Multislice spiral computed tomography (MSCT) coronary angiography is a promising non-invasive technique for the detection of coronary stenoses.1–4 The advent of the technically improved 16 row MSCT scanner, with higher spatial and temporal resolution, has permitted more reliable detection of coronary plaques and significant obstructive coronary lesions.5 It appears likely that MSCT coronary angiography will mature into a non-invasive diagnostic tool that will become integrated into the management of patients with known or suspected coronary atherosclerosis. This review will focus on the basics of the scanner, the diagnostic performance, and potential future applications.
BASICS OF MSCT CORONARY ANGIOGRAPHY
What is computed tomography?
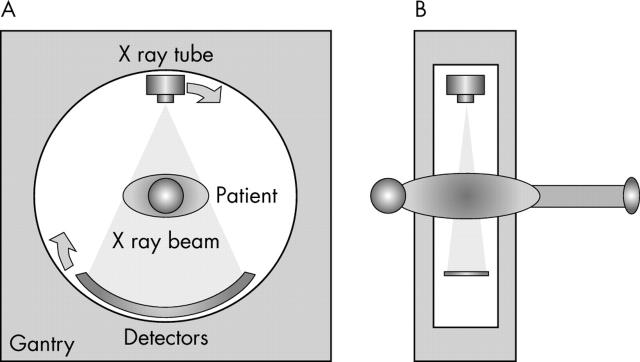
A CT scanner consists of an x ray tube and a row of detectors, which rotate around the patient who is positioned in the centre. The tube produces a fan shaped x ray beam, which passes through the patient and hits the detector on the other side (fig 1). The atomic density of a tissue that an x ray beam encounters determines its attenuation with a higher atomic tissue density resulting in a higher attenuation. The various tissues in a cross section can be distinguished because they have differences in atomic density and attenuation. The attenuation of the x ray beam is expressed as an absolute value measured in Hounsfield units (HU). The rotation of the x ray tube allows calculation of the attenuation at every single point of the slice, which is used to produce a cross sectional image of the body.
Figure 1.
Frontal (A) and side (B) view of a computed tomography (CT) scanner.
The first generation CT scanners used a sequential acquisition pattern, also known as “step-and-shoot”. These scanners produced an axial image while the table remained motionless and for each other slice the table moved to a different position. This sequence of events was repeated throughout the scan range (fig 2A). Sequential CT scanning was both time consuming and extremely sensitive to respiratory movements and was therefore not suitable for cardiac imaging.
Figure 2.
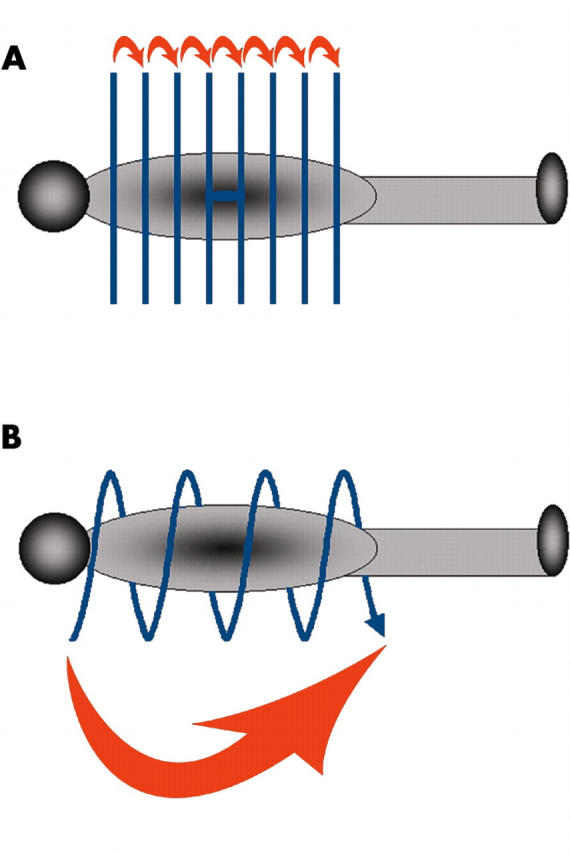
Sequential (A) and spiral (B) CT scanning.
To what do the terms “spiral CT” and “multi-slice spiral CT” refer?
The total scan time was significantly reduced with the introduction of spiral CT scanners. The scan is performed while the patient is continuously moving at a pre-defined speed through the scanner. The resulting trajectory of the x ray tube rotating around the patient can be plotted as a helix or spiral (fig 2B). These scanners acquire volumetric data and cross sectional images can be reconstructed later for any anatomic region. This configuration significantly reduced the total scan time, but still was not fast enough for cardiac scanning.
