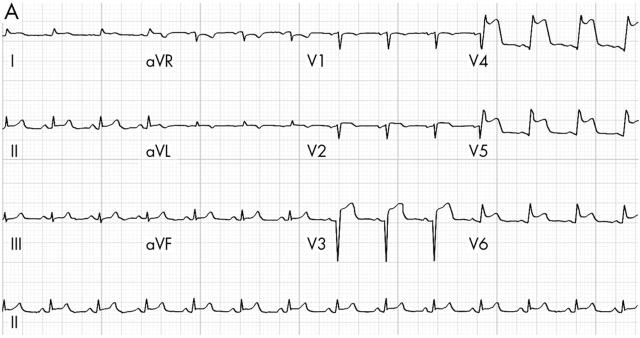
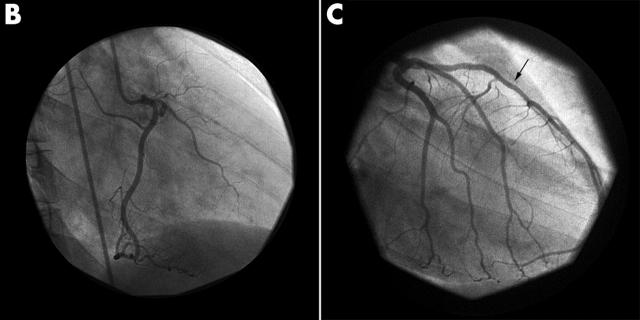
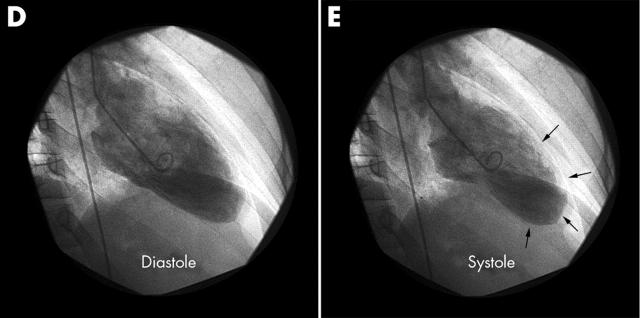
A 40 year old woman developed severe chest discomfort associated with dyspnoea. Her only risk factor was smoking. The ECG showed anterior ST elevation (panel A). Symptoms persisted despite treatment with oxygen, aspirin, intravenous glyceryl trinitrate, metoprolol, and heparin. Emergency cardiac catheterisation revealed normal coronary arteries (panels B and C). The left ventricle (LV) was akinetic/dyskinetic except for the basal segments (panels D and E). Her symptoms and ECG changes resolved gradually. Serial cardiac biomarker elevations were typical of acute myocardial infarction.
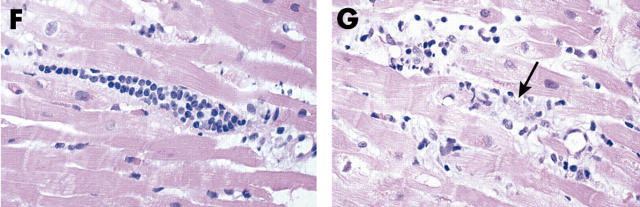
On day 3, an echocardiogram showed a small pericardial effusion. The distal two thirds of the LV was still akinetic/dyskinetic. A right ventricular biopsy showed foci of lymphocytic infiltrate, some in association with myocyte damage (panels F and G). These findings were consistent with the diagnosis of lymphocytic myocarditis.
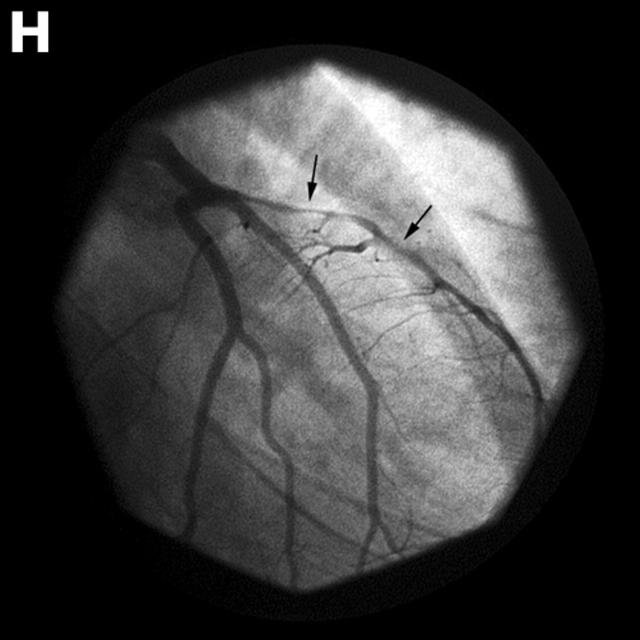
On day 6, the patient was discharged on medical treatment. Ten hours later she developed recurrent symptoms. The ECG showed anterior ST elevation, unresponsive to intravenous glyceryl trinitrate or diltiazem. At repeat cardiac catheterisation there was severe spasm of the left anterior descending (LAD) coronary artery (panel H). Intracoronary vasodilators were administered without success. Balloon dilatation of the LAD was needed to restore flow.
This patient had coronary vasospasm in the setting of lymphocytic myocarditis. Myocarditis occasionally presents as or mimics acute myocardial infarction, but associated coronary spasm has rarely been documented. Caution should be exercised when attributing myocardial infarction to the myocarditis alone, especially if there is ST elevation. Coronary arteriography should be performed early and provocative studies for vasospasm done in the convalescent phase if diagnostic uncertainty persists.