Diabetes is not only a predisposing factor for cardiovascular disease but once diabetic patients develop coronary artery disease (CAD) they have significantly worse outcomes compared to non-diabetic patients.1,2 Diabetes is an independent risk factor for a worse outcome after presentation with acute coronary syndrome (ACS).2
Prior studies have demonstrated that diabetic patients without previous myocardial infarction have as high a risk as non-diabetic patients with previous myocardial infarction.3 Based on this and other studies, diabetes is considered a CAD equivalent or, in other words, patients with diabetes should be treated as already having vascular disease. Elevated cardiac enzymes, both creatine kinase myocardial band (CK-MB) and troponin, have been demonstrated to be important prognostic determinants of patients with ACS and to identify high risk patients.4 The prognostic implications of elevated biomarkers in diabetic patients who are already considered to be at high risk have not been systematically studied.
METHODS
The primary objective was to analyse the prognostic implication of elevated biomarkers in patients with and without diabetes in predicting six month mortality. We studied 1951 consecutive patients who were admitted to the University of Michigan Medical Center from 27 December 1998 to 16 October 2002 with a diagnosis of ACS. The protocol was approved by the institutional review board at the University of Michigan and informed consent obtained from all patients. Diabetes was defined as a known history of type 1 or type 2 diabetes mellitus treated with diet, oral glucose lowering agents, or insulin. Patients utilising insulin for the management of their diabetes before admission were included in the insulin treated diabetic patient subset. Univariate statistics are presented as frequency and percentage for categorical variables, and mean and standard deviation for continuous variables. Probability (p) values for comparisons of the distributions of categorical variables between diabetic and non-diabetic patients were based on χ2 tests; p values for comparisons of continuous variables between diabetic and non-diabetic groups were based on t tests. A multivariable logistic regression analysis was performed for six month mortality in ACS patients adjusted for age, sex, cardiovascular risk factors such as hypertension, hyperlipidaemia, smoking, renal failure, and prior myocardial infarction. All analyses were performed using SAS 8.2 (SAS Institute, Cary, North Carolina, USA).
RESULTS
Of the 1951 patients who were admitted for ACS, 598 (31%) had a previous diagnosis of diabetes mellitus. Age (63.7 (12.3) v 63.3 (14.1) years, p = 0.53) and sex (62.2% v 65.9% male, respectively, p = 0.11) were similar between diabetic and non-diabetic patients. Forty nine per cent of the diabetic patients were identified as insulin treated (type of inpatient and outpatient therapy). Of the 598 patients with diabetes, approximately 71% had elevated biomarkers. Diabetic patients were less likely to present with ST elevation myocardial infarction and more likely to present with non-ST elevation myocardial infarction compared to non-diabetic patients.
Diabetic patients had higher frequencies of hyperlipidaemia, hypertension, obesity, heart failure, and previous myocardial infarction, and were more likely to have a prior diagnosis of renal insufficiency or end stage renal disease. They also had more evidence of non-cardiac vascular disease, including peripheral vascular disease and prior history of stroke or transient ischaemic attack. More diabetic patients had previously undergone percutaneous coronary intervention or coronary artery bypass grafting. Diabetic patients were less likely to be smokers.
The rates of individual in-hospital complications were increased in the diabetic patients versus non-diabetic patients (table 1). Diabetic patients experienced more heart failure, pulmonary oedema, and renal failure while in the hospital. In-hospital mortality was increased by 90% in patients with diabetes (7.3% v 4.0%, p = 0.0017; odds ratio (OR) 1.91, 95% confidence interval (CI) 1.27 to 2.88).
Table 1.
Demographics, management, and clinical outcomes of patients presenting with ACS stratified by diabetes
| Diabetic patient (n = 598) | Non–diabetic patient (n = 1353) | p Value | |
| Demographics | |||
| Mean age (years) | 63.7 (12.3) | 63.3 (14.1) | 0.53 |
| Male | 62.2% | 65.9% | 0.11 |
| Prior myocardial infarction | 50.2% | 37.2% | <0.01 |
| Prior transient ischaemic attack/stroke | 15.5% | 10.1% | <0.01 |
| Hypertension | 81.4% | 61% | <0.01 |
| Hyperlipidaemia | 68.1% | 58.4% | <0.01 |
| Renal insufficiency | 16.2% | 5.3% | <0.01 |
| Hypertension | 81.4% | 61% | <0.01 |
| Peripheral vascular disease | 20.7% | 12.6% | <0.01 |
| Positive biomarkers | 69.2% | 71.1% | 0.38 |
| Ejection Fraction | 46.9% | 49.6% | 0.03 |
| Management | |||
| Percutaneous coronary intervention | 37.1% | 42.7% | 0.01 |
| Coronary artery bypass grafting | 8.4% | 8.1% | 0.86 |
| Intravenous glycoprotein IIb/IIIa | 21.7% | 23.2% | 0.48 |
| Thrombolytics | 5.1% | 7.9% | 0.01 |
| In-hospital events | |||
| Death | 7.3% | 4.0% | <0.01 |
| Reinfarction | 1.6% | 1.1% | 0.38 |
| Stroke | 0.84% | 1.33% | 0.34 |
| Pulmonary oedema | 10.7% | 7.3% | 0.01 |
| Major bleeding | 9.4% | 7.8% | 0.24 |
| Events by 6 months | |||
| Death | 14.2% | 8.4% | <0.01 |
| Reinfarction | 6.0% | 4.9% | 0.42 |
| Stroke | 1.9% | 1.1% | 0.20 |
| Rehospitalisation for ACS | 31.3% | 25.2% | 0.02 |
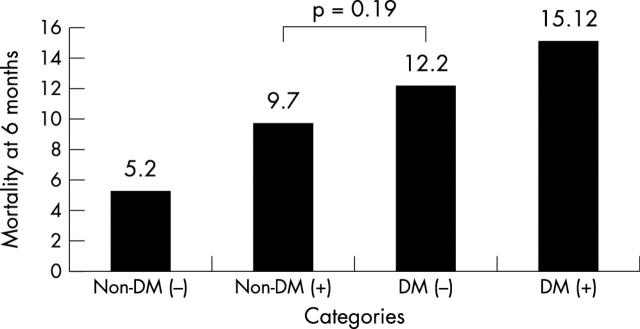
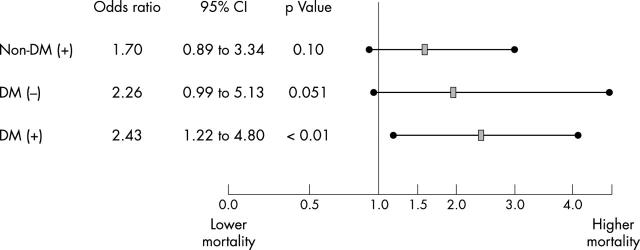
At six months, diabetic patients without elevated cardiac enzymes had a significantly higher mortality compared to non-diabetic patients (12.2% v 5.2%, p = 0.016) and mortality was not different compared to non-diabetic patients with elevated cardiac enzymes (12.2% v 9.7%, p = 0.19) (fig 1). After multivariate adjustment for baseline demographics and co-morbidities, diabetic patients without elevated biomarkers had equivalent risk compared to non-diabetic patients with positive biomarkers (fig 2). Diabetic patients with elevated biomarkers were at the highest risk. The multivariate model demonstrated that diabetic patients on insulin had a trend towards higher mortality compared to diabetic patients treated with diet or an oral hypoglycaemic (OR 1.78; 95% CI 0.98 to 3.26, p = 0.06).
Figure 1.
Cumulative six month mortality in diabetic and non-diabetic patients presenting with ACS stratified by positive cardiac enzymes (CK-MB or troponin). Non-DM (−) = non-diabetic patients without elevated cardiac enzymes; Non-DM (+) = non-diabetic patients with elevated cardiac enzymes; NDM (−) = diabetic patients without elevated cardiac enzymes; DM (+) = diabetic patients with elevated cardiac enzymes.
Figure 2.
Multivariable predictors of six month mortality after ACS in patients stratified by diabetic status and elevated biomarkers. Non-diabetic patients without elevated cardiac enzymes were used as the reference group. Non-DM (+) = non-diabetic patients with elevated cardiac enzymes; DM (−) = diabetic patients without elevated cardiac enzymes; DM (+) = diabetic patients with elevated cardiac enzymes. Diabetic patients without elevated biomarkers had equivalent risk compared to non-diabetic patients who had positive biomarkers. The C index for the model was 0.76; Hosmer-Lemeshow test statistic was 0.44.
DISCUSSION
Previous studies have shown that after an acute myocardial infarction, diabetic patients have worse in-hospital outcomes compared to non-diabetic patients. Several prior studies have demonstrated the unequivocal prognostic implications of elevated cardiac enzymes in patients presenting with ACS.5 An important observation from our study is that the prognosis of diabetic patients presenting with ACS without elevated cardiac enzymes is comparable to non-diabetic patients with elevated cardiac enzymes. Thus diabetic patients who present with ACS but do not have elevated cardiac enzymes (CK-MB or troponin) should probably be treated as aggressively as individuals with elevated biomarkers to try to improve outcomes.
A potential limitation of this study is that determination >of the presence of diabetes mellitus was done by history alone. Thus, the non-diabetic patient group may have included some patients with undiagnosed diabetes or subclinical insulin resistance, the metabolic syndrome that puts patients at higher risk for coronary events.6 If so, the actual adverse event rate difference would be even greater than that found between the two groups of patients in this study.
This study demonstrates that diabetic patients with ACS, without elevated biomarkers, have a mortality risk similar to patients with elevated cardiac enzymes or biomarkers after adjustment for baseline demographics and co-morbidities. Thus diabetic patients presenting with ACS should be treated as aggressively as someone with positive biomarkers, which may in turn potentially translate into improved clinical outcome.
Acknowledgments
This study was supported in part by the Mardigian Foundation Grant.
Abbreviations
ACS, acute coronary syndrome
CAD, coronary artery disease
CK-MB, creatine kinase myocardial band
REFERENCES
- 1.Yudkin JS, Oswald GA. Determinants of hospital admission and case fatality in diabetic-patients with myocardial-infarction. Diabetes Care 1988;11:351–8. [DOI] [PubMed] [Google Scholar]
- 2.Kouvaras G, Cokkinos D, Spyropoulou M. Increased mortality of diabetics after acute myocardial-infarction attributed to diffusely impaired left-ventricular performance as assessed by echocardiography. Jpn Heart J 1988;29:1–9. [DOI] [PubMed] [Google Scholar]
- 3.Haffner SM, Lehto S, Ronnemaa T, et al. Mortality from coronary heart disease in subjects with type 2 diabetes and in non-diabetic subjects with and without prior myocardial infarction. N Engl J Med 1998;339:229–34. [DOI] [PubMed] [Google Scholar]
- 4.James S, Armstrong P, Califf R, et al. Troponin T levels and risk of 30-day outcomes in patients with the acute coronary syndrome: prospective verification in the GUSTO-IV trial. Am J Med 2003;115:178–84. [DOI] [PubMed] [Google Scholar]
- 5.Newby LK, Goldmann BU, Ohman EM. Troponin: an important prognostic marker and risk-stratification tool in non-ST-segment elevation acute coronary syndromes. J Am Coll Cardiol 2003;41:31–6S. [DOI] [PubMed] [Google Scholar]
- 6.Norhammar A, Tenerz A, Nilsson G, et al. Glucose metabolism in patients with acute myocardial infarction and no previous diagnosis of diabetes mellitus: a prospective study. Lancet 2002;359:2140–4. [DOI] [PubMed] [Google Scholar]