Multislice spiral CT (MSCT) is a recent development in spiral CT. MSCT scanners are equipped with multiple and thinner detector rows, and have a faster x ray tube rotation speed. These technical advances have an important impact on image quality and will be discussed in detail.
What does the term “retrospective ECG gating” mean?
The contraction of the heart can cause severe motion artefacts on MSCT. To overcome this problem, only data obtained during the diastolic phase of the cardiac cycle (when cardiac motion is reduced) is used for image reconstruction.
The ECG trace of the patient is continuously monitored during the scan procedure, and retrospective ECG gating is used to generate images in the diastolic phase of the cardiac cycle. This retrospective gating technique is based on data acquisition during the whole cardiac cycle. After data acquisition, retrospectively, the optimal reconstruction window is chosen among all available time positions during the diastolic phase to ensure the least cardiac motion artefacts (fig 3). The retrospective gating technique allows flexibility in the position of reconstruction windows to diminish artefacts related to rapid coronary motion and extrasystoles. However, this flexibility is obtained at the cost of a high radiation exposure.
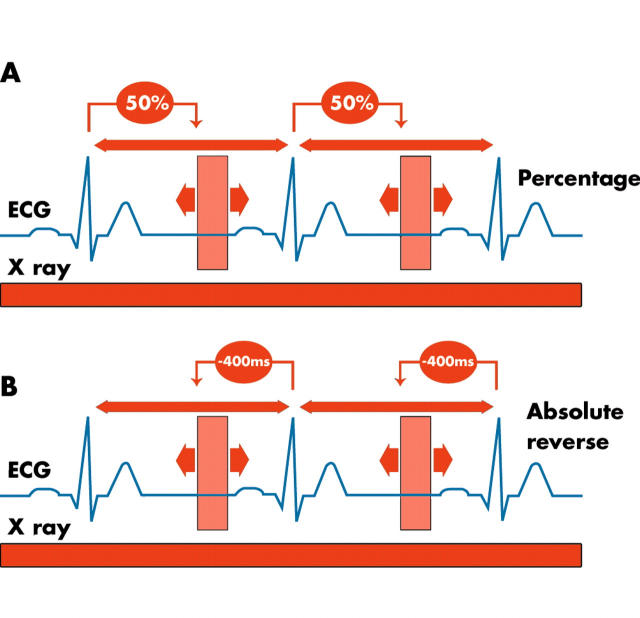
Figure 3.
Scanning during the entire cardiac cycle allows retrospective gating. Different reconstruction windows during the diastolic phase can be explored to obtain images with the least motion artefacts. Two methods can be used to adjust reconstruction windows. One method selects different percentages of the cardiac cycle (A). Another method selects different positions based on an absolute time interval before the next R wave (B). No data are currently available to prove the superiority of either method and both methods are commonly used.
What are the technical requirements for MSCT coronary angiography?
Non-invasive visualisation of the coronary arteries is challenging. High temporal and high spatial resolution are both prerequisites to visualise the small, tortuous, and rapidly moving coronary arteries. Moreover, the scan must be performed within a single breath hold to diminish artefacts related to breathing.
The spatial resolution in the x/y axis of current MSCT scanners is 0.4 × 0.4 mm. The spatial resolution in the z axis is determined by the minimum slice thickness, which varies from 0.5–0.75 mm depending on the manufacturer. These features permit reconstruction of high quality images with a sub-millimetre, nearly isotropic (same size in every dimension) voxel size. This high spatial resolution reduces partial volume effects and also allows visualisation of coronary segments down to diameters of 1.5–2 mm.
A high temporal resolution is needed to minimise artefacts related to coronary motion. The temporal resolution is dependent on the rotation speed of the x ray tube and the detector. Usually a reconstruction algorithm is applied which uses data obtained over half the rotation time of the x ray tube. The temporal resolution using this algorithm currently ranges from 188–250 ms, depending on the manufacturer. In clinical practice, a temporal resolution within this range is sufficient for reliable visualisation of the coronary arteries in patients with a heart rate below 70 beats/min.
Current state-of-the-art MSCT scanners are equipped with 16 detector rows. This feature, combined with the increased rotation speed of the x ray, allows scanning of the heart (generally 11–14 cm in the cranio-caudal axis) in a single breath hold of less than 20 seconds, which is a manageable breath hold for practically all patients.
What are the limitations and pitfalls of MSCT coronary angiography?
