Abstract
Lipomatous hypertrophy of the interatrial septum is a benign cardiac mass that should be considered as part of the differential diagnosis for any atrial cardiac tumour. In the reported case, this lesion was initially suspected to be malignant and the patient was thus referred directly to cardiac surgeons for surgical removal. Unnecessary surgical intervention was swiftly averted because the cardiac surgeon promptly referred the patient for an expert echocardiogram that confirmed the diagnosis of lipomatous hypertrophy. The authors discuss the characteristic features of this lesion and how the diagnosis may be made based on several non-invasive imaging modalities without the need for a tissue biopsy. This condition is more common than initially thought and remains under-recognised by most clinicians. In such cases an increased awareness of this lesion along with the opinion of a specialist echocardiologist would help to avoid a misdiagnosis and unnecessary intervention.
Keywords: lipomatous hypertrophy, interatrial septum, cardiac mass and cardiac surgery
Lipomatous hypertrophy of the interatrial septum is a benign cardiac mass characterised as a non-encapsulated mass of fatty tissue that infiltrates the atrial septum. Although once described as a relatively rare finding, with the widespread use of echocardiography lipomatous hypertrophy is now being increasingly recognised and should be considered as part of the differential diagnosis for any atrial cardiac tumours. As most patients with this condition remain asymptomatic the majority of cases are generally picked up as an incidental finding at the time of cardiac imaging, surgery, or necropsy.1,2 Consequently this condition remains under-recognised by most clinicians and can thus be easily mistaken for a more sinister malignant lesion, subsequently leading to unwarranted surgical removal.3 We describe one such case where unnecessary intervention was avoided by a surgeon referring the patient back to a physician for a fresh opinion.
CASE REPORT
An 82 year old woman was referred from her local hospital with a suspected malignant intracardiac mass for a surgical biopsy followed by possible surgical removal. She had originally presented with a 12 month history of shortness of breath on exertion. At that time she had no history of weight loss or any other cardiorespiratory symptoms. On examination she was thin with no overt signs of heart failure. She had the murmur of moderate mitral regurgitation. Investigations included posteroanterior chest radiography, which showed an extrathoracic shadow initially thought to be a breast lesion. Subsequent mammography and computed tomography (CT) of her chest were reported as normal. To investigate a possible cardiac cause of her symptoms a transthoracic echocardiogram was recorded, which showed an intracardiac atrial septal lesion that was suspected to be malignant and thus was referred directly to the cardiac surgeons at a tertiary centre.
After transfer of the patient, the receiving cardiac surgeon requested a repeat transthoracic echocardiogram along with a second opinion from a cardiologist with a specialist interest in echocardiography. After transthoracic echocardiography the probable diagnosis was lipomatous hypertrophy of the interatrial septum (fig 1). The lesion was further evaluated by transoesophageal echocardiography (TOE) (fig 2) and cardiac magnetic resonance imaging (MRI) (fig 3) (Intera, Philips Medical Systems), which confirmed the diagnosis. Furthermore, TOE showed a prolapse of the posterior mitral valve leaflet leading to moderate mitral regurgitation, which was the probable cause of her shortness of breath. After her investigation and the optimisation of her medical treatment the benign nature of the atrial septal lesion was explained to the patient and she was discharged with local follow up.
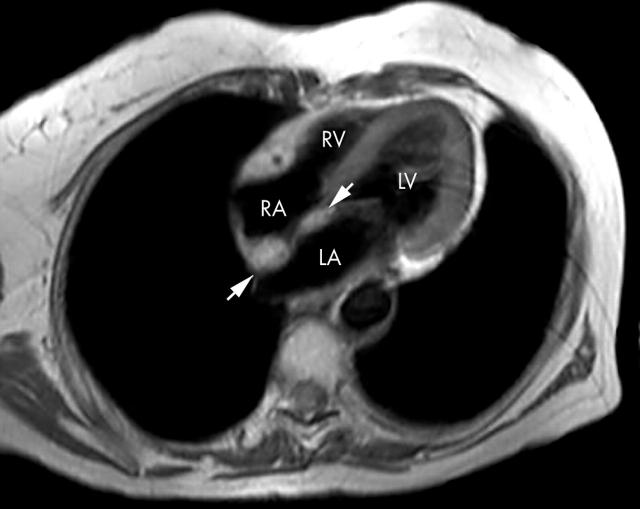
Figure 1.
Transthoracic echocardiogram showing lipomatous hypertrophy of the intra-atrial septum. Four chamber apical long axis view showing classic lipomatous hypertrophy of the atrial septum (arrows). LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle.
