycerides). Other markers, such as HDL-C (⩽ 1.0 mmol/l (⩽ 40 mg/dl)) and fasting triglycerides (⩾ 2.0 mmol/l (⩾ 180 mg/dl)) can be used for identifying individuals at increased coronary risk, but suffer the need to collect a fasting sample.
In patients aged 40–69 years, metabolic risk factors (that is, hypertension, diabetes, dyslipidaemia) become more prevalent. For middle aged women, premature menopause is an additional risk factor for CHD. Unfortunately, the presumption from observational studies that hormone replacement therapy (HRT) helped reverse this post-menopausal rise in CHD has not been borne out in formal HRT intervention trials, where the rate of CHD events actually increased (due to an excess of events in the first year of HRT). The largest proportion of high risk individuals will be found in the older population (⩾ 70 years). Hypertension, smoking, and hyperlipidaemia are the three most important modifiable risk factors in this population.
Multifactorial global risk estimation
Although high LDL-C may be the most important individual risk factor for CHD, estimation of an individual’s actual risk for future CHD events must take into account all other coexistent CHD risk factors. Indeed, risk associated with any level of cholesterol is notably influenced by coexistent risk factors. LDL-C acts as an accelerator of risk; as baseline LDL-C increases, the CHD risk impact of other risk factors increases at a faster rate. Therefore, an individual with a number of modest risk factors may be at considerably greater risk for CHD than a person with one very high risk factor.
These risk factor interactions provide the rationale for determining patient eligibility for primary prevention treatments on the basis of formal CHD risk scoring. European guidelines for CHD risk assessment use sex, age, smoking status, systolic blood pressure, presence of left ventricular hypertrophy, and TC to assess 10 year risk for CHD or CVD.15 The combined British societies guidelines are broadly similar to the European guidelines, but use HDL-C:TC ratio to calculate CHD risk score, rather than TC.
The method of determining individual global risk is using one of the various algorithms available, based upon the Framingham equation.16 These tools include the third edition of the Sheffield risk tables, the European coronary risk chart, or the New Zealand risk assessments tool. In addition to these colour charts (which classify risk by sex, age, systolic blood pressure, TC and HDL-C, and smoking status), a number of computer based programmes are available. However, even these relatively simple tools require training of staff in their use since the limited studies that have validated their use by primary care staff show errors are common and systematic. Furthermore, there is limited evidence that physicians are confused by the variation in recommendations between different guidelines.
In the UK, the initial priority for primary prevention of CVD is to treat patients whose risk of CHD events is greater than 30% over 10 years using the Framingham risk equation; this is based on grounds of affordability since even patients at as low a risk of CHD as 6% over 10 years will still benefit from statin treatment. For most countries, and the ultimate target for the UK, the threshold for treatment is a 20% 10 year risk. An exception to this conservative 30% 10 year threshold for intervention in the UK is the diabetic patient group, where a lower 15% CHD or 20% CVD threshold is advocated to trigger primary prevention. In the US guidelines, patients with diabetes are treated as coronary risk equivalent and therefore do not need their risk estimated, but simply treated to LDL target. Another group where adjustment of the global risk score is required comprises those with a positive family history of premature CVD (below 55 years in men or 65 in women), where a multiplier of 1.5 of the risk score is advocated in the UK (effectively producing a threshold of 20% 10 year risk). A similar weighting is advocated by some for ethnic minorities because of their accelerated cardiovascular risk.
A major problem with global risk estimation is what should be done for individuals at borderline risk, currently identified as a 10 year risk of 10–20% in the USA or 20–30% in the UK. The pragmatic suggestion in the UK is to recalculate the 10 year risk, having projected the patient’s age to 60 (since age is a major driver in the model) in those borderline cases where the clinician feels uncomfortable in not providing primary prevention on the basis of the global risk score. A more scientific approach would be to use the triad of high LDL-C, low HDL-C (< 1 mmol/l), and elevated triglycerides (> 1.8 mmol/l) as a trigger to intervene in “moderate” risk individuals. Individuals with this triad, which is significantly associated with the metabolic syndrome, suffered a greater cardiovascular event rate than those with isolated elevation of LDL-C in the placebo arm of the 4S trial (29.7% v 25.6% at one year, p = 0.01), and achieved a much higher event reduction on statin treatment (relative risk reduction (RR) 0.48 v 0.86 and between treatment RR of 0.48, 95% confidence interval (CI) 0.33 to 0.69). Similarly, additional adverse cardiovascular risk with the triad compared to isolated elevated LDL-C (RR 3.8) and enhanced treatment benefit (71% v 34%) has been observed with gemfibrozil and explained all the treatment effect in the BIP (benzafibrate in CVD prevention) study.
The public health implications of reducing thresholds for eligibility for primary prevention are enormous. Using a 30% 10 year cut-off is estimated to encompass 3.4% of the UK population, in addition to the 4.8% eligible for secondary prevention. Reducing the threshold to 15% 10 year CHD risk (National Institute for Clinical Excellence recommendation for diabetes) would target 19.6% of the UK population for primary prevention alone, and reducing to 6% 10 year risk—the level observed in the placebo arm of AFCAPS/TexCAPS—would encompass around 57% of the UK population. Clearly these patient numbers are beyond the scope of current service provision and illustrate the crucial importance of greater public policy changes on food production and smoking to reduce overall population risk factors rather than medicalising most of the UK population.
Surrogate inflammatory markers to improve global risk assessment
One possible additional tool in the future will be the use of surrogate inflammatory markers for determining enhanced risk, most notably the inflammatory marker highly sensitive C reactive protein (hsCRP), but also fibrinogen and white blood cells. Indeed the use of hsCRP is now advocated for guiding primary prevention treatment decisions in the moderate global risk category in the USA,17 differentiating between individuals with an hsCRP of < 1 mg/l (low risk), to 1–3 mg/l (average risk), to > 3 mg/l (high risk). These recommendations are based upon numerous observational studies that have demonstrated an approximately twofold elevated cardiovascular risk in the upper tertile of hsCRP concentrations compared to the lower tertile in several large longitudinal studies, with the association observable in men, women, and the elderly. No other country has yet advocated surrogate marker use because these observational data have not been replicated in formal trials.
In summary, the challenge for clinicians is to develop robust systems that enable repeated opportunistic screening of their adult populations for smoking, obesity, hypertension, and diabetes, with subsequent assessment of lipid status in those positive and with formal CVD risk score assessment. These steps should result in treating the overall CVD risk as well as the individual abnormalities. To supplement this opportunistic screening, practices need to perform annual audit searches to identify patients eligible for lipid and CVD risk assessment that have been missed. The use of surrogate risk markers, such as hsCRP, await formal trial evidence before adoption into routine clinical practice.
INTERVENTIONS TO REDUCE CARDIOVASCULAR RISK IN PRIMARY AND SECONDARY PREVENTION
The overall objective of CVD prevention is to reduce the risk of a major CVD event. To meet this objective, both lifestyle and therapeutic goals are set (table 1). Patients should be counselled to stop smoking, make healthy food choices, be physically active, and achieve their ideal weight. Other risk factors, such as blood pressure, blood glucose, TC, and LDL-C should be normalised.
Table 1.
Risk factors for CVD and recommended European target goals: key points
| Non-modifiable | |
| • Age | Men: ⩾45 years |
| Women: >55 years | |
| • Personal history of CHD | |
| • Family history of CHD | |
| Modifiable | Target goals |
| • High TC | <5.0 mmol/l (<190 mg/dl) |
| • High LDL-C | <3.0 mmol/l (<115 mg/dl) |
| • Low HDL-C | >1.1 mmol/l (>40 mg/dl) |
| • High triglyceride | <1.2 mmol/l (<150 mg/dl) |
| • Hypertension | <140/85 mm Hg (140/80 or 130/80 mm Hg in diabetes) |
| • Diabetes mellitus | Normalise glucose concentrations (HBA1C below 7 mmol/l) |
| • Current tobacco use | Smoking cessation |
| • Obesity | Body mass index <25 kg/m2 |
| • Sedentary lifestyle | Exercise for 30 minutes 3–5 times weekly |
HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; TC, total cholesterol.