MSCT coronary angiography is feasible in patients with a stable heart rhythm, able to breath-hold for 20 seconds. The image quality is degraded by artefacts in patients with irregular heart rhythms; atrial fibrillation is a contraindication for MSCT imaging while frequent extra-systoles can severely degrade image quality, although in the case of occasional extra-systoles this can be overcome by sometimes lengthy manual reconstruction of the images. Breathing during the scan can also severely degrade image quality. Other limitations of CT angiography in general are contraindications to x ray exposure (for example, pregnancy) or to the administration of intravenous iodinated contrast material (for example, allergy, renal failure, or hyperthyroidisms).
Well known pitfalls of MSCT coronary angiography include motion artefacts and severe coronary calcification. The temporal resolution of current 16 row MSCT scanners allows reliable evaluation of the coronary arteries at stable heart rates below 70 beats/min. Oral or intravenous β blockers should be administered to patients with higher resting heart rates to reduce the frequency of motion artefacts. The most rapidly moving coronary segment is the mid part of the right coronary artery where motion artefacts are most frequently observed. Adequate image quality at this level is usually a guarantee of good image quality in the rest of the coronary tree.
Large deposits of calcium in the coronary wall also influence image quality. Coronary calcifications are high density structures causing beam hardening and partial volume artefacts. These artefacts result in over-projection (blooming) of the calcifications on the coronary lumen hampering assessment of coronary lesions (fig 4). Therefore, assessment of both the presence and severity of coronary lesions is compromised in heavily calcified vessels.
Figure 4.
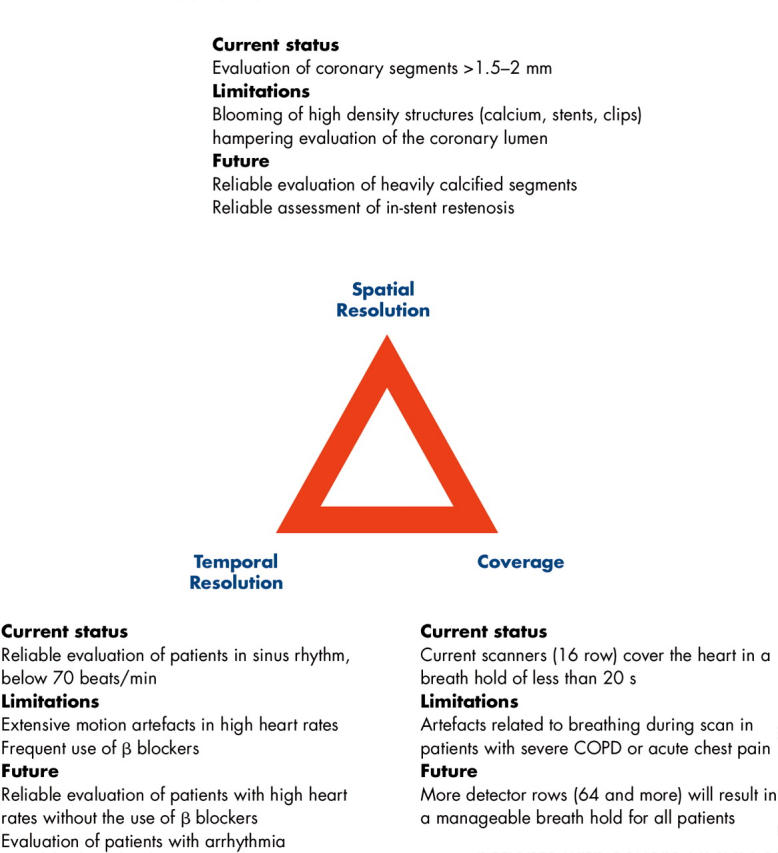
Influence of spatial resolution, temporal resolution, and coverage on the diagnostic performance of MSCT coronary angiography. COPD, chronic obstructive pulmonary disease.
The radiation exposure during MSCT coronary angiography, generally between 7.1–10.9 mSv, remains a source of concern.6–9 Prospective x ray tube modulation can be applied to reduce radiation exposure. This setting reduces radiation output during systole and decreases the calculated effective radiation exposure by up to 50% at low heart rates. The resultant calculated effective radiation exposure (4.3 mSv) is of the same order of magnitude as that of an invasive diagnostic coronary angiogram (2–6 mSv).9
CLINICAL APPLICATIONS
Detection of significant obstructive coronary lesions: historical perspectives
The clinical application of MSCT coronary angiography using the previous generation four row MSCT scanners was limited for several reasons. A significant number of vessels were non-assessable because of the relatively low temporal and spatial resolution. Furthermore, the long scan time (∼40 s) frequently resulted in breathing artefacts during the latter part of the scan.1–4 These limitations resulted in exclusion of up to 32% of the vessels from the analysis because of insufficient image quality (table 1).2
Table 1.
