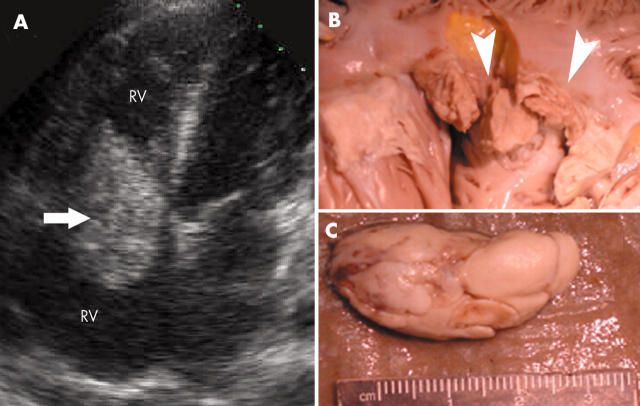
A 19 year old, previously healthy, woman was admitted with complaints of generalised fatigue, chills, and signs of septic shock. There was no history of alcohol or intravenous drug abuse. A chest computed tomographic scan visualised two areas of infarction in the right lung. These findings prompted an echocardiographic examination, which demonstrated a large (6 × 3 cm), lobulated, mobile mass, partially obstructing the tricuspid valve, and prolapsing into the right ventricle. (panel A, arrow).
The diagnosis of tricuspid valve endocarditis was confirmed when Streptococcus agalactiae grew in three out of four admission peripheral blood samples. Because of disseminated intravascular coagulation with persistent, severe, thrombocytopenia (< 10000 platelets/mm3), urgent tricuspid valve surgery was not possible. On the third hospital day, the patient showed signs of decreased oxygenation, requiring ventilatory support, and followed by cardiopulmonary arrest. Despite all resuscitative efforts, including initiation of cardiopulmonary bypass, the patient died.
A post-mortem examination revealed complete obstruction of the right pulmonary artery by a 3 × 2 cm mass, representing a fragment of bacterial vegetation (panel C). The tricuspid valve was eroded with an associated myocardial abscess (panel B, arrowheads). On microscopic examination, the tricuspid valve surface was coated with numerous Gram-positive cocci.
S agalactiae is an uncommon cause of native tricuspid valve endocarditis in the absence of predisposing conditions such as intravenous drug abuse, diabetes mellitus, alcoholism, or pregnancy. The bacteria lack fibrinolysin production, which might explain the unusual large, friable vegetations, and the high rate of embolisation.
Figure 1.
(A) Apical four chamber view with large vegetation of the tricuspid valve (arrow). (B) Tricuspid valve, which is eroded, with an associated myocardial abscess (arrowheads). (C) Embolus (bacterial vegetation) recovered from the right pulmonary artery.