Abstract
In patients who are refractory to medical treatment of hypertrophic cardiomyopathy, surgical myomectomy or percutaneous transluminal alcohol septal myocardial ablation (PTSMA) is appropriate, with both the procedures having comparable results. In PTSMA ethanol is selectively injected into septal arteries supplying the hypertrophied septal myocardium. The authors describe a case of apical myocardial injury caused by passage of ethanol into the distal left anterior descending artery through a septal collateral that developed after double bolus injection of ethanol. They advocate single bolus injection of alcohol to avoid this complication.
Keywords: apical myocardial injury, hypertrophic cardiomyopathy, septal ablation
Hypertrophic cardiomyopathy (HCM) is a heterogenous genetic disorder characterised by primary myocardial hypertrophy. The interventricular septum is often involved, which may cause left ventricular outflow tract obstruction.1,2 β Blockers, verapamil, and disopyramide are the mainstay for treatment of patients who are symptomatic due to left ventricular outflow tract obstruction. However, in patients who are refractory to medical treatment surgical myomectomy or percutaneous transluminal alcohol septal myocardial ablation (PTSMA) is appropriate, with both the procedures having comparable results.3,4 In PTSMA ethanol is selectively injected into septal arteries supplying the hypertrophied septal myocardium. We describe a case of apical myocardial injury caused by passage of ethanol into the distal left anterior descending coronary artery (LAD) through a septal collateral that developed after double bolus injection of ethanol. We advocate single bolus injection of alcohol to avoid this complication.
CASE REPORT
A 53 year old woman was incidentally found to have a cardiac murmur during a visit to her doctor for flu-like symptoms. She also had a history of dyspnoea (New York Heart Association class II–III) and exertional chest pain. Transthoracic echocardiography was consistent with features of HCM with a septal thickness of 1.7 cm, systolic anterior motion of the mitral valve, an outflow tract gradient of 70 mm Hg at rest with a normal aortic valve, and good left ventricular function. She was intolerant of β blockers and calcium channel blockers and in view of continuing symptoms she underwent PTSMA.
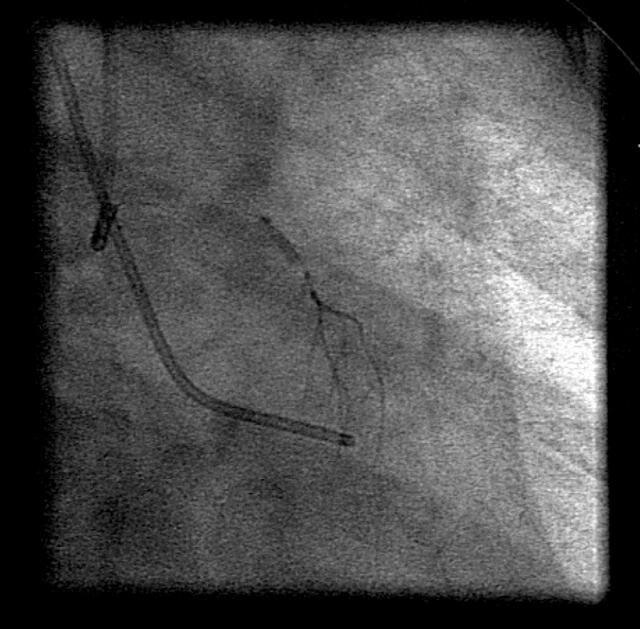
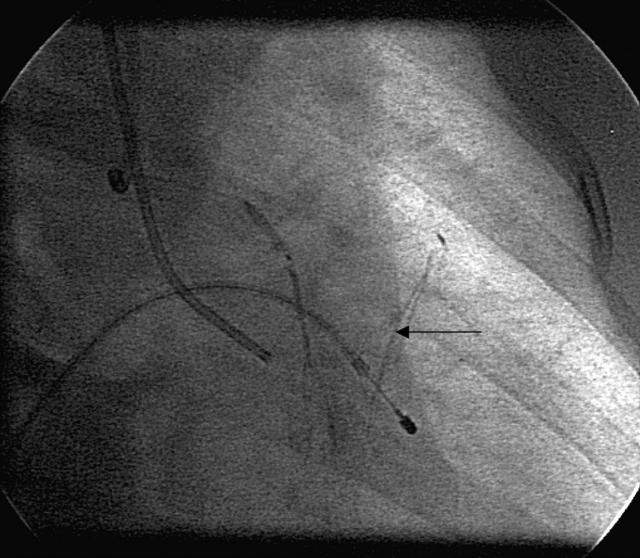
Coronary angiography before PTSMA showed normal coronary arteries with a large first septal artery with no evidence of collaterals. A resting gradient of 130 mm Hg was noted in the left ventricular outflow tract with postventricular extrasystolic accentuation. After wire access to the first septal artery and balloon inflation the gradient fell greatly. Contrast echocardiography confirmed that the first septal artery supplied the hypertrophic portion of the interventricular septum with no significant involvement of any other part of myocardium. No reflux of contrast from the septal artery into the LAD was confirmed (fig 1). After prophylactic analgesia administration, 1.5 ml of ethanol was injected slowly into the first septal artery causing ST depression in leads V1 and V2 and right bundle branch block. Repeat contrast echocardiography showed limited brightness in the septal region. A second injection of 0.5 ml of ethanol was given after an interval of 3–4 minutes. The patient complained of severe chest pain and developed 2:1 heart block and ST segment elevation in leads V1–V3. Repeat contrast injection down the balloon showed a collateral from first septal artery to the distal LAD and coronary angiography showed slow flow down the distal LAD beyond the collateral (fig 2). Echocardiography showed a localised segment of apical akinesia and a bright hypertrophied septum. The left ventricular outflow tract gradient fell to 30 mm Hg. The patient remained in 2:1 heart block for 40 minutes. An echocardiogram 60 minutes after the procedure showed complete resolution of the apical akinesia. The ST segment elevation on ECG resolved.
Figure 1.
Selective septal artery angiogram before ethanol ablation, with no collaterals.
Figure 2.
Angiogram after ethanol injection showing a collateral vessel between the septal artery and distal left anterior descending coronary artery (arrow).
DISCUSSION
PTSMA is now a recognised treatment for HCM and the outcomes are as good as with surgical myomectomy.3,4 PTSMA associated mortality is around 1–2% in experienced centres, comparable with myomectomy.3,5 Right bundle branch block and transitory heart block can be seen in 50% patients and 5–24% patients develop high degree atrioventricular block requiring a permanent pacemaker.3,6 Remote myocardial infarction during PTSMA is a recognised complication, particularly if the balloon is not fully occlusive and alcohol leaks back into the LAD causing anterior myocardial infarction. Myocardial free wall rupture and papillary muscle rupture have also been reported.7
Our patient developed apical myocardial injury due to passage of ethanol into a collateral branch from the first septal artery to the distal LAD. This collateral vessel was absent during the initial contrast injection but developed during the procedure. The first septal artery is the most common artery used for septal ablation and in most cases it supplies the obstructive portion of the septum, though it can supply a greater proportion of myocardium. Localisation of the septal territory of blood supply should be confirmed with contrast echocardiography to avoid these complications.8 Wustmann and colleagues9 showed that during brief coronary occlusion of a normal artery, 20% of patients have immediately recruitable collateral flow to the respective vascular area sufficient to prevent myocardial ischaemia. The myocardial infarct size is directly related to the volume of intracoronary absolute alcohol during myocardial ablation and has no relation to the injection velocity.10 In our patient there was no sign of anterior myocardial injury during the first 1.5 ml injection of ethanol. The last 0.5 ml of ethanol was injected after a gap of 3–4 minutes during which a contrast echocardiogram was recorded. We believe that after the first injection of ethanol, tissue oedema in the septal area developed leading to increased resistance to blood flow. This, together with the increased balloon inflation time and consequent ischaemia, led to the recruitment of the collateral artery between the first septal artery and the distal LAD.
This report shows that remote myocardial infarction may occur during PTSMA caused by collateralisation of the septal artery and can be avoided by a single bolus injection of ethanol. If a second injection is required the presence of collateral should be checked before the injection.
Abbreviations
HCM, hypertrophic cardiomyopathy
LAD, left anterior descending coronary artery
PTSMA, percutaneous transluminal alcohol septal myocardial ablation
There are no competing interests with this case report.
REFERENCES
- 1.Maron BJ, McKenna WJ, Danielson GK, et al. American College of Cardiology/European Society of Cardiology clinical expert consensus document on hypertrophic cardiomyopathy. J Am Coll Cardiol 2003;42:1687–713. [DOI] [PubMed] [Google Scholar]
- 2.Maron MS, Olivotto I, Betocchi S, et al. Effect of left ventricular outflow tract obstruction on clinical outcome in hypertrophic cardiomyopathy. N Engl J Med 2003;348:295–303. [DOI] [PubMed] [Google Scholar]
- 3.Qin XJ, Shiota T, Lever HM, et al. Outcome of patients with hypertrophic obstructive cardiomyopathy after percutaneous transluminal septal myocardial ablation and septal myomectomy surgery. J Am Coll Cardiol 2001;38:1994–2000. [DOI] [PubMed] [Google Scholar]
- 4.Nagueh SF, Ommen SR, Lakkis NM, et al. Comparison of ethanol septal reduction therapy with surgical myectomy for the treatment of hypertrophic cardiomyopathy. J Am Coll Cardiol 2001;38:1701–6. [DOI] [PubMed] [Google Scholar]
- 5.Gietzen FH, Leuner CJ, Obergassel L, et al. Role of transcoronary ablation of septal hypertrophy in patients with hypertrophic cardiomyopathy, NYHA functional class III–IV, and outflow tract obstruction only under provocable conditions. Circulation 2002;106:454–9. [DOI] [PubMed] [Google Scholar]
- 6.Seggewiss H, Gleichmann U, Faber L, et al. Percutaneous transluminal septal myocardial ablation in hypertrophic obstructive cardiomyopathy: acute results and 3-month follow-up in 25 patients. J Am Coll Cardiol 1998;31:252–8. [DOI] [PubMed] [Google Scholar]
- 7.Ruzyllo W, Chojnowska L, Demkow M, et al. Left ventricular outflow tract gradient decrease with non-surgical myocardial reduction improves exercise capacity in patients with hypertrophic obstructive cardiomyopathy. Eur Heart J 2000;21:770–7. [DOI] [PubMed] [Google Scholar]
- 8.Faber L, Meissner A, Ziemssen P, et al. Percutaneous transluminal septal myocardial ablation for hypertrophic cardiomyopathy. Heart 2000;83:326–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wustmann K, Zbinden S, Windecker S, et al. Is there functional collateral flow during vascular occlusion in angiographically normal coronary arteries? Circulation 2003;107:2213–20. [DOI] [PubMed] [Google Scholar]
- 10.Li QZ, Cheng OT, Li Liu. et al Experimental study of relationship between intracoronary alcohol injection and the size of resultant myocardial infarct. Int J Cardiol 2003;9:93–6. [DOI] [PubMed] [Google Scholar]