Detection of significant (⩾50%) coronary lesions with MSCT coronary angiography
| n | Excl (%) | Sens (%) | Spec (%) | PPV (%) | NPV (%) | Acc (%) | |
| 4 row MSCT | |||||||
| Nieman et al1 | 31 | 27 | 81 | 97 | 81 | 97 | 95 |
| Achenbach et al2 | 64 | 32 | 85 | 76 | 56 | 94 | 79 |
| Knez et al3 | 44 | 6 | 78 | 98 | 84 | 96 | 94 |
| Vogl et al4 | 38 | 19 | 75 | 99 | 92 | 98 | 98 |
| 16 row MSCT | |||||||
| Nieman et al10 | 58 | 0 | 95 | 86 | 80 | 97 | 97 |
| Ropers et al11 | 77 | 12 | 92 | 93 | 79 | 97 | 93 |
| Mollet et al12 | 128 | 0 | 92 | 95 | 79 | 98 | 95 |
Excl, excluded; Sens, sensitivity; Spec, specificity; PPV, positive predictive value; NPV, negative predictive value; Acc, accuracy.
Detection of significant obstructive coronary lesions: current status
The sensitivity and specificity for detection of significant (⩾ 50% lumen narrowing) lesions with the current generation of 16 row MSCT scanners, when appropriate measures are taken to ensure an appropriate heart rate (use of β blockers for pre-scan heart rates above 60 beats/min), is around 90% (fig 5).10–12 More importantly, the number of non-assessable vessels has been significantly reduced with the 16 row MSCT scanner. Ropers et al excluded only 12% of the vessels and both Nieman et al and Mollet et al did not exclude any vessels for this reason (table 1). This is an important advance because clinical application of this technique presupposes reliable visualisation of the entire coronary tree.
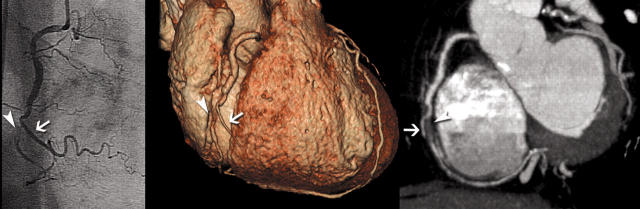
Figure 5.
Conventional angiography image (left panel) showing a subtotal occlusion (arrowhead) of the mid part of the right coronary artery, distal to a right ventricular (RV) branch (arrow). Corresponding CT images using different image post-processing techniques: volume rendered (middle panel) and maximum intensity projection (right panel) images showing the subtotal occlusion (arrowhead) and RV branch (arrow).
Coronary plaque imaging
MSCT coronary calcium score: assessment of the calcium burden
Coronary calcium quantification was first reported with electron beam CT (EBCT) scanners. Histological studies have shown that attenuation values > 130 HU were closely correlated with the presence of calcified plaque.13 Agatston proposed a calcium score to classify calcium deposits in the coronary wall. This score used an area threshold of ⩾ 1 mm2 and a density threshold of > 130 HU to identify a calcified lesion and the Agatston score was calculated by multiplying the area of each calcified lesion with the peak density of the plaque.14 Long term follow up studies have suggested that the Agatston score has incremental prognostic value in the prediction of sudden coronary death or non-fatal myocardial infarction in asymptomatic, high risk patients although this is still somewhat controversial. The presence of calcium is a surrogate for the presence of atherosclerosis and the extent of coronary calcium correlates with the overall atherosclerotic plaque burden. A high calcium score is associated with a higher likelihood of an adverse coronary event, but the presence of calcium in a plaque cannot be considered, at present, as an indicator of plaque vulnerability. Furthermore, a negative calcium score is not a guarantee that the vessel is free from atherosclerotic lesions, including vulnerable plaques, although it renders their presence less likely.15 Coronary calcium is also a function of age and sex, and the predictive accuracy of calcium scoring is improved when adjusted for these parameters.
Several prospective follow up studies have been published to establish the prognostic value of coronary calcium in intermediate to high risk asymptomatic subjects (table 2).16–19 However, the incremental value, over conventional risk factors, of calcium scoring for screening asymptomatic, high risk patients is currently still somewhat controversial because of conflicting data. Large, randomised, prospective follow up studies are needed to establish the real prognostic value of coronary calcium.
Table 2.
Prognostic value of coronary calcium in intermediate and high risk individuals (EBCT studies)
| Study | Subject (n) | Mean age (years) | Follow up (months) | Adverse events* | Cut off value† | Relative risk‡ |
| Detrano et al16 | 1196 | 66 | 41 | 46 | 44 | 2.3 |
| Arad et al17 | 1173 | 53 | 43 | 39 | 160 | 22.2 |
| Raggi et al18 | 676 | 52 | 32 | 30 | >0 | 0.12 v 3.0§ |
| Kondos et al19 | 5635¶ | M:50, F:54 | 37 | 58 | >0 | M:5.8, F:1.8 |
*Adverse events defined as: death and myocardial infarction.
†Cut off value: threshold based on Agatson score, considered as having an increased risk.
‡Relative risk is calculated against the patients with a lower risk score.
§Annual risk.
¶Follow up rate only 64%.
M, male; F, female.
A good correlation between calcium scoring with EBCT and MSCT scanners has been described and currently both techniques are used for calcium scoring.20 Most studies have been performed using EBCT scanners, but nowadays this will gradually be taken over by MSCT scanners, which are widely available.
MSCT coronary angiography: assessment of the total MSCT plaque burden
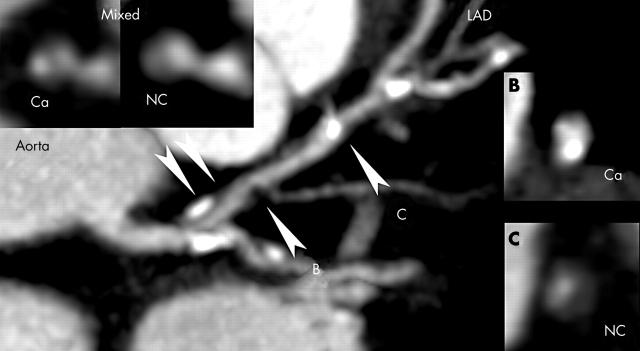
Coronary calcium quantification with EBCT correlates with the extent of atherosclerosis, but severely underestimates the total coronary plaque burden.13 In fact, the amount of calcium detected with EBCT reflects only one fifth of the measured atherosclerotic plaque burden.13 In individual patients, there is wide variation in the extent and severity of coronary plaques. Sixteen row MSCT coronary angiography not only permits reliable detection of significant obstructive lesions, but also detection and classification of coronary plaques into calcified or non-calcified plaques (fig 6).21–23 The total MSCT plaque burden provides additional information about the extent, distribution, and location of coronary atherosclerosis, and might correlate more closely with the total plaque burden found on histology.
Figure 6.
Maximum intensity projected CT image of the left main and left anterior descending coronary artery showing mixed (inlays), calcified (B), and non-calcified (C) plaques. Ca, calcified; LAD, left anterior descending coronary artery; NC, non-calcified.
It has been suggested that the attenuation, in Hounsfield units, of the components of non-calcified plaques could reliably identify the presence of lipid or of fibrous tissue. This might help to identify potentially vulnerable plaques.23–26 More extensive studies are needed to establish the full potential of MSCT coronary angiography in plaque detection and characterisation. An important limitation is the absence of dedicated software able to quantify accurately the amount of calcified as well as non-calcified plaques on a contrast enhanced scan.
Left ventricle function with MSCT coronary angiography
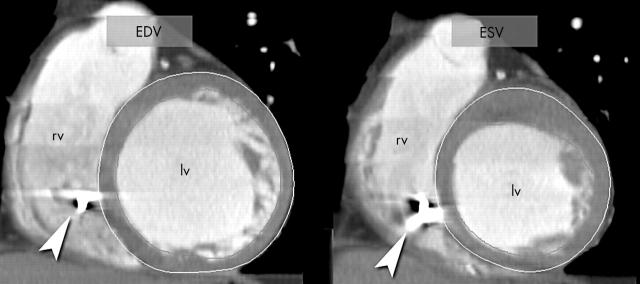
Information of left ventricular function (LVF) can be derived from the scan data obtained during MSCT coronary angiography. Reconstruction of datasets during different phases of the cardiac cycle enables calculation of end diastolic and end systolic volumes of the left ventricle, stroke volume, and ejection fraction (fig 7). A good correlation between ejection fraction measured with MSCT and either magnetic resonance imaging (MRI) or conventional biplane ventriculography has been demonstrated.27,28 MSCT is a less suitable technique for the assessment of wall motion abnormalities because of its lower temporal resolution when compared with MRI or echocardiography. However, the primary aim of MSCT is non-invasive evaluation of the coronary arteries and the provision of functional information is a bonus.
Figure 7.
Reconstruction of datasets at end diastole (left) and end systole (right) allow calculation of ejection fraction and volumes. Reconstruction of additional datasets during the cardiac cycle is required for assessment of wall motion abnormalities. This patient has an impaired ejection fraction due to a previous inferoseptal infarction, which is visualised by reduced thickening of the septal myocardium. MSCT angiography is a potential alternative for patients who cannot undergo MRI—for example, patients with pacemakers (in the present case, a pacemaker lead is visualised in the right ventricle; arrowhead). EDV, end diastolic volume; ESV, end systolic volume; lv, left ventricle; rv, right ventricle.
Non-invasive multislice CT: key points.
Multislice spiral computed tomography (MSCT) coronary angiography is a non-invasive technique that can visualise both the lumen and the wall of the coronary arteries
A low dose non-enhanced MSCT scan can be used for calcium scoring
The latest MSCT scanners allow reliable detection of significant obstructive lesions in native coronary arteries in selected patients
Improvements in MSCT technology are required for reliable evaluation of less selected patient groups
The clinical value of MSCT coronary angiography needs to be established in multi-centre studies, evaluating populations with differing prevalence and presentations of coronary atherosclerosis
Other applications of cardiac MSCT
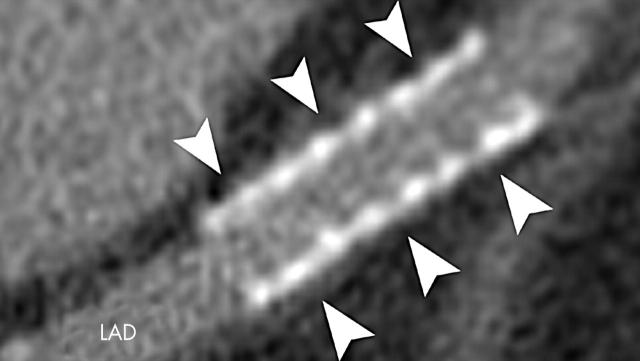
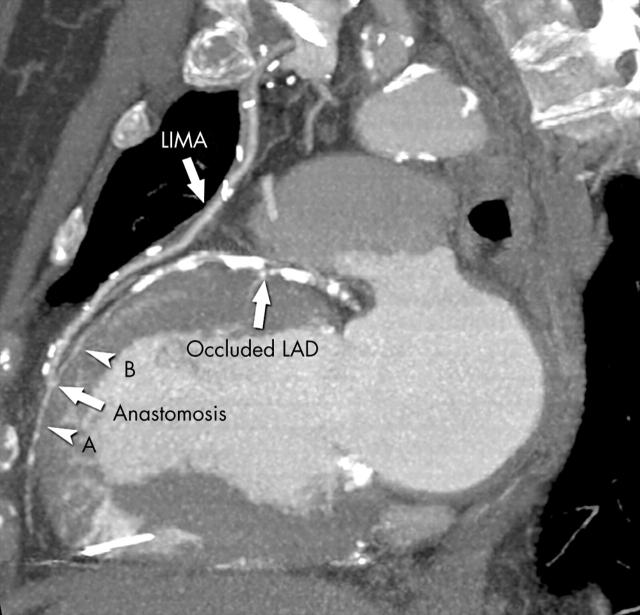
The use of a higher tube current and edge enhancing reconstruction filters allows assessment of stent patency (fig 8). However, beam hardening artefacts related to high density stent materials hamper reliable visualisation of the coronary lumen in stents and do not permit accurate assessment of non-obstructive intima hyperplasia. MSCT angiography is not restricted to native coronary arteries. It provides morphologic information about coronary veins and cardiac chambers, which can be useful for venous mapping or detection of intracardiac thrombi. This technique can also be used to evaluate venous or arterial bypass grafts (fig 9). Preliminary studies, using four row MSCT scanners, showed a high sensitivity and specificity for the detection of occluded venous grafts (97–100% and 98%, respectively).29,30 Diagnostic accuracy for the detection of non-occlusive stenoses in venous grafts and evaluation of arterial grafts was suboptimal; this finding, in conjunction with the fact that a significant percentage of bypass segments (up to 42% of arterial bypasses) were non-assessable limits current clinical application.
Figure 8.
Contrast is well visualised inside the stent allowing assessment of stent patency. This is also shown on the cross sectional image located between the two arrowheads.
Figure 9.
This maximum intensity projection image shows a patent arterial graft (left internal mammary artery, LIMA) inserted on an occluded left anterior descending artery (LAD). The anastomosis is clearly visualised and antegrade filling of the distal part of the LAD (A) as well as retrograde filling of the mid part of the LAD (B) is shown.
FUTURE ROLE OF MSCT CORONARY ANGIOGRAPHY
Current 16 row MSCT scanners allow non-invasive evaluation of both the lumen and wall of the coronary artery. In the near future, MSCT coronary angiography might become an alternative to diagnostic conventional angiography for the detection of significant obstructive lesions. Further studies are needed to determine the role of MSCT coronary angiography in various patient groups such as asymptomatic high risk individuals, asymptomatic patients with known coronary artery disease, or in the evaluation of coronary obstructions in patients with stable angina or acute coronary syndromes.
REFERENCES
- 1.Nieman K, Oudkerk M, Rensing BJ, et al. Coronary angiography with multi-slice computed tomography. Lancet 2001;357:599–603. ▸ First study comparing the results of four row multislice CT coronary angiography with that of conventional angiography for the detection of significant obstructive stenoses. [DOI] [PubMed] [Google Scholar]
- 2.Achenbach S, Giesler T, Ropers D, et al. Detection of coronary artery stenoses by contrast-enhanced, retrospectively electrocardiographically-gated, multislice spiral computed tomography. Circulation 2001;103:2535–8. [DOI] [PubMed] [Google Scholar]
- 3.Knez A, Becker CR, Leber A, et al. Usefulness of multislice spiral computed tomography angiography for determination of coronary artery stenoses. Am J Cardiol 2001;88:1191–4. [DOI] [PubMed] [Google Scholar]
- 4.Vogl TJ, Abolmaali ND, Diebold T, et al. Techniques for the detection of coronary atherosclerosis: multi-detector row CT coronary angiography. Radiology 2002;223:212–20. [DOI] [PubMed] [Google Scholar]
- 5.Flohr TG, Schoepf UJ, Kuettner A, et al. Advances in cardiac imaging with 16-section CT systems. Acad Radiol 2003;10:386–401. [DOI] [PubMed] [Google Scholar]
- 6.Jakobs TF, Becker CR, Ohnesorge B, et al. Multislice helical CT of the heart with retrospective ECG gating: reduction of radiation exposure by ECG-controlled tube current modulation. Eur Radiol 2002;12:1081–6. [DOI] [PubMed] [Google Scholar]
- 7.Hunold P, Vogt FM, Schmermund A, et al. Radiation exposure during cardiac CT: effective doses at multi-detector row CT and electron-beam CT. Radiology 2003;226:145–52. [DOI] [PubMed] [Google Scholar]
- 8.Morin RL, Gerber TC, McCollough CH. Radiation dose in computed tomography of the heart. Circulation 2003;107:917–22. [DOI] [PubMed] [Google Scholar]
- 9.Trabold T, Buchgeister M, Kuttner A, et al. Estimation of radiation exposure in 16-detector row computed tomography of the heart with retrospective ECG-gating. Rofo Fortschr Geb Rontgenstr Neuen Bildgeb Verfahr 2003;175:1051–5. [DOI] [PubMed] [Google Scholar]
- 10.Nieman K, Cademartiri F, Lemos PA, et al. Reliable noninvasive coronary angiography with fast submillimeter multislice spiral computed tomography. Circulation 2002;106:2051–4. ▸ First study comparing the results of 16 row multislice CT coronary angiography with that of conventional angiography for the detection of significant obstructive stenoses. [DOI] [PubMed] [Google Scholar]
- 11.Ropers D, Baum U, Pohle K, et al. Detection of coronary artery stenoses with thin-slice multi-detector row spiral computed tomography and multiplanar reconstruction. Circulation 2003;107:664–6. [DOI] [PubMed] [Google Scholar]
- 12.Mollet NR, Cademartiri F, Nieman K, et al. Multislice spiral CT coronary angiography in patients with stable angina pectoris. J Am Coll Cardiol 2004;43:2265–70. [DOI] [PubMed] [Google Scholar]
- 13.Rumberger JA, Simons DB, Fitzpatrick LA, et al. Coronary artery calcium area by electron-beam computed tomography and coronary atherosclerotic plaque area. A histopathologic correlative study. Circulation 1995;92:2157–62. [DOI] [PubMed] [Google Scholar]
- 14.Agatston AS, Janowitz WR, Hildner FJ, et al. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990;15:827–32. [DOI] [PubMed] [Google Scholar]
- 15.Wexler L, Brundage B, Crouse J, et al. Coronary artery calcification: pathophysiology, epidemiology, imaging methods, and clinical implications. A statement for health professionals from the American Heart Association writing group. Circulation 1996;94:1175–92. [DOI] [PubMed] [Google Scholar]
- 16.Detrano RC, Wong ND, Doherty TM, et al. Coronary calcium does not accurately predict near-term future coronary events in high-risk adults. Circulation 1999;99:2633–8. [DOI] [PubMed] [Google Scholar]
- 17.Arad Y, Spadaro LA, Goodman K, et al. Prediction of coronary events with electron beam computed tomography. J Am Coll Cardiol 2000;36:1253–60. [DOI] [PubMed] [Google Scholar]
- 18.Raggi P, Cooil B, Callister TQ. Use of electron beam tomography data to develop models for prediction of hard coronary events. Am Heart J 2001;141:375–82. [DOI] [PubMed] [Google Scholar]
- 19.Kondos GT, Hoff JA, Sevrukov A, et al. Electron-beam tomography coronary artery calcium and cardiac events: a 37-month follow-up of 5635 initially asymptomatic low- to intermediate-risk adults. Circulation 2003;107:2571–6. [DOI] [PubMed] [Google Scholar]
- 20.Becker CR, Knez A, Jakobs TF, et al. Detection and quantification of coronary artery calcification with electron-beam and conventional CT. Eur Radiol 1999;9:620–4. [DOI] [PubMed] [Google Scholar]
- 21.Schoenhagen P, Tuzcu EM, Stillman AE, et al. Non-invasive assessment of plaque morphology and remodeling in mildly stenotic coronary segments: comparison of 16-slice computed tomography and intravascular ultrasound. Coron Artery Dis 2003;14:459–62. [DOI] [PubMed] [Google Scholar]
- 22.Achenbach S, Moselewski F, Ropers D, et al. Detection of calcified and noncalcified coronary atherosclerotic plaque by contrast-enhanced, submillimeter multidetector spiral computed tomography: a segment-based comparison with intravascular ultrasound. Circulation 2004;109:14–17. ▸ Study comparing the results of 16 row MSCT coronary angiography to detect coronary plaques with that of intracoronary ultrasound. [DOI] [PubMed] [Google Scholar]
- 23.Leber AW, Knez A, Becker A, et al. Accuracy of multidetector spiral computed tomography in identifying and differentiating the composition of coronary atherosclerotic plaques: a comparative study with intracoronary ultrasound. J Am Coll Cardiol 2004;43:1241–7. ▸ Study comparing the results of 16 row MSCT coronary angiography to detect coronary plaques with that of intracoronary ultrasound and correlation with CT density measurements for classification of coronary plaques into soft, fibrous, or calcified plaques. [DOI] [PubMed] [Google Scholar]
- 24.Schroeder S, Kopp AF, Baumbach A, et al. Noninvasive detection and evaluation of atherosclerotic coronary plaques with multislice computed tomography. J Am Coll Cardiol 2001;37:1430–5. ▸ First study demonstrating the potential of MSCT coronary angiography to classify non-calcified plaques into soft or fibrous plaque based on CT density measurements. [DOI] [PubMed] [Google Scholar]
- 25.Becker CR, Nikolaou K, Muders M, et al. Ex vivo coronary atherosclerotic plaque characterization with multi-detector-row CT. Eur Radiol 2003;13:2094–8. [DOI] [PubMed] [Google Scholar]
- 26.Nikolaou K, Becker CR, Muders M, et al. Multidetector-row computed tomography and magnetic resonance imaging of atherosclerotic lesions in human ex vivo coronary arteries. Atherosclerosis 2004;174:243–52. [DOI] [PubMed] [Google Scholar]
- 27.Juergens KU, Grude M, Fallenberg EM, et al. Using ECG-gated multidetector CT to evaluate global left ventricular myocardial function in patients with coronary artery disease. Am J Roentgenol 2002;179:1545–50. [DOI] [PubMed] [Google Scholar]
- 28.Grude M, Juergens KU, Wichter T, et al. Evaluation of global left ventricular myocardial function with electrocardiogram-gated multidetector computed tomography: comparison with magnetic resonance imaging. Invest Radiol 2003;38:653–61. [DOI] [PubMed] [Google Scholar]
- 29.Ropers D, Ulzheimer S, Wenkel E, et al. Investigation of aortocoronary artery bypass grafts by multislice spiral computed tomography with electrocardiographic-gated image reconstruction. Am J Cardiol 2001;88:792–5. [DOI] [PubMed] [Google Scholar]
- 30.Nieman K, Pattynama PM, Rensing BJ, et al. Evaluation of patients after coronary artery bypass surgery: CT angiographic assessment of grafts and coronary arteries. Radiology 2003;229:749–56. [DOI] [PubMed] [Google Scholar]