Role of lifestyle intervention to prevent CVD
Most risk associated with lifestyle relates to smoking, now the single greatest cause of illness and premature death in the UK. Numerous interventions to assist smoking cessation have been evaluated and physician guidelines published.18 Brief opportunistic advice to stop smoking does have a significant influence on smoking cessation, with a 2% (95% CI 1% to 3%) effect size compared to placebo at six months when conducted in primary care. Intensive behavioural support from a specialist can achieve 4% (95% CI 0% to 8%) to 7% (95% CI 5% to 9%) effect size, dependent on setting. Nicotine replacement therapy, in whatever formulation, has a significant incremental effect on counselling, with a range of effect sizes from 5% (95% CI 4% to 7%) with brief counselling to 12% (95% CI 7% to 17%) effect size with intensive behavioural support. Use of bupropion 300 mg per day achieves a similar effect size to nicotine replacement therapy (NRT) of 9% (95% CI 5% to 14%). Overall effect size of combining NRT or bupropion with intensive support is estimated at 13–19%. Less data are available on long term cessation rates; however, there is a blunting of the cessation rates with time, reducing by around a third at 3–4 years, and a 50% reduction in continued stop rate at eight years.
Normalisation of weight, increased consumption of fruit and vegetables, decreased intake of saturated fats (< 10% of calories), salt (< 6 g/day), and free sugars, and increased activity levels will all impact on reduced cardiovascular risk. Furthermore, such diets further provide primary prevention of new onset diabetes mellitus.19
Role of interventions for hypertension to prevent CVD
Patients with blood pressures between 160–199 mm Hg systolic over 100–109 mm Hg diastolic should all be treated, assuming levels do not drop after 4–12 weeks of non-pharmacological advice (or immediately in the case of established CVD and/or organ damage). For “borderline” blood pressures of 140–159 mm Hg systolic or 90–99 mm Hg diastolic, treatment should be instigated immediately in the case of existing end organ damage or established CVD. Furthermore, in all such patients, absolute cardiovascular risk should be assessed to guide treatment of hypertension, in much the same way as clinicians will be using such risk calculations to guide the need for statin treatment. In the case of hypertension, the trigger for treatment in “borderline hypertension” is suggested at a 10 year CHD risk above 15% (or CVD risk greater than 20%).
Appropriate choice of antihypertensive treatment has been subject to massive comparator trials where patients are randomised to incremental drug doses and sequences of drug classes. The evidence essentially confirms that the different drug classes in hypertension have a similar sized effect, in most patients, in reducing CVD. This has resulted in recommendations that most patients should start with a diuretic since they are so cheap and significantly reduce CVD risk at least as effectively as other drug classes. There are differences in clinical outcomes in some comparator studies that appear to show that some drugs are more effective than others, such as doxazosin versus others, ACE inhibitors versus diuretics, or angiotensin receptor blockers versus β blockers. However, these data may suffer the limitations of open studies, or less reliable categorisation of outcomes, or are generalisable only to high risk hypertension. Most of these studies were comparisons on a background of diuretic treatment in most patients.
The important unifying message from all hypertension trials is that most patients need multiple treatments to control blood pressure, from around 40% on two or more drugs in ALLHAT (antihypertensive and lipid lowering treatment to prevent heart attack trial) to 63% in HOT (hypertension optional treatment) to achieve diastolic pressure below 90 mm Hg (73% to below 80 mm Hg in HOT). Furthermore, these trials have demonstrated that it is feasible to reach blood pressure targets over extended periods (at least in trials) with control of hypertension (defined as a systolic blood pressure < 140 mm Hg and diastolic blood pressure < 90 mm Hg) achieved in approximately two thirds of participants at five years in ALLHAT and 85% at four years in HOT. These rates of hypertension control greatly exceed corresponding rates in the general population (approximately 44% in the USA and 6% in England). Physicians may therefore appropriately tailor initial medication to the patient on the basis of factors such as age, co-morbidity, adverse events, or ethnicity, but will in most cases need to end up with two or three different classes of drug to achieve adequate control.
Role of interventions for dyslipidaemia to prevent CVD
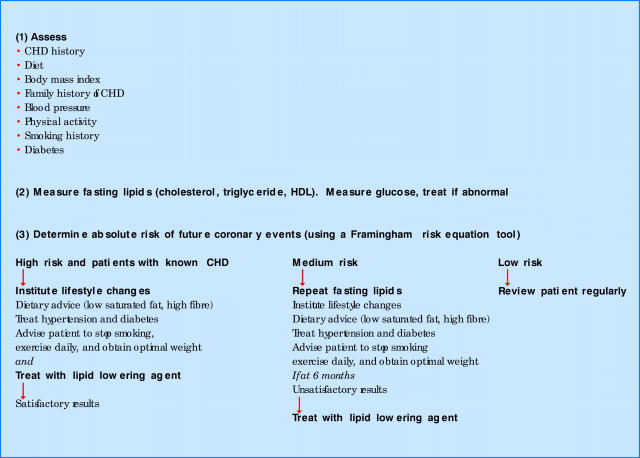
Lowering LDL-C is the primary focus for the management of dyslipidaemia, by lifestyle interventions and, usually, pharmacotherapy to achieve recommended goals (fig 1). In low risk and moderate risk individuals, the European and British guidelines advocate an initial management strategy of dietary adjustment (reduced intake of total fats, reduced intake of saturated fats, increased intake of fresh fruits and vegetables (five portions daily), reduced salt intake (< 1 g/day), and reduced alcohol use), increased physical activity, and weight reduction, if needed. For a few, lifestyle counselling is the only intervention required. Moderate risk patients who do not achieve target LDL-C concentrations with lifestyle modification and patients in the high risk category should be offered drug intervention. Patients with established CVD (secondary prevention patients) should always be offered lipid lowering treatment.
Figure 1.
Risk assessment based management of cardiovascular disease: key points. CHD, coronary heart disease; HDL, high density lipoprotein.
Current UK and European recommendations suggest a target LDL-C concentration of ⩽ 3 mmol/l (⩽ 115 mg/dl), regardless of degree of individual risk. However, a threshold value below which LDL-C lowering no longer provides additional reduction in CHD risk has not been identified and debate surrounds the question of what the minimal LDL-C target should be. Indeed, there is evidence for lowering lipid concentrations to below the currently recommended minimum targets. Current trials are formally testing the benefit of additional lipid lowering in high risk CHD patients, such as target LDL-C below 1.9 mmol/l (73 mg/dl) in the higher dose statin arm of the TNT (treat to new targets) study.
Five classes of lipid lowering agents are available: bile acid sequestrants, niacin, fibrates, cholesterol absorbers, and 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors (statins). Guidelines state that preference should be given to statin monotherapy because of the stronger evidence supporting their efficacy in reducing coronary morbidity, mortality, and prolonging survival in CHD patients and those at risk for CHD. All of the licensed statins are well tolerated and have good long term safety records. There are differences between statins in their effectiveness at LDL-C lowering at comparable doses and their duration of action. Shorter acting statins should be dosed at night. If the target LDL-C goal is not reached within a reasonable time period, the statin dose should be titrated up.
Additional interventions for secondary prevention of CVD
All of the interventions discussed above are the same for either primary prevention, once the individual is identified as being at sufficient risk, or secondary prevention. Additional interventions for secondary prevention include low dose aspirin (75–160 mg daily) in all cases20 and β blockers post-myocardial infarction, plus ACE inhibitors where systolic dysfunction had occurred. More recent data are likely to extend the use of ACE inhibitors to all patients with CHD, whether high risk or low risk. Finally, most patients with atrial fibrillation (all those over 65 years) should receive thromboprophylaxis by anticoagulation with warfarin to a target international normalised ratio (INR) of 2.
SUMMARY
European and US guidelines emphasise the importance of identifying and treating all adults with CVD or at high risk for developing CVD. Although tools are available that can aid in the identification and treatment of individuals at risk, substantial opportunities to reduce morbidity and mortality are being missed. If the rising toll of CVD is to be reduced, preventive cardiology for individuals at risk for CHD must become a medical priority. Identification of at-risk individuals and institution of aggressive risk factor modification must become standard practice, in compliance with international treatment guidelines. The complexity of the population screening, the surveillance of those at risk, the requirement to intervene to specific targets, and the need to audit to satisfactory standards will be a considerable challenge to all health providers.
REFERENCES
- 1.Murray CJ, Lopez AD. The global burden of disease, 1990–2020. Nat Med 1998;4:1241–3. [DOI] [PubMed] [Google Scholar]
- 2.Neaton JD, Wentworth D. Serum cholesterol, blood pressure, cigarette smoking, and death from coronary heart disease. Arch Intern Med 1992;152:56–64. [PubMed] [Google Scholar]
- 3.Doll R , Peto R, Wheatley K, et al. Mortality in relation to smoking: 40 years’ observations on male British doctors. BMJ 1994;309:901–11. ▸ Highly influential data from the Oxford trials group that comprehensively de-bunked propaganda from the tobacco industry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.MacMahon S , Peto R, Cutler J, et al. Blood pressure, stroke, and coronary heart disease. Part 1, prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet 1990;335:765–74. ▸ The first major meta-analysis of the placebo controlled hypertension treatment trials involving patients in 14 studies which showed that treatment significantly reduced CHD as well as stroke. Helped to establish CVD as one of the most evidence based areas of clinical medicine. [DOI] [PubMed] [Google Scholar]
- 5.Pocock SJ, Shaper AG, Phillips AN. Concentrations of high-density lipoprotein cholesterol, triglycerides, and total cholesterol in ischaemic heart disease. BMJ 1989;298:998–1002. ▸ Study of 7735 men in the British regional heart study (from general practices across 24 regional towns), individuals who helped confirm the association between elevated lipids and cardiovascular risk, especially for total cholesterol values. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hansson L , Zanchetti A, Carruthers SG, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the hypertension optimal treatment (HOT) randomised trial. HOT study group. Lancet 1998;351:1755–62. ▸ Very influential trial of 18790 patients in primary care treated to three different blood pressure targets (150/90, 145/85, and 140/80 mm Hg) and followed for four years that showed that: (1) below 150/90 mm Hg was significantly better than above (but lack of power failed to distinguish, except in diabetic patients, between the three levels because only 3 mm Hg blood pressure difference emerged rather than the 10 mm Hg planned); (2) that multiple drugs were needed to achieve control in over two thirds; and (3) that reaching targets could be maintained for years in primary care. [DOI] [PubMed] [Google Scholar]
- 7.United Kingdom Prospective Diabetes Study Group. Tight blood pressure control and risk macro-vascular and micro-vascular complications in type 2 diabetes. UKPDS. BMJ 1998;317:703–13. ▸ Major trial of 3867 patients for up to 20 years (mean length of treatment was 11 years) that made up for the length it took to complete by the number of subsequent publications, and demonstrated the critical importance of treating vascular risk factors as well as glucose values and confirmed that degree of blood pressure control determined outcomes.9732337 [Google Scholar]
- 8.Second Joint Task Force. Prevention of coronary heart disease in clinical practice. Recommendations of the second joint task force of European and other societies on coronary prevention. Eur Heart J 1998;19:1434–503. [DOI] [PubMed] [Google Scholar]
- 9.Neaton JD, Blackburn H, Jacobs D, et al. Serum cholesterol level and mortality findings for men screened in the multiple risk factor intervention trial. Multiple risk factor intervention trial research group. Arch Intern Med 1992;152:1490–5000. ▸ Classic paper from the multiple risk factor intervention trial (MRFIT) group which, with the Framingham study, identified unequivocally the importance of interaction and multiplication of risk factors in driving vascular disease, among the 350 977 participants aged 35–57 years followed up for an average of 12 years, and the importance of not treating risk factors in isolation. [PubMed] [Google Scholar]
- 10.Scandinavian Simvastatin Survival Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian simvastatin survival study (4S). Lancet 1994;344:1383–9. ▸ Landmark Swedish trial of high risk secondary prevention in 4444 patients that led the massive evidence base on the efficacy and safety of the HMG-CoA reductase inhibitors (statins) that initiated the growth of the class to the world’s most prescribed drugs. 4S showed a 30% risk reduction in all cause mortality over 5.4 years, and the mortality curves continue to diverge at subsequent follow ups of the cohort.7968073 [Google Scholar]
- 11.Shepherd J , Cobbe SM, Ford I, et al. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland coronary prevention study group. N Engl J Med 1995;333:1301–7. ▸ Equally important as 4S is this Scottish statin trial of high risk CVD primary prevention in 6595 men aged 45–64 years that demonstrated a 24% risk reduction in mortality in men with no prior CVD. [DOI] [PubMed] [Google Scholar]
- 12.Heart Protection Study Collaborative Group. MRC/BHF heart protection study of cholesterol lowering in 20536 high risk individuals: a randomised controlled clinical trial. Lancet 2002;360:7–22. ▸ More recent large UK statin trial of 20 536 individuals with only modest elevation of total cholesterol (above 3.5 mmol/l), that achieved a 17% reduction in all cause mortality compared to the placebo group, plus answered many remaining questions—statins were equally effective and safe in the elderly, they reduced stroke rates by 25%, there was no excess cancer rates, and they were equally effective in patients with diabetes and no CVD as in people with established CVD.12114036 [Google Scholar]
- 13.Rubins HD, Robins SJ, Collins D, et al. Gemfibrozil for the secondary prevention of coronary heart disease in men with low levels of high-density lipoprotein cholesterol. Veterans Affairs high-density lipoprotein cholesterol intervention trial (VA-HIT) study group. N Engl J Med 1999;341:410–8. [DOI] [PubMed] [Google Scholar]
- 14.EUROASPIRE I and II Group. Clinical reality of coronary prevention guidelines: a comparison of EUROASPIRE I and II in nine countries. Lancet 2001;357:995–1001. [DOI] [PubMed] [Google Scholar]
- 15.Wood D , De Backer G, Faergeman O, et al. Prevention of coronary heart disease in clinical practice: recommendations of the second joint task force of European and other societies on coronary prevention. Atherosclerosis 1998;140:199–270. [DOI] [PubMed] [Google Scholar]
- 16.Anderson KM, Odell PM, Wilson PWF, et al. Cardiovascular disease risk profiles. Am Heart J 1991;121:293–8. ▸ Original data from one of the most important epidemiological cohorts in the history of medicine that has spawned most risk factor estimators and, despite being based on around 5537 largely well-to-do New Englander 30–74 year olds and their offspring, initially free from CVD, remains a reliable assessment of CVD risk in northern European populations (but overestimates risk in southern Europe, hence the SCORE project).1985385 [Google Scholar]
- 17.Pearson TA, Mensah GA, Alexander RW, et al. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation 2003;107:499–511. [DOI] [PubMed] [Google Scholar]
- 18.West R , McNeill A, Raw M. Smoking cessation guidelines for health professionals: an update. Thorax 2000;545:987–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eriksson J , Lindstrom J, Valle T, et al. Prevention of type II diabetes in subjects with impaired glucose tolerance: the diabetes prevention study (DPS) in Finland. Study design and 1-year interim report on the feasibility of the lifestyle intervention programme. Diabetologia 1999;42:793–801. [DOI] [PubMed] [Google Scholar]
- 20.Antiplatelet Trialists’ Collaboration. Collaborative overview of randomized trials of antiplatelet therapy, 1: prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. BMJ 1994;308:81–106. [PMC free article] [PubMed] [Google Scholar]