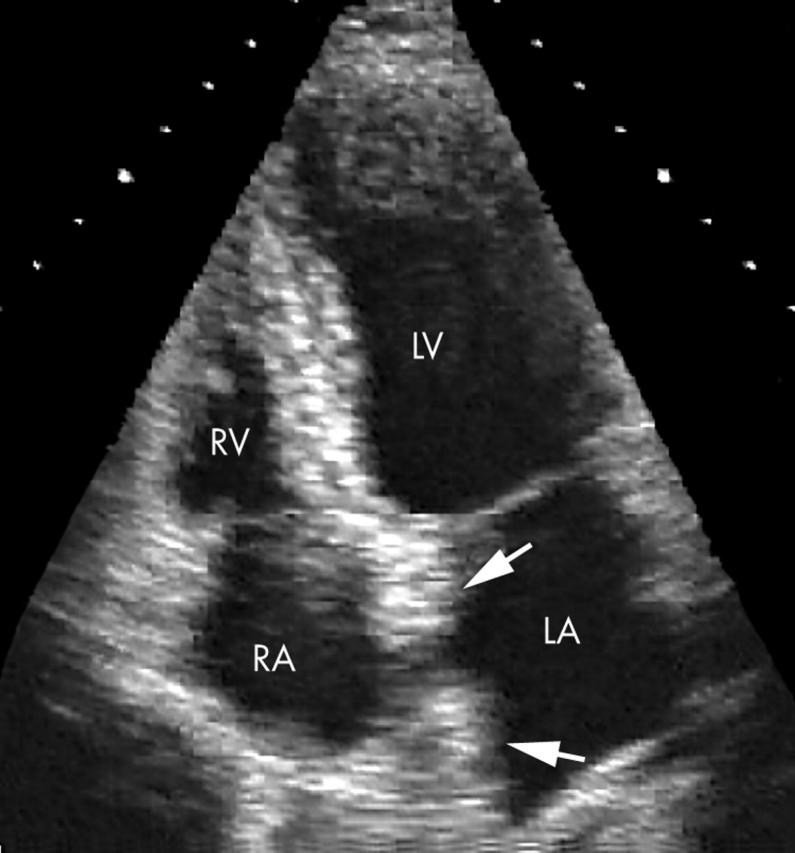
Figure 2.
Transoesophageal echocardiogram at the mid-oesophageal level showing the classic hour glass shaped lipomatous hypertrophy of the intra-atrial septum (arrow heads). Note the clearly defined septal borders along with the bright echogenicity of thickened tissue, which clearly spares the fossa ovalis (FO, arrow).
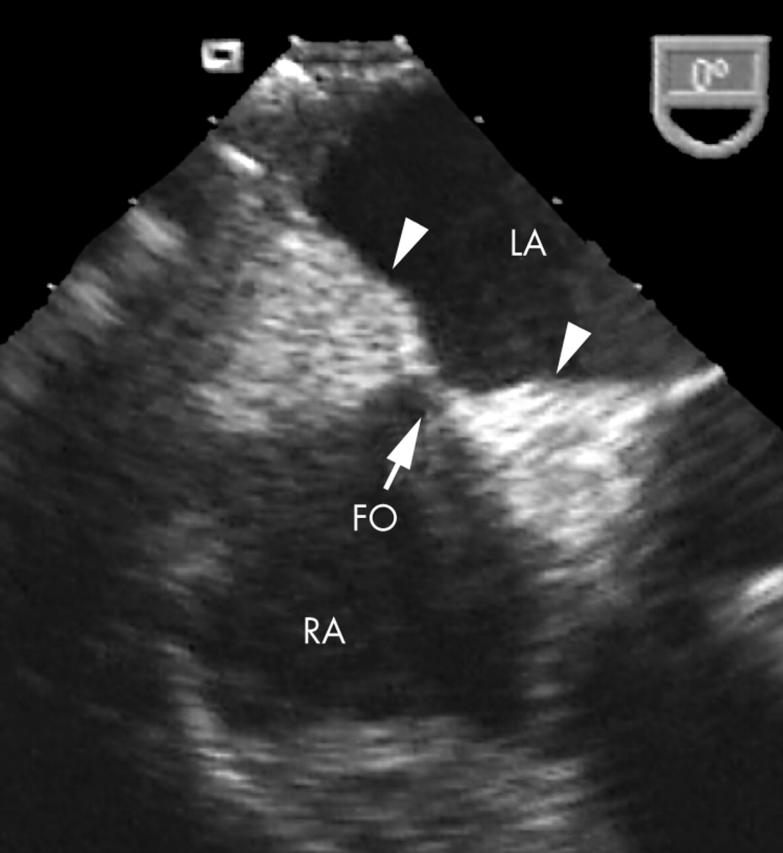
Figure 3.
Cardiac magnetic resonance image recorded at 3 T magnetic field strength with a body array coil. An ECG triggered breath hold turbospinecho sequence (repetition time 25 ms, echo time 1620 ms) in a four chamber view is shown. The atrial septum is thickened (arrows) on either side of the FO up to 18 mm. Characteristically the signal of the septal thickening is isointense to the subcutaneous fat.
DISCUSSION
Lipomatous hypertrophy of the cardiac interatrial septum was first described at a postmortem examination in 1964.4 Since then this condition has been reported widely in 88 case reports and original articles. Associated with increasing age and body mass, lipomatous hypertrophy has been reported to have an incidence between 1–8% depending on the series and methods used to detect the lesion (necropsy 1%,5 transthoracic echocardiography 8%6). In a recent large prospective study, 1292 patients undergoing multislice CT for other indications were reviewed for the presence of this disorder.7 The incidence was as high as 2.2% (29 patients) and was clearly associated with increasing age, confirming that lipomatous hypertrophy is more common than previously suspected. Although it is a benign tumour remaining asymptomatic in most people it may be associated with atrial arrhythmias often requiring antiarrhythmic agents.8 Only in the rare extreme cases of large lesions, which can cause circulatory obstruction, are patients required to undergo surgical resection and septal reconstruction.9,10 The best management consists of rapid diagnosis, reassurance, and masterly inactivity.
Histologically the lesion is characterised by a non-encapsulated mass of adipocytes interspersed with atypical and hypertrophied myocytes.11 Modern imaging techniques such as echocardiography, multislice CT, and MRI are the imaging modalities that may be used to diagnose this lesion,12 but expertise is essential to avoid misinterpretation. The defining characteristic feature is the specific septal location of the atrial thickening that tends to be greater than 2 cm and typically spares the fossa ovalis, hence taking on a classical dumbbell or hourglass shape. Furthermore, the tissue is isodense to the surrounding subcutaneous fatty tissue. As the structural features of this lesion are so distinct from any other intracardiac mass it is now widely accepted that the diagnosis can be made confidently without the need for tissue biopsy.
Our case clearly shows that the diagnosis can be easily and clearly made at the bedside based on transthoracic echocardiography and TOE. Although a clear diagnosis can also be based on MRI, this test remains an expensive technique localised to specialist centres. On retrospective review of the CT recorded at the referring hospital, not only was the lesion identifiable but also the characteristic diagnostic features described earlier were evident (fig 4). Each technique can establish the diagnosis but there will be cases that test the known limitations of each imaging modality. In such situations echocardiography used in combination with CT or MRI will help to make a complementary diagnosis.13,14
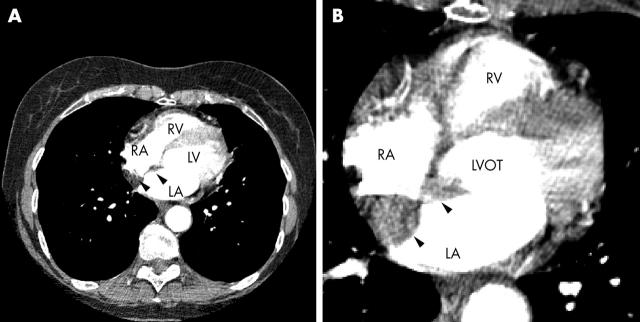
Figure 4.
Contrast enhanced multislice computed tomography (CT) of the thorax showing thickening of the intra-atrial septum (arrow heads). The axial slices of the body show the heart in an approximate four chamber view. (A) Lower cardiac section; (B) close up of a higher cardiac section. The contrast agent generated a high attenuation in the LV, LV outflow tract (LVOT), LA, RV, and RA. The septal thickening is clearly visualised. Note also that CT allows characterisation of the nature of the septal tissue, which is clearly hypointense to normal myocardium and has an attenuation similar to subcutaneous fat.
Taking into account the increasing age of the general population and the expanding use of non-invasive imaging techniques, the probability of identifying this lesion will increase. However, despite the reported common incidence we suggest that this condition is still under-recognised by all specialities and may easily, as in this case, lead to a misdiagnosis. Had the receiving surgeon not requested an expert echocardiogram our patient may well have undergone an unnecessary major surgical procedure, which carries in itself a significant risk. Good communication and discussion of new cases between complementing specialities is not only good medical practice but is also essential in correctly diagnosing common but under-recognised conditions such as this.
Important lesson
With patient transfers a fresh opinion from complementing specialities can often revise the working diagnosis and possibly avoid the need for unnecessary intervention. Imaging modalities do not lie, rather interpretation may vary depending on the level of expertise, no matter which modality this is.
Abbreviations
CT, computed tomography
MRI, magnetic resonance imaging
TOE, transoesophageal echocardiography
Funding: none.
Conflict of interest: none.
I Nadra wrote the report. D Dawson and SA Schmitz carried out the imaging of the patient. PP Punjabi and P Nihoyannopoulos were involved in managing the patient.
REFERENCES
- 1.Bhattacharjee M, Neligan MC, Dervan P. Lipomatous hypertrophy of the interatrial septum: an unusual intraoperative finding. Br Heart J 1991;65:49–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gay JD, Guileyardo JM, Townsend-Parchman JK, et al. Clinical and morphologic features of lipomatous hypertrophy (“massive fatty deposits”) of the interatrial septum. Am J Forensic Med Pathol 1996;17:43–8. [DOI] [PubMed] [Google Scholar]
- 3.Pharr JR, Figueredo VM. Lipomatus hypertrophy of the atrial septum and prominent crista terminalis appearing as a right atrial mass. Eur J Echocardiogr 2002;3:159–61. [DOI] [PubMed] [Google Scholar]
- 4.Prior JT. Lipomatous hypertrophy of cardiac interatrial septum: a lesion resembling hibernoma, lipoblastomatosis and infiltrating lipoma. Arch Pathol 1964;78:11–5. [PubMed] [Google Scholar]
- 5.Reyes CV, Jablokow VR. Lipomatous hypertrophy of the cardiac interatrial septum: a report of 38 cases and review of the literature. Am J Clin Pathol 1979;72:785–8. [DOI] [PubMed] [Google Scholar]
- 6.Pochis WT, Saeian K, Sagar KB. Usefulness of transesophageal echocardiography in diagnosing lipomatous hypertrophy of the atrial septum with comparison to transthoracic echocardiography. Am J Cardiol 1992;70:396–8. [DOI] [PubMed] [Google Scholar]
- 7.Heyer CM, Kagel T, Lemburg SP, et al. Lipomatous hypertrophy of the interatrial septum: a prospective study of incidence, imaging findings, and clinical symptoms. Chest 2003;124:2068–73. [DOI] [PubMed] [Google Scholar]
- 8.Hutter AM Jr, Page DL. Atrial arrhythmias and lipomatous hypertrophy of the cardiac interatrial septum. Am Heart J 1971;82:16–21. [DOI] [PubMed] [Google Scholar]
- 9.McNamara RF, Taylor AE, Panner BJ. Superior vena caval obstruction by lipomatous hypertrophy of the right atrium. Clin Cardiol 1987;10:609–10. [DOI] [PubMed] [Google Scholar]
- 10.Christiansen S, Stypmann J, Baba HA, et al. Surgical management of extensive lipomatous hypertrophy of the right atrium. Cardiovasc Surg 2000;8:88–90. [DOI] [PubMed] [Google Scholar]
- 11.Burke AP, Litovsky S, Virmani R. Lipomatous hypertrophy of the atrial septum presenting as a right atrial mass. Am J Surg Pathol 1996;20:678–85. [DOI] [PubMed] [Google Scholar]
- 12.Kindman LA, Wright A, Tye T, et al. Lipomatous hypertrophy of the interatrial septum: characterization by transesophageal and transthoracic echocardiography, magnetic resonance imaging, and computed tomography. J Am Soc Echocardiogr 1988;1:450–4. [DOI] [PubMed] [Google Scholar]
- 13.Simons M, Cabin HS, Jaffe CC. Lipomatous hypertrophy of the atrial septum: diagnosis by combined echocardiography and computerized tomography. Am J Cardiol 1984;54:465–6. [DOI] [PubMed] [Google Scholar]
- 14.Munoz J, Losada A, Ibanez M, et al. Lipomatous hypertrophy of the atrial septum: complementary diagnosis by transoesophageal echocardiography and nuclear magnetic resonance imaging. Eur Heart J 1996;17:1290–1. [DOI] [PubMed] [Google Scholar]