Abstract
Objective: To assess whether the extent of primary and secondary coronary heart disease (CHD) prevention in older British men and women differs between patients with and without diabetes.
Design: Two prospective cardiovascular cohort studies.
Setting: 24 British towns.
Patients: 4252 men and 4286 women aged 60–79 years examined between 1998 and 2001.
Main outcome measures: Use of aspirin, statin, and blood pressure lowering treatment and risk factor control, examined by diabetic status and history of established CHD.
Results: About 20% of the men and 12% of the women had established CHD at age 60–79 years and 7% of the men and 5% of the women had diabetes. In primary CHD prevention, patients with diabetes were more likely to receive CHD risk reducing medications than those without diabetes, but the proportions receiving preventive treatments in both groups were low. In secondary prevention, diabetic and non-diabetic patients received similar levels of treatment, with the exception of angiotensin converting enzyme inhibitors and (for women only) blood pressure lowering treatment, which were more widely used among diabetic patients. There were no clear differences in blood pressure control or cigarette smoking by diabetic status in primary or secondary prevention. Mean total cholesterol concentrations were lower in diabetic patients independently of treatment with statins.
Conclusions: Despite their exceptionally high CHD risk, many opportunities to reduce CHD risk among patients with diabetes have not been taken.
Keywords: diabetes, coronary heart disease, primary prevention, secondary prevention
Diabetes is associated with a greatly increased risk of further cardiovascular events and death, in both patients with and patients without established coronary heart disease (CHD).1,2 Cardiovascular risks among patients with diabetes and CHD are exceptionally high.1 Several randomised controlled trials and meta-analyses have confirmed that the benefits of aspirin,3 statins,4–7 and angiotensin converting enzyme (ACE) inhibitors8 extend to patients with diabetes, and the benefits of blood pressure lowering treatments in the primary prevention of CHD in patients with diabetes have been clearly shown.9,10 The potential benefits of both primary and especially secondary CHD prevention in patients with diabetes are therefore substantial. In recognition of this, both British and European guidelines on cardiovascular disease prevention have for several years recommended that patients with non-insulin dependent diabetes (or insulin dependent diabetes with microalbuminuria) should be identified as a priority group for cardiovascular preventive treatments.11–13
In this study, we set out to examine the extent to which opportunities for CHD prevention have been taken in patients aged 60–79 with diabetes. Specifically, we compared the extent of CHD prevention received by diabetic and non-diabetic patients examined separately according to whether they had established CHD (secondary prevention) or not (primary prevention) in two parallel population based studies of cardiovascular health among older men and women examined between 1998 and 2001.
METHODS
Description of the cohort studies
The British regional heart study (BRHS) is a prospective study of cardiovascular disease in men in one general practice in each of 24 British towns, representing all major British regions.14 Participants aged 40–59 years were enrolled in 1978–80 and have been followed up for cardiovascular mortality through the National Health Service central registers and for cardiovascular morbidity through regular biennial reviews of general practice records. Fewer than 1% have been lost to follow up.15 Between February 1998 and February 2000, 4252 men (76% of all surviving men) attended for a 20 year follow up examination where they were physically examined and completed a detailed nurse administered questionnaire providing information on current medications, history of diabetes, and cigarette smoking habits. The British women’s heart and health study (BWHHS) cohort was established between 1999 and 2001 to parallel the BRHS.16 In total 4286 women aged 60–79 years attended for a physical examination and completed a similar questionnaire to the men’s 20 year follow up questionnaire. Participants’ general practice medical records (including general practitioner notes and hospital correspondence) were reviewed in detail to identify diagnoses of diabetes and all diagnoses of angina and myocardial infarction occurring since 1978, as well as all occurrences of coronary artery bypass grafting (CABG) and percutaneous transluminal coronary angioplasty (PTCA). For both men and women, a diagnosis of myocardial infarction was confirmed according to established World Health Organization criteria (any report of myocardial infarction accompanied by at least two of the following: history of severe chest pain, ECG evidence of myocardial infarction, and enzyme changes associated with myocardial infarction). Ethical approval was obtained from all relevant local research ethics committees for both studies.
Physical examination
In the 20 year rescreening of men in the BRHS and the baseline screening of women in the BWHHS, patients had standardised measurements of weight and height; body mass index was calculated as weight in kilograms divided by the square of the height in metres (kg/m2). Seated blood pressure was measured twice in succession in the right arm with a Dinamap 1846SX vital signs monitor; the average of the two measurements were used in analyses. These estimates were corrected for overreading by the instrument for systolic blood pressure17 and were adjusted for observer variation within each town.18 Blood samples were taken after a minimum six hour fast from all participants except those taking oral hypoglycaemic drugs or insulin, who provided non-fasting samples. These were stored frozen at −20°C until analysed for serum total cholesterol with a Hitachi 747 automated analyser. Current smoking status was ascertained by questionnaire. All participants were asked to list all current medications (including aspirin, with or without prescription); this information was checked directly against medication containers or prescription cards. All medications were coded according to the British National Formulary classification (http://www.bnf.org/).
Evidence of CHD and diabetes
Established CHD was defined as a general practice record of definite myocardial infarction (diagnosed in accordance with World Health Organization criteria), any report of angina, or any revascularisation procedure (PTCA or CABG). Patients were classified as having diabetes on the basis of a general practice record of diabetes or recall of a doctor’s diagnosis of diabetes.
Statistical methods
Logistic regression was used to estimate age adjusted odds ratios for treatment use (and risk factor control) for diabetic relative to non-diabetic patients. Differences in the distributions of total cholesterol and systolic blood pressure between patients with and those without diabetes were assessed by the Kolmogorov-Smirnov test, which tests whether two independent sets of data plausibly have the same underlying distribution.
RESULTS
Study participants
Of the 4252 men who attended for examination in the BRHS, 854 (20%) had evidence of CHD (definite myocardial infarction, any report of angina, or a revascularisation procedure (PTCA or CABG)) and 316 (7%) had diabetes (recall or general practice record). For the 4286 women who attended the baseline examination of the BWHHS, these figures were 525 (12%) and 216 (5%), respectively. Among both men and women, diabetes was more common among patients who also had a history of CHD; for men, 10% of those with CHD had diabetes compared with 7% of those without CHD, and for women, 9% of those with CHD had diabetes compared with 4% of those without (table 1). Table 1 shows the level of medication use and risk factor control in both primary and secondary prevention among both patients with and patients without diabetes.
Table 1.
Prevalence of treatment use and risk factor control among 4252 men and 4286 women aged 60–79 in the British regional heart study and British women’s heart and health study, 1998–2001
| Primary prevention | Secondary prevention | |||||||
| Diabetic | Non-diabetic | OR | 95% CI | Diabetic | Non-diabetic | OR | 95% CI | |
| Men | ||||||||
| Number of patients | 232 | 3166 | 84 | 770 | ||||
| Aspirin | 22.8% | 15.9% | 1.54 | 1.12 to 2.13 | 72.6% | 71.1% | 1.08 | 0.65 to 1.79 |
| Statins | 6.0% | 2.1% | 3.10 | 1.71 to 5.62 | 25.0% | 24.3% | 1.06 | 0.63 to 1.81 |
| β Blockers | 13.8% | 8.8% | 1.63 | 1.10 to 2.42 | 29.8% | 31.4% | 0.93 | 0.57 to 1.53 |
| ACE inhibitors | 25.0% | 5.9% | 5.28 | 3.78 to 7.36 | 34.5% | 19.7% | 2.14 | 1.32 to 3.47 |
| Any BP lowering drugs | 43.5% | 20.6% | 2.96 | 2.24 to 3.89 | 60.7% | 56.0% | 1.22 | 0.77 to 1.93 |
| Aspirin and statins | 3.4% | 1.0% | 3.62 | 1.65 to 7.96 | 20.2% | 21.2% | 0.96 | 0.55 to 1.70 |
| Cigarette smoking | 9.5% | 13.4% | 0.69 | 0.44 to 1.08 | 9.6% | 11.5% | 0.83 | 0.39 to 1.78 |
| BMI ⩾30 kg/m2 | 32.3% | 14.6% | 2.83 | 2.09 to 3.83 | 32.5% | 21.3% | 1.81 | 1.09 to 2.99 |
| SBP <130 mm Hg | 14.7% | 20.5% | 0.68 | 0.47 to 1.00 | 22.9% | 29.4% | 0.72 | 0.42 to 1.23 |
| DBP <80 mm Hg | 37.7% | 30.0% | 1.40 | 1.06 to 1.85 | 56.6% | 45.3% | 1.57 | 1.00 to 2.49 |
| TC <5 mmol/l | 21.9% | 13.7% | 1.74 | 1.24 to 2.44 | 34.7% | 21.9% | 1.91 | 1.15 to 3.17 |
| Women | ||||||||
| Number of patients | 167 | 3594 | 49 | 476 | ||||
| Aspirin | 22.7% | 9.0% | 2.96 | 1.98 to 4.43 | 43.2% | 46.4% | 0.88 | 0.47 to 1.65 |
| Statins | 23.4% | 3.9% | 7.62 | 5.04 to 11.51 | 25.0% | 27.2% | 0.93 | 0.45 to 1.91 |
| β Blockers | 25.3% | 11.6% | 2.57 | 1.76 to 3.75 | 20.5% | 32.0% | 0.55 | 0.26 to 1.19 |
| ACE inhibitors | 27.5% | 6.5% | 5.57 | 3.86 to 8.04 | 34.7% | 18.5% | 2.32 | 1.23 to 4.37 |
| Any BP lowering drugs | 57.1% | 26.1% | 3.77 | 2.71 to 5.25 | 65.9% | 48.4% | 2.05 | 1.07 to 3.93 |
| Aspirin and statins | 9.7% | 1.2% | 8.77 | 4.72 to 16.29 | 13.6% | 19.4% | 0.67 | 0.27 to 1.64 |
| Cigarette smoking | 12.1% | 11.6% | 1.06 | 0.65 to 1.71 | 6.1% | 11.8% | 0.50 | 0.15 to 1.66 |
| BMI ⩾30 kg/m2 | 55.2% | 24.4% | 3.88 | 2.79 to 5.39 | 53.7% | 30.3% | 2.74 | 1.43 to 5.25 |
| SBP <130 mm Hg | 15.1% | 24.3% | 0.57 | 0.36 to 0.90 | 21.4% | 31.6% | 0.61 | 0.28 to 1.32 |
| DBP <80 mm Hg | 46.1% | 50.4% | 0.85 | 0.61 to 1.19 | 54.8% | 58.9% | 0.86 | 0.45 to 1.63 |
| TC <5 mmol/l | 16.3% | 4.8% | 3.88 | 2.43 to 6.18 | 17.5% | 12.3% | 1.58 | 0.66 to 3.80 |
ACE, angiotensin converting enzyme; BMI, body mass index; BP, blood pressure; CI, confidence interval; DBP, diastolic blood pressure; OR, age adjusted odds ratio (diabetic relative to non-diabetic); SBP, systolic blood pressure; TC, total cholesterol.
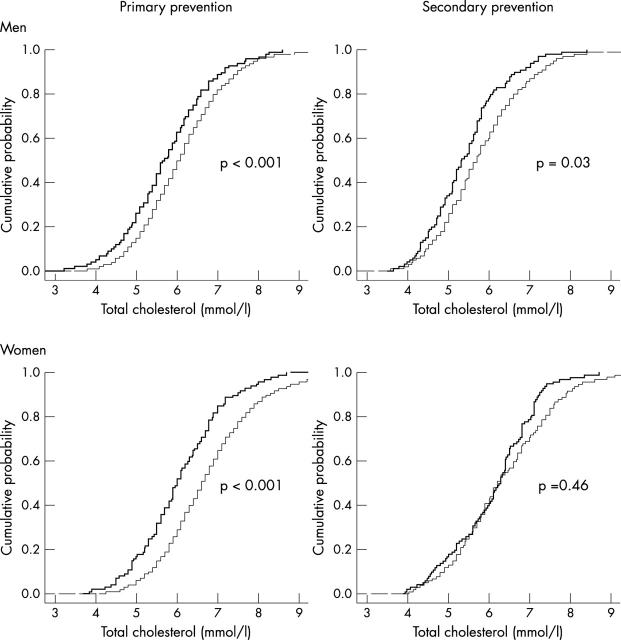
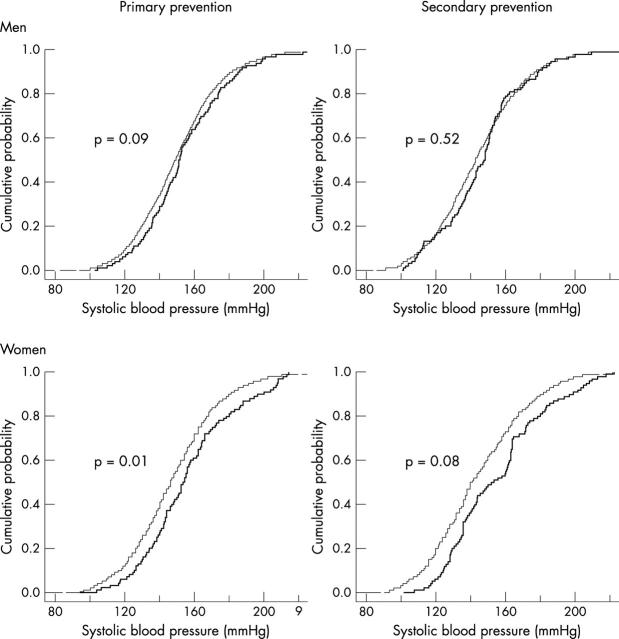
Primary prevention
Among patients without previous CHD, the likelihood of receiving aspirin, statins, β blockers, ACE inhibitors, and any blood pressure lowering drug was much greater among diabetic than among non-diabetic patients (table 1). However, even among diabetic patients, only small proportions were receiving either single or combined medications. For example, only about one in 17 men and one in 10 women with diabetes were receiving both aspirin and a statin. Figure 1 shows the distribution of total cholesterol and fig 2 the distribution of systolic blood pressure for patients with and without diabetes; table 1 shows the proportions achieving particular cut off values. Both men and women with diabetes had lower serum total cholesterol concentration than patients without diabetes, and a higher proportion of them had a total cholesterol concentration less than 5 mmol/l (odds ratio for low total cholesterol for diabetic relative to non-diabetic patients was 1.74 in men and 3.88 in women). However, this difference in mean cholesterol concentration could not be attributed to treatment with statins, being just as notable in patients who were not receiving statins. Systolic blood pressures tended to be higher among diabetic than among non-diabetic patients. However, men with diabetes were marginally more likely to have low diastolic pressure (< 80 mm Hg) than men without diabetes (table 1). Both men and women with diabetes were more likely to be obese (body mass index ⩾ 30 kg/m2) than those without diabetes (odds ratio 2.83 for men and 3.88 for women). No significant differences in cigarette smoking rates were observed between patients with and patients without diabetes.
Figure 1.
Empirical distributions of serum total cholesterol. In each panel, the thick line corresponds to patients with diabetes and the thin line to patients without diabetes.
Figure 2.
Empirical distributions of systolic blood pressure. In each panel, the thick line corresponds to patients with diabetes and the thin line to patients without diabetes.
Secondary prevention
Rates of preventive drug use were higher among patients with established CHD than in the primary prevention group, among both men and women. However, rates were still generally low among both diabetic and non-diabetic patients; patients with diabetes were no more likely than patients without diabetes to receive aspirin, statins, or β blockers. The prevalence of use of ACE inhibitors and (for women only) any blood pressure lowering drug was higher among those with diabetes (odds ratios for use of ACE inhibitors for diabetic relative to non-diabetic patients was 2.14 in men and 2.32 in women). As with primary prevention, a higher proportion of patients with diabetes had total cholesterol concentrations below 5 mmol/l (fig 1). This difference was also independent of treatment with statins. Blood pressure control was similar among patients with and without diabetes (fig 2). As observed in the primary prevention group, diabetic patients were more likely to be obese and there were no significant differences in cigarette smoking rates between patients with and patients without diabetes.
Further analyses
Repeat analyses were restricted to 2501 men and 2313 women who were younger than 70 years at their date of examination. Overall, rates of drug use and risk factor control among these younger patients were similar to those for all patients, except in the case of statins, where about one third of the men and women with diagnosed CHD received these drugs (compared with one quarter of all patients). However, for both men and women, differences in drug use and risk factor control between diabetic and non-diabetic patients were largely unaffected by exclusion of patients aged 70 or over. Trends in drug use for all patients with established CHD were also examined over the study period. Among men with established CHD, use of aspirin and, particularly, statins was more probable in 1999–2000 than in 1998 (74% v 67% for aspirin and 28% v 19% for statins, respectively). Similarly, women with CHD who were examined in 2000–01 tended to be more likely to receive these drugs than women examined in 1999 (aspirin use was 52% in 2000–01 compared with 33% in 1999, and statin use was 30% and 21%, respectively, in these years). Women with CHD were also more likely to receive ACE inhibitors in 2000-01 than in 1999. However, for both men and women, adjustment for trends in drug use did not influence the comparative differences observed between patients with and patients without diabetes.
DISCUSSION
At the time of this study, few patients with diabetes appeared to be receiving optimal CHD prevention, despite their exceptionally high risk of CHD. In the secondary prevention context, diabetic patients were more likely to be receiving ACE inhibitors and blood pressure lowering medication, though there was no notable improvement in blood pressure control. The frequency of use of aspirin, β blockers, and statins was similar for diabetic and non-diabetic patients. In the primary prevention context, the prevalences of preventive medication use by diabetic patients, though higher than the prevalences among non-diabetic patients, were still low. These low rates of preventive treatment were present despite the clear evidence of strong benefits of aggressive risk reduction among diabetic patients, which was incorporated in recommendations and guidelines published from the late 1990s.11–13 At the time of these observations, evidence regarding the effectiveness of statins was largely based on patients aged 75 years or younger and, while it has since been shown that these benefits do extend to patients aged over 75,19 this may have influenced prescription rates among our older patients. We have previously shown that among men with diagnosed CHD, those who were younger at the date of their event were more likely to receive statins than those who were older (after adjustment for the year that the event occurred).20 However, even among patients younger than 70, the overall prevalence of statin use in secondary prevention was low (about one third of both men and women). Furthermore, the similarities in drug use between diabetic and non-diabetic patients were the same in all age groups.
The improvement of CHD prevention in patients with diabetes is an important priority. In the secondary prevention context, it appears that the extent of clinical prevention provided to diabetic patients is similar to that provided to non-diabetic patients. This suggests that the limiting factor for secondary prevention among patients with diabetes is the overall standard of prevention provided to patients with established CHD. Taking steps to increase overall coverage of secondary prevention—emphasising the major independent reductions in risk of recurrent vascular disease that can be obtained from antiplatelet drugs, statins, β blockers, and ACE inhibitors21 or closely related combination treatments22—is likely to be the most direct way to improve secondary prevention in diabetic patients.
Opportunities for the primary prevention of CHD in patients with diabetes occur in the context of routine diabetes care. However, concern has been expressed about the quality of guidelines available for the management of patients with diabetes and the need to focus management more strongly on cardiovascular disease prevention.23 More systematic evidence based approaches to the management of patients with diabetes may help to ensure that opportunities for primary prevention of CHD in this high risk group are realised (http://www.doh.gov.uk/nsf/diabetes).24
Acknowledgments
The British regional heart study (established by Professor A G Shaper) is a British Heart Foundation (BHF) Research Group and receives additional support from the Department of Health (England). The British women’s heart and health study is funded by the Department of Health (England). JRE is supported by a BHF Junior Research Fellowship. DAL is funded by a Department of Health (England) Career Scientist Award. The views expressed in this publication are those of the authors and not necessarily those of the funding agencies.
Abbreviations
ACE, angiotensin converting enzyme
BRHS, British regional heart study
BWHHS, British women’s heart and health study
CABG, coronary artery bypass grafting
CHD, coronary heart disease, PTCA, percutaneous transluminal coronary angioplasty
REFERENCES
- 1.Haffner SM, Lehto S, Ronnemaa T, et al. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med 1998;339:229–34. [DOI] [PubMed] [Google Scholar]
- 2.Mukamal KJ, Nesto RW, Cohen MC, et al. Impact of diabetes on long-term survival after acute myocardial infarction: comparability of risk with prior myocardial infarction. Diabetes Care 2001;24:1422–7. [DOI] [PubMed] [Google Scholar]
- 3.Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. Antithrombotic trialists’ collaboration. BMJ 2002;324:71–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Collins R, Armitage J, Parish S, Heart Protection Study Collaborative Group, et al. MRC/BHF heart protection study of cholesterol-lowering with simvastatin in 5963 people with diabetes: a randomised placebo-controlled trial. Lancet 2003;361:2005–16.12814710 [Google Scholar]
- 5.Pyorala K, Pedersen TR, Kjekshus J, et al. Cholesterol lowering with simvastatin improves prognosis of diabetic patients with coronary heart disease: a subgroup analysis of the Scandinavian simvastatin survival study (4S). Diabetes Care 1997;20:614–20. [DOI] [PubMed] [Google Scholar]
- 6.Sacks FM, Pfeffer MA, Moye LA, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and recurrent events trial investigators. N Engl J Med 1996;335:1001–9. [DOI] [PubMed] [Google Scholar]
- 7.Keech A, Colquhoun D, Best J, et al. Secondary prevention of cardiovascular events with long-term pravastatin in patients with diabetes or impaired fasting glucose: results from the LIPID trial. Diabetes Care 2003;26:2713–21. [DOI] [PubMed] [Google Scholar]
- 8.HOPE Investigators. Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy. Heart outcomes prevention evaluation study investigators. Lancet 2000;355:253–9. [PubMed] [Google Scholar]
- 9.UK Prospective Diabetes Study Group. Efficacy of atenolol and captopril in reducing risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 39. UK prospective diabetes study group. BMJ 1998;317:713–20. [PMC free article] [PubMed] [Google Scholar]
- 10.UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK prospective diabetes study group. BMJ 1998;317:703–13. [PMC free article] [PubMed] [Google Scholar]
- 11.British Cardiac Society, British Hyperlipidaemia Association, British Hypertension Society. Joint British recommendations on prevention of coronary heart disease in clinical practice. British Cardiac Society, British Hyperlipidaemia Association, British Hypertension Society, endorsed by the British Diabetic Association. Heart 1998;80 (suppl 2) :1–29. [PMC free article] [PubMed] [Google Scholar]
- 12.De Backer G, Ambrosioni E, Borch-Johnsen K, et al. European guidelines on cardiovascular disease prevention in clinical practice: third joint task force of European and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of eight societies and by invited experts). Eur Heart J 2003;24:1601–10. [DOI] [PubMed] [Google Scholar]
- 13.Wood D, De Backer G, Faergeman O, et al. Prevention of coronary heart disease in clinical practice: recommendations of the second joint task force of European and other societies on coronary prevention. Atherosclerosis 1998;140:199–270. [DOI] [PubMed] [Google Scholar]
- 14.Shaper AG, Pocock SJ, Walker M, et al. British regional heart study: cardiovascular risk factors in middle-aged men in 24 towns. BMJ 1981;283:179–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walker M, Shaper AG, Lennon L, et al. Twenty year follow-up of a cohort based in general practices in 24 British towns. J Public Health Med 2000;22:479–85. [DOI] [PubMed] [Google Scholar]
- 16.Lawlor DA, Bedford C, Taylor M, et al. Geographical variation in cardiovascular disease, risk factors, and their control in older women: British women’s heart and health study. J Epidemiol Community Health 2003;57:134–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Whincup PH, Bruce NG, Cook DG, et al. The Dinamap 1846SX automated blood pressure recorder: comparison with the Hawksley random zero sphygmomanometer under field conditions. J Epidemiol Community Health 1992;46:164–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bruce NG, Shaper AG, Walker M, