Several investigators around the turn of the 19th century confirmed the association between coronary artery occlusion, coronary artery reperfusion and ventricular fibrillation (VF) experimentally.w1 MacWilliam was probably the first to recognise the clinical importance of these findings in humans, suggesting in 1889 that syncope could result from coronary occlusion, VF with loss of cardiac output.w1 MacWilliam also described termination of VF in man that was achieved by repetitive electric shocks applied through a large pair of electrodes placed over the cardiac apex and the sixth or seventh dorsal vertebra.w2
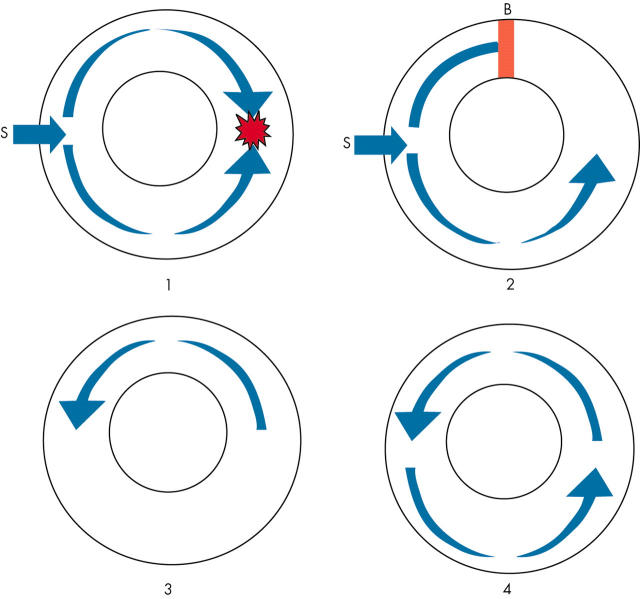
Mines and Garrey subsequently described the role of re-entry as a mechanism for fibrillation in the early part of the 20th century.w1 Mines suggested that an area of conduction block must be present to facilitate re-entry.w1 This observation is explained in fig 1. Prolonged myocardial repolarisation will provide an area of functional conduction block (as occurs in ischaemic ventricular tissue) and thus a substrate for re-entry.
Figure 1.
Re-entry. In normal tissue (panel 1) an electrical stimulus (S) will produce wavefronts that travel in both directions. These will collide and die out. In panel 2, an area of conduction block is present (B). The upper wavefront produced by the stimulus (S) dies out as it encounters the area of block. However, the lower wavefront continues to travel around the tissue. By the time this wavefront reaches the upper half of the ring of cardiac tissue, the conduction block has resolved and a re-entrant wavefront is established (panels 3 and 4).
Garrey also noted that a “critical mass” of cardiac tissue was required to maintain fibrillation.w2 These seminal observations have provided a foundation for our understanding of ventricular fibrillation.
It is generally agreed that spontaneous re-entrant arrhythmias can be initiated by the interaction between a propagating wavefront and an obstacle in its path (for example, an area of conduction block such as an old infarction scar) or triggered by a spontaneous premature beat.w2 Where a wavefront interacts with an area of conduction block, a re-entrant arrhythmia can begin as vortices that initiate in a figure-of-8 configuration.w2 This process eventually results in multiple daughter wavelets that are capable of creating new vortices and wavebreaks in a continuous self perpetuating manner.w2 In VF, the human heart most likely accommodates a relatively small number of drifting scroll like waves (or vortices) that interact with each other in complex spatio-temporal patterns.w2
Defibrillation of VF aims to bring an abrupt halt to this process and rapidly restore normal cardiac rhythm and cardiac output, thus preventing sudden death. Occasionally, a chest blow to the lower end of the sternum will correct VF but the majority require electrical defibrillation.
CELLULAR EFFECTS OF DEFIBRILLATING SHOCKS
To date, the exact mechanisms behind electrical defibrillation remain incompletely understood. It is thought that shocks defibrillate by altering the potential difference across the cell membrane (that is, the transmembrane potential).1 However, the situation in the heart is extremely complex with the intracellular space and extracellular space both possessing different electrical properties than the membrane that divides them.1 Early electrical mapping studies suggested that cells nearest the anode become hyperpolarised, while cells nearest the cathode become depolarised. The amount of hyperpolarisation and depolarisation is directly linked to the extracellular potential gradient.1 However, there is no current consensus on how this extracellular potential gradient relates to the transmembrane potential gradient. Furthermore, instead of hyperpolarisation and depolarisation closely spaced at opposite ends of cells or cell bundles due to a high intracellular resistance at these sites, considerably larger regions of depolarisation and hyperpolarisation have been reported.2 In addition, membrane depolarisation is also strongly influenced by tissue anisotropy (tissue resistivity is anisotropic—that is, it is increased if current flows transverse to the long axis of the muscle fibres rather than along it) and the curvature of myofibres. Thus, different regions exposed to identical stimuli could undergo notably different changes in membrane polarisation.2
We have described the importance of field strength (above 5 V/cm) for stimulation of refractory myocardium in our previous article in this series.w3 The production of a graded response from refractory cells has also been described.w3 Some authors believe that prolongation of refractoriness is of crucial importance for successful defibrillation.w4 In theory, extension of the refractory period of a sufficient number of cells will cause fibrillatory activation fronts to encounter refractory tissue and thus die out. However, others have suggested that for successful defibrillation a shock must depolarise myocardial tissue, even during its refractory period.w5
PROPOSED MECHANISMS OF DEFIBRILLATION
It is known that a critical mass of tissue is necessary to sustain VF. Zipes and colleaguesw6 subsequently demonstrated that chemical depolarisation of a critical mass of myocardium, using selective infusion of potassium chloride into the left coronary artery, would abolish fibrillation. Therefore, if a sufficient voltage potential gradient could be generated by a shock to halt the fibrillation activation fronts in the myocardium, fibrillation could be abolished. Indeed small areas that still support activation wavefronts have been shown to exist after a shock.1 These fronts arise in regions where the potential gradients produced by the shock are lowest.1 In theory, a shock can be successful if a critical mass of myocardium is successfully defibrillated while still leaving a small mass of fibrillating tissue that is insufficient to sustain the arrhythmia.
A lower limit of vulnerability exists for myocardium.2 This is the minimum strength required by an electrical stimulus to induce fibrillation during the vulnerable period. It was noted in the 1960s that there was an upper limit to the strengths of shocks delivered during the vulnerable period that induce VF.2 It was also noted that the strengths of these shocks at “the upper limit of vulnerability” were approximately equivalent to the shocks at defibrillation threshold.2 It has subsequently been shown that induced re-entry circuits could be made to behave predictably.2 When electrodes were applied and two additional stimuli (S1 and S2) were delivered to myocardium to induce fibrillation, it was noted that the direction of rotation and position of the resulting re-entry circuit could be manipulated according to the location of the stimulating electrodes and adjusting the interval between the S1 and S2 stimuli.2 In addition, an area of critical potential gradient existed where re-entry occurred. This was located at a distance from the S2 electrode, which increased in proportion to the shock stimulus.2 As the S2 stimulus increased in strength from the VF “induction” threshold (lower limit of vulnerability) toward the upper limit of vulnerability, the site of re-entry moved progressively from near the S2 electrode to an increasingly distant portion of the ventricles where the shock potential gradient was weakest.2
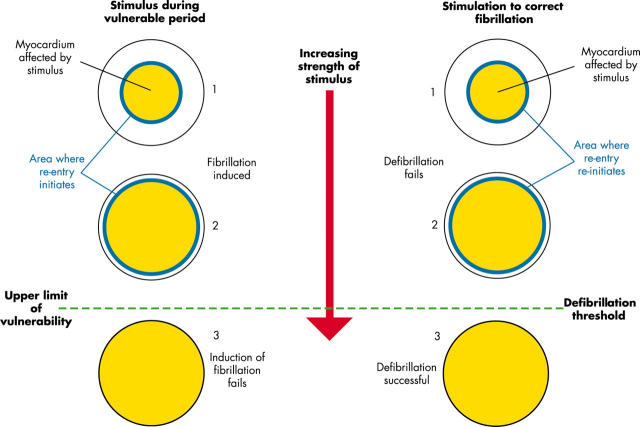
Shocks of the same strength delivered during VF (that is, attempted defibrillation) also produced a similar region of lowest shock potential gradient, and this area was the source of earliest activation that propagated globally across the epicardium and allowed fibrillation to continue.2 These effects are summarised in fig 2. The upper limit of vulnerability hypothesis for defibrillation states “to defibrillate, a shock not only must halt the activation fronts of fibrillation, but it also must not reinitiate fibrillation by the same mechanism that a shock of the same strength during the vulnerable period of sinus or paced rhythm initiates fibrillation”.2
Figure 2.
Relation between the upper limit of vulnerability and defibrillation threshold. The myocardium affected by the electrical stimulus is represented in yellow. In the left half of the diagram shocks are delivered to induce VF during the vulnerable period while in the right half of the diagram shocks are delivered during VF to attempt defibrillation. As the strength of electrical stimulus increases from 1 to 2, the area of myocardium affected increases. The zone where re-entry occurs after the shock (blue region) moves away from the area where the shock is delivered. A further increase in the intensity of stimulus (3) affects all of the myocardium and prevents induction of VF above the upper limit of vulnerability and successfully defibrillates above the defibrillation threshold.
Recent data have provided insight into why shocks fail. Ongoing propagation of re-entry is mainly responsible for failure of defibrillation for low strength shocks, while focal activation is responsible for shock failure near defibrillation threshold.w7 This raises the possibility that pharmacological interventions may enhance defibrillation efficacy.
In an effort to unify existing hypotheses for defibrillation, Dillon and Kwaku have introduced the idea of progressive depolarisation: “Progressively stronger shocks depolarize, progressively more refractory myocardium, to progressively prevent postshock wavefronts, and prolong and synchronize postshock repolarisation, in a progressively larger volume of the ventricle, to progressively decrease the probability of fibrillation after the shock.”3
In summary, the relation between a defibrillating shock and myocardial cells is extremely complex and influenced by many variables. A critical electrical stimulus must be applied to fibrillating tissue in order to achieve successful defibrillation. This stimulus must produce a sufficient potential gradient to alter the transmembrane potential in an adequate proportion of the fibrillating tissue. Furthermore, the stimulus must not lead to the development of reactivation fronts. The precise ionic actions that lead to this process are incompletely understood. Each of the current theories of defibrillation has merit, and is likely to play a significant role in the process. However, they are neither mutually exclusive nor all encompassing.
DEFIBRILLATION IN CLINICAL PRACTICE
A description of defibrillation waveforms and their production is given in our previous article in this series.w3 Transthoracic monophasic defibrillators have been employed for the management of cardiac arrest caused by ventricular arrhythmias for over four decades. There is a universally agreed protocol for the electrode positions and energies that should be used to treat ventricular arrhythmias with these waveforms.4 Current UK guidelines recommend a 200 J, 200 J, 360 J sequence with subsequent shocks at 360 J if the arrhythmia is uncorrected.5
However, many studies of ventricular fibrillation have confirmed the superiority of various biphasic waveforms over monophasic pulses of equivalent or similar duration. Biphasic waveforms offer equivalent or superior efficacy at lower energy and peak voltage than their monophasic counterparts. This has been shown in animal models of transthoracic defibrillationw8–w13 and epicardial defibrillation.w14–w19 Endocardial defibrillation systems also perform better with biphasic waveforms in animalsw20–w24 and clinical studies.w25–w28 In addition, biphasic shocks have also been shown to be less deleterious to myocardial function in epicardial or transthoracic animal models of ventricular defibrillation.w9 w11 w29
TRANSTHORACIC IMPEDANCE
Transthoracic impedance (TTI) has been recognised as an important determinant of successful defibrillation.4w30 Defibrillation is accomplished by passage of sufficient electric current through the heart. The energy chosen and the TTI, or resistance to current flow, determine the current flow. Factors that determine TTI include energy selected, electrode size, paddle–skin coupling material, number and time interval of previous shocks, phase of ventilation, distance between electrodes (size of the chest), and paddle electrode pressure.4 It is also known that high current densities within myocardial tissue may adversely affect outcome by directly injuring myocardial cells, or by inducing post-shock dysfunction and refibrillation.w4 Recent developments have therefore focused on enhancing the delivery of energy to the myocardium. The modern generation of biphasic defibrillators are calibrated to alter the waveform delivered to the patient based on TTI (that is, impedance compensated biphasic waveforms (ICB)). These devices aim to deliver a shock “dose” that is proportional to each patient. Therefore, patients with low TTI (typically smaller and lighter) receive a similar energy to those with higher TTI (usually larger heavier patients). Different approaches are employed to achieve this goal, including adjusting peak voltage (or current), waveform tilt, and waveform duration. There are subtle differences for both the methods of impedance compensation and the waveforms delivered for different manufacturers’ devices, and ICB waveform defibrillation is not strictly “current based” (where an identical peak current is delivered to the myocardium for each patient) at present, although this approach shows promise.w31 In addition, the optimal energies have not been identified for ICB defibrillation and there is no universally agreed energy selection protocol at present.
CLINICAL STUDIES COMPARING MONOPHASIC AND BIPHASIC WAVEFORMS
Several clinical studies have evaluated modern ICB waveforms compared with their monophasic equivalents in the clinical setting. Mittal and colleagues6 compared a rectilinear biphasic waveform at 120 J (Zoll PD-2100 defibrillator) with a damped sine wave at 200 J in the electrophysiology laboratory. A total of 184 patients were included in the study (98 biphasic, 86 monophasic) and induced VF was the treated rhythm in 146 patients (74 biphasic, 72 monophasic). Successful defibrillation was defined as conversion of ventricular tachycardia or ventricular fibrillation to a supraventricular or paced rhythm associated with a measurable blood pressure and pulse that persisted for at least 30 seconds post shock. First shock efficacy of the biphasic waveform was greater than that of the monophasic waveform (99% v 93%, p = 0.05) and was achieved with nearly 60% less delivered current (14±1 A v 33±7 A, p < 0.0001). However, these results should be interpreted with caution. The authors did not comment on the duration of arrhythmia before defibrillation (presumably this was < 1 minute for all patients) and the electrophysiology laboratory is clearly not representative of a collapse episode caused by VF or pulseless VT.
Schneider and colleagues compared an ICB automated external defibrillator (Agilent Forerunner) with several monophasic devices (delivering either damped sine wave or monophasic truncated exponential waveforms) in patients with out-of-hospital cardiac arrest.7 Biphasic shocks were delivered in a 150 J, 150 J, 150 J sequence, while monophasic shocks were delivered in a 200 J, 200 J, 360 J sequence. Responders were not blinded to the delivered waveform. A total of 115 patients (54 biphasic, 61 monophasic) presented with VF: only the first episode was included for analysis. The primary end point of the study was the percentage of patients with VF who were defibrillated in the first series of ⩽ 3 shocks (defibrillation was defined as termination of VF for ⩾ 5 seconds). The average time from the emergency call to the first shock was 8.9 minutes. More patients were defibrillated with the initial biphasic shock than with the initial monophasic shock (96% v 59%; p < 0.0001) and more patients (76%) achieved return of spontaneous circulation (ROSC) after biphasic defibrillation compared with higher energy monophasic defibrillation (54%; p = 0.01). For the primary end point of defibrillation within the first shock series, 98% of VF patients were defibrillated with 150 J biphasic shocks compared with 69% of patients defibrillated with 200–360 J monophasic shocks (p < 0.0001).
Most recently van Alem and colleagues8 compared the success of biphasic (Medtronic Physio-Control LIFEPAK 500) and monophasic (damped sine wave) shocks for defibrillation in out-of-hospital cardiac arrest in a prospective, randomised, double blind clinical trial.8 The shock protocol for both waveforms was 200 J, 200 J, 360 J (and 360 J for each shock thereafter as needed for defibrillation). Patients had both witnessed and non-witnessed cardiac arrest with VF as the initial recorded rhythm. The primary end point was removal of VF with a return of an organised rhythm within one minute after the first shock. The secondary end point was termination of VF at five seconds after the first shock. VF was the initial recorded rhythm in 120 patients (51 biphasic, 69 monophasic). The success rate of 200 J first shocks was significantly higher for biphasic than for monophasic shocks (35/51 (69%) and 31/69 (45%); p = 0.01).
ENERGY SELECTION FOR BIPHASIC DEFIBRILLATORS
Energy selection for biphasic waveforms and the best method of impedance compensation is still hotly debated.
Recently, it was shown that different transthoracic ICB devices behave differently over a range of TTI in an animal model of cardiac arrest caused by VF with an external resistance placed in the circuit to resemble human TTI.9 The odds ratio of successful defibrillation with an ICB waveform was 11.5 times greater than for a monophasic damped sine (MDS) waveform (95% confidence interval (CI) 8.3 to 15.8) and 53.7 times greater than for a monophasic truncated exponential (MTE) waveform (95% CI 31 to 94). Interestingly, the MDS waveform achieved a significantly higher success rate than the MTE waveform (odds ratio 4.7, 95% CI 2.8 to 7.8). The authors concluded: “Despite impedance-compensation schemes in biphasic defibrillators, impedance has an impact on their efficacy. At high-impedance, modest efficacy differences exist among clinically available biphasic defibrillators, reflecting differences in both waveforms and manufacturer provided doses.” These conclusions were heavily criticised.10 It was noted that the results were out of context with previously published clinical data. It was suggested that the animal ± electronic surrogate model of high impedance defibrillation was inappropriate and the correspondents questioned whether the application of these results to the clinical setting would in fact be harmful. The main rationale for this argument was that only a limited fraction of the shock dose was delivered to the animals in contrast to the clinical setting where patients with higher TTI receive the full dose.10 In reply, Walker and colleagues11 stated that their animal model was appropriate for comparison of relative efficacy between devices and the method of simulating high impedance served this purpose well. However, recent animal data have suggested that higher energy biphasic shocks impact negatively on haemodynamic function after defibrillation.12
It is therefore difficult for clinicians to place the results obtained from these clinical and animal studies in context. Further retrospective studies in patients have also suggested that monophasic truncated exponential waveforms may be inferior to damped sine wave monophasic pulses (as well as biphasic waveforms).13,14 It is inevitable that practice is going to switch to ICB waveform based defibrillation. When ICB devices are used for ventricular defibrillation, the clinician should use manufacturer recommended energies. Our own experience with ICB waveforms shows a lower efficacy for these devices when “all comers” with cardiac arrest and ventricular arrhythmia were included in a clinical trial.w32 The excellent results achieved with these devices in clinical studies with strict criteria are not duplicated in clinical practice. Our results suggest that ICB waveform energy selection requires widespread clinical evaluation before universal guidelines can be developed.
TRIPHASIC WAVEFORMS
Experience with triphasic waveforms has been conflicting and is limited to animal models. Initial studies suggest that these waveforms do not appear to have any significant advantage over their biphasic counterparts.w33 w34 However, one recent publication found some increase in efficacy at low energies.w35 At present, triphasic waveforms remain experimental.
AUTOMATED EXTERNAL DEFIBRILLATORS AND PUBLIC ACCESS DEFIBRILLATION
It is widely accepted that increasing the duration of VF reduces the likelihood of survival, and that the majority of out-of-hospital cardiac arrests occur in the home. Experience from the management of cardiac arrest in Seattle shows almost 100% survival for patients with VF who receive immediate treatment, while only 5% survive if treatment is delayed for more than 10 minutes.15 At present most emergency medical service (EMS) response times are longer than eight minutes, and survival rates from cardiac arrest are only 5–10% for most communities.15 Furthermore, the Guidelines 2000 conference concluded, “Early defibrillation (shock delivery within 5 minutes of EMS call receipt) is a high-priority goal”.16 Therefore, the most practical strategy to improve survival is reducing call-to-response interval by use of public access defibrillation (PAD) programmes. PAD incorporates the use of automated external defibrillators (AEDs) for out-of-hospital sudden cardiac arrests by members of the public with no formal medical background.
AEDs have been available since 1979,w36 and were able to recognise cardiac rhythm via pads in the mid 1980s.w37 These devices incorporate a rhythm analysis system and a shock advisory system. The AED can be semi-automated (the machine instructs the responder to deliver a shock) or fully automated (where the device delivers the shock automatically).16 Devices intended for use by the public are usually smaller and lighter, and have no screen for rhythm interpretation (fig 3).
Figure 3.
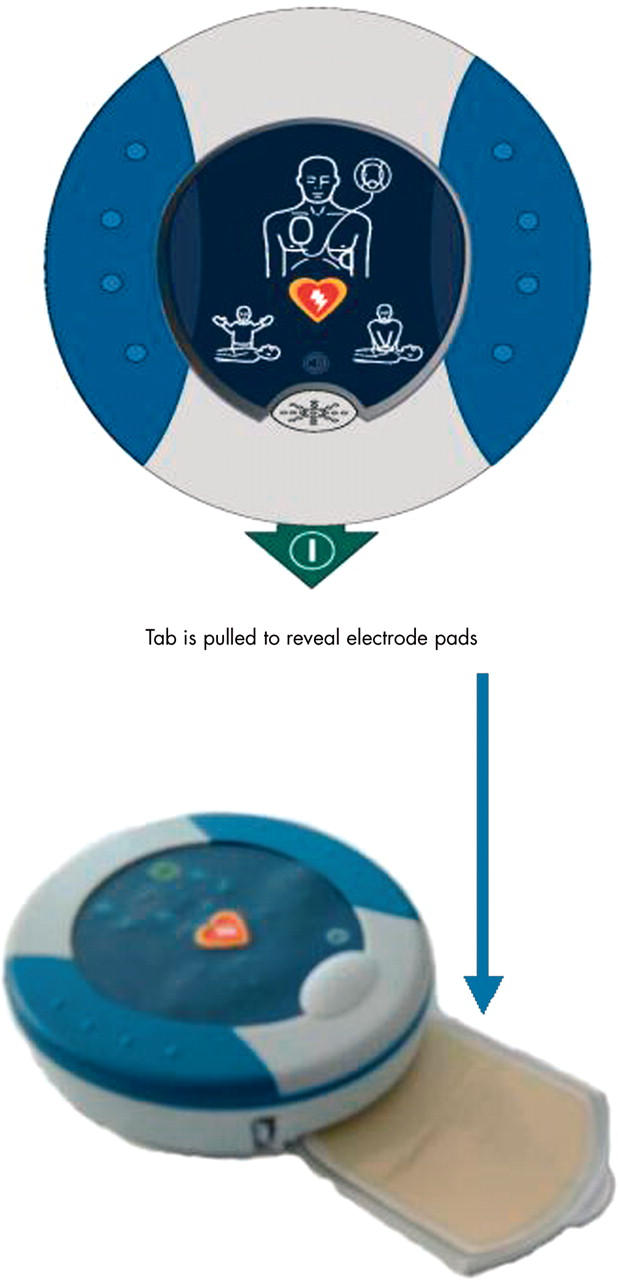
Automated external defibrillator (AED) intended for use by the general public (weight 1 kg).
Approaches to PAD programmes
The American Heart Association (AHA)16 and the European Resuscitation Council (ERC)17 have both endorsed PAD in recent scientific statements. There are two distinct approaches to AED deployment in the community. The devices can be placed in mobile units with first responders (police, fire personnel, district nurses, or lay personnel) or at fixed locations, where there is a reasonable chance of a cardiac arrest occurring. At present the AHA suggest deployment of PAD programmes when: (1) the frequency of cardiac arrest events is such that there is a reasonable probability of AED use; (2) an EMS call-to-shock time interval of less than five minutes cannot be reliably achieved with conventional EMS services; and (3) an EMS call–to-shock time interval of less than five minutes can be reliably achieved (in > 90% of cases) by training and equipping laypersons to function as first responders in the community EMS system, recognising cardiac arrest, phoning an emergency telephone number, initiating cardiopulmonary resuscitation (CPR), and attaching/operating an AED.16
Clinical studies of PAD programmes
Studies have demonstrated that equipping mobile first responders (police officers) with AEDs could reduce the time to defibrillation and increase survival rates among victims of cardiac arrest to 26–40%.w38 w39 When police officers were equipped with AEDs in Miami, they responded to cardiac arrests more quickly than conventional EMS and significantly increased survival rates for those with VF/VT from 9% to 17% (p = 0.047).w40
Other studies provided valuable information regarding the value of placing static AEDs in strategic locations such as airports,w41 aeroplanes,w42 w43 and casinosw44 where sudden cardiac arrests can be expected to occur and training personnel to use them is relatively straightforward. Caffrey and colleaguesw41 examined AED placement in Chicago airports and demonstrated high levels of survival (with good neurologic function) for those with cardiac arrest caused by VF. Page and colleaguesw43 described the results of the decision by American Airlines in 1997 to equip its aircraft with defibrillators. The programme was highly effective for victims who were found to have VF. Of these, 40% survived to discharge from the hospital with full neurologic and functional recovery. Valenzuela and colleaguesw44 reported the results of a programme that trained security officers in casinos in the use of AEDs. The mean time to defibrillation by security guards was 4.4 minutes compared with 9.8 minutes from collapse to the arrival of EMS. The rate of survival to hospital discharge was 53%, and all survivors were able to care for themselves.
A study from Italy compared resuscitation success for patients managed initially by PAD volunteers and those with the traditional EMS response. A hybrid approach of mobile and static AEDs was used. They found that when the PAD volunteers initiated defibrillation there was a tripling in the rate of survival to hospital discharge from 3.3% to 10.5% (p = 0.006), for those with “shockable” rhythms the survival rate increased from 21.2% to 44.1% (p = 0.046), and neurologically intact survival was improved from 2.4% to 8.4% (p = 0.009). These PAD volunteers did not receive traditional education in CPR.w45
More recently the results of “PAD: the public access defibrillation trial” were presented at the 2003 American Heart Association meeting. This interesting prospective randomised trial was initiated to evaluate whether the addition of AEDs to a CPR based community volunteer response system increases survival in victims of out-of-hospital cardiac arrest living in community units defined as high risk. A total of 14.6% of the CPR only group survived to discharge compared to 22.5% of the CPR and AED group (p = 0.042). The investigators concluded that trained laypersons can use AEDs safely to provide early defibrillation with a resulting improved survival. Of interest the survival rate in multi-unit residential facilities was very low and there was no difference between the two groups.w46
Although some studies demonstrate success with AED use, others have shown no benefit. In a retrospective analysis of the impact of the introduction of an AED into an established EMS, Stotz and colleaguesw47 found no significant survival advantage for witnessed out-of-hospital cardiac arrest victims despite time to defibrillation being significantly improved (5.7 minutes v 15.6 minutes). Another study found that low density populations derived no benefit from AED use by EMS personnel.w48
It should also be noted that the potential benefits from introduction of AEDs will not be maximised unless other links in the “chain of survival” are optimised.w49 In addition, the recently published European Society of Cardiology/European Resuscitation Council (ESC/ERC) recommendation for the use of AEDs in Europe state that each programme should be tailored to each specific environment. They recognise that each project needs to achieve a compromise between the widespread distribution of AEDs and the economic feasibility of the programme in terms of available resources.17 The UK government published the white paper Saving lives: our healthier nation in 1999.w50 This document included plans for “ training for members of the public in the use of defibrillators”. In response the government led national PAD project has been established in England.w51 To date, almost 700 AEDs have been sited, with over 6000 first responders trained resulting in 37 survivors of cardiac arrest (event to discharge).w52
Defibrillation for ventricular fibrillation: key points.
Ventricular fibrillation is a re-entrant arrhythmia, where a small number of self sustaining vortices maintain ventricular electrical activity without cardiac output
The critical mass and upper limit of vulnerability hypotheses are central theories for mechanisms of defibrillation
During transthoracic ventricular defibrillation with monophasic waveforms shocks should be given in a 200 J, 200 J, 360 J sequence with further shocks delivered at 360 J if the arrhythmia is not removed
Biphasic waveforms are superior to monophasic waveforms for transthoracic ventricular defibrillation
A number of defibrillators that deliver impedance compensated biphasic waveforms are available for ventricular defibrillation. These should be used according to manufacturer specified guidelines
No universal guidelines exist for biphasic waveforms and ventricular defibrillation. There is no evidence to suggest that any one biphasic defibrillator is superior to another
Automated external defibrillators are safe and effective for the treatment of ventricular fibrillation. These devices can be safely used by lay rescuers with minimal training
Public access defibrillation programmes improve outcomes in cardiac arrest. However, the cost benefit ratio of these programmes has not been established
Implementation of public access defibrillation programmes should be specific for each region where they are applied
Cost effectiveness of PAD programmes
The potential impact of public access defibrillators in Scotland on survival after out of hospital cardiopulmonary arrest was examined in 2002.w53 The authors concluded that the predicted increase in survival from targeted provision of public access defibrillators is less than the increase achievable through expansion of first responder defibrillation to nonambulance personnel or of bystander cardiopulmonary resuscitation.w53 The same group also found modelling of costs of locating defibrillators in all major airports, railway stations, and bus stations throughout Scotland resulted in costs of £29 625 for each life year gained and £41 146 for each quality adjusted life-year (QALY). They concluded that these costs represent poorer value for money than some alternative strategies, such as the use of other trained first responders, and exceed the commonly used cut-off levels for funding in the UK and USA.w54 However, a cost analysis based on the previously mentioned casinos studyw44 found that such a strategy was associated with an incremental cost effectiveness ratio similar to those of other common medical interventions.w55
Improving outcomes with AEDs
Evidence is also accumulating that demonstrates an important interaction between CPR and defibrillation. Steen and colleagues18 conducted a study in which VF was induced for 6.5 minutes in pigs. In group 1, defibrillation was the only treatment carried out. In group 2, CPR was carried out for 3.5 minutes before delayed defibrillation (a 40 second hands free interval occurred pre-shock to simulate AED use). If unsuccessful, CPR was resumed for a further 30 seconds before a second or a third delayed shock was given. In group 3, CPR was applied for 3.5 minutes after which up to three shocks were given during ongoing CPR. Return of spontaneous circulation occurred in none of the pigs in group 1, in one of six pigs in group 2, and in five of six pigs in group 3. The authors concluded that adequate heart massage before and during defibrillation greatly improved the likelihood of return of spontaneous circulation.18
In another study defibrillation with an AED performed as recommended by the manufacturer, and manual defibrillation (performed as per guidelines), was compared in a pig model of VF. Return of spontaneous circulation within five minutes of simulated defibrillator arrival occurred in only one of eight animals in the automated external defibrillator group versus six of eight animals in the manual defibrillation group. This was attributed to the longer delays in resumption of chest compressions after a shock with an AED defibrillator versus manual defibrillation. The mean percentage of time that chest compressions were performed in the first minute after the first countershock was 15% versus 40% for the AED and manual groups, respectively.19
A recent review of this topic has been published.20 This review also referred to a study that analysed the performance of experienced first responders where an average of 40% of the potential time available for chest compressions was lost because of AED voice prompts.21 The authors concluded that formidable evidence is emerging that new emphasis is required on the way in which chest compression is performed to improve defibrillation outcomes.20 If this focus on “hands off time” is incorporated into forthcoming new guidelines from the International Liaison Committee on Resuscitation it will alter current algorithms for the use of AEDs. This in turn may affect how AED programmes are organised to best meet local needs.
CONCLUSIONS AND FUTURE DEVELOPMENTS
There have been major advances in cardiopulmonary resuscitation and ventricular defibrillation over the last decade. The field of resuscitation continues to evolve rapidly. It is clear that biphasic defibrillators are superior to their monophasic counterparts and these devices will quickly replace monophasic defibrillators. We anticipate an increasing evidence base regarding the use of these devices in the near future. This will hopefully culminate in a universal treatment protocol to simplify the use of these devices in clinical practice. PAD is also rapidly expanding. These programmes clearly save lives when they are applied appropriately. The main questions that must be answered now are where should these programmes be implemented, who should be trained how to use AEDs, and can AED use be optimised (by reducing “hands free” time)? A hybrid approach of PAD with mobile first responders and static units in selected areas is likely to represent the most efficient use of resources. However, judicious deployment of PAD programmes are likely to become more cost beneficial as the price of devices falls in a competitive marketplace. The ultimate challenge is for improving outcome from sudden cardiac death that occurs in the home.
Supplementary Material
REFERENCES
- 1.Ideker RE, Wolf PD, Tang ASL. Mechanisms of defibrillation. In: Tacker WA, ed. Defibrillation of the heart. St Louis, Missouri: Mosby-Year Book, Inc, 1994:15–45.
- 2.Ideker RE, Chattipakorn N, Gray RA. Defibrillation mechanisms: the parable of the blind men and the elephant. J Cardiovasc Electrophysiol 2000;11:1008–13. Review of the mechanisms of defibrillation. [DOI] [PubMed] [Google Scholar]
- 3.Dillon SM, Kwaku KF. Progressive depolarization. A unified hypothesis for defibrillation and fibrillation induction by shocks. J Cardiovasc Electrophysiol 1998;9:529–52. Thorough examination of theories of defibrillation. [DOI] [PubMed] [Google Scholar]
- 4.ECC Guidelines. Part 6: Advanced cardiovascular life support: section 2: defibrillation. Circulation 2000;102 (suppl I) :I90–4. [PubMed] [Google Scholar]
- 5.Resuscitation Council (UK). Adult advanced life support. Resuscitation Guidelines 2000. http://www.resus.org.uk/pages/als.htm. Current UK Resuscitation Council Guidelines.
- 6.Mittal S, Ayati S, Stein KM, et al. for the ZOLL Investigators Comparison of a novel rectilinear biphasic waveform with a damped sine wave monophasic waveform for transthoracic ventricular defibrillation. J Am Coll Cardiol 1999;34:1595–601. Study demonstrating superiority of rectilinear biphasic waveform over monophasic waveform [DOI] [PubMed] [Google Scholar]
- 7.Schneider T, Martens PR, Paschen H, et al. for the Optimized Response to Cardiac Arrest (ORCA) Investigators. Multicenter, randomized, controlled trial of 150-J biphasic shocks compared with 200- to 360-J monophasic shocks in the resuscitation of out-of-hospital cardiac arrest victims. Circulation 2000;102:1780–7. Study demonstrating superiority of biphasic waveform over monophasic waveform for out-of-hospital cardiac arrest. [DOI] [PubMed] [Google Scholar]
- 8.Van Alem AP, Chapman FW, Lank P, et al. A prospective randomised and blinded comparison of first shock success of monophasic and biphasic waveforms in out-of-hospital cardiac arrest. Resuscitation 2003;58:17–24. Further study demonstrating superiority of biphasic waveform over monophasic waveform for out-of-hospital cardiac arrest. [DOI] [PubMed] [Google Scholar]
- 9.Walker RG, Melnick SB, Chapman FW, et al. Comparison of six clinically used external defibrillators in swine. Resuscitation 2003;57:73–83. [DOI] [PubMed] [Google Scholar]
- 10.Jones JL, Snyder DE, Morgan C. Predictions from misleading pig model are potentially harmful to humans. Resuscitation 2003;59:365–7. [DOI] [PubMed] [Google Scholar]
- 11.Walker RG, Chapman FW, Schmitt PW, et al. Response to Jones et al letter re: Defibrillation wave form comparison from Walker RG, Melnick SB, Chapman FW, Walcott GP, Schmitt PW, Ideker RE, Resuscitation 2003;59:367–71. [Google Scholar]
- 12.Tang W, Weil MH, Sun S, et al. The effects of biphasic waveform design on post-resuscitation myocardial function. J Am Coll Cardiol 2004;43:1228–35. [DOI] [PubMed] [Google Scholar]
- 13.Carpenter J, Rea TD, Murray JA, et al. Defibrillation waveform and post-shock rhythm in out-of-hospital ventricular fibrillation cardiac arrest. Resuscitation 2003;59:189–96. [DOI] [PubMed] [Google Scholar]
- 14.Calle PA, Monsieurs KG, Buylaert WA. Equivalence of the standard monophasic shocks delivered by automated external defibrillators? Resuscitation 2002;53:41–46. [DOI] [PubMed] [Google Scholar]
- 15.Weaver WD, Peberdy MA. Defibrillators in public places—one step closer to home. N Engl J Med 2002;347:1223–4. [DOI] [PubMed] [Google Scholar]
- 16.ECC Guidelines. Part 4: the automated external defibrillator. Circulation 2000;102 (suppl I) :I60. Recent Guidelines 2000 Conference statement on AEDs.10966663 [Google Scholar]
- 17.Priori SG, Bossaert LL, Chamberlain DA, et al. ESC-ERC recommendations for the use of automated external defibrillators (AEDs) in Europe. Eur Heart J 2004;25:437–45. Current European guidelines for AED use. [DOI] [PubMed] [Google Scholar]
- 18.Steen S, Liao Q, Pierre L, et al. The critical importance of minimal delay between chest compressions and subsequent defibrillation: a haemodynamic explanation. Resuscitation 2003;58:249–58. [DOI] [PubMed] [Google Scholar]
- 19.Berg RA, Hilwig RW, Kern KB, et al. Automated external defibrillation versus manual defibrillation for prolonged ventricular fibrillation: lethal delays of chest compressions before and after countershocks. Ann Emerg Med 2003;42:458–67. Study demonstrating deleterious effects of increased hands free time before a shock with AEDs. [DOI] [PubMed] [Google Scholar]
- 20.Chamberlain D, Handley AJ, Colquhoun M. Time for change? Resuscitation 2003;58:237–47. Review of evidence for minimising hands free time before shock delivery. [DOI] [PubMed] [Google Scholar]
- 21.van Alem AP, Sanou BT, Koster RW. Interruption of cardiopulmonary resuscitation with the use of the automated external defibrillator in out-of-hospital cardiac arrest. Ann Emerg Med 2003;42:449–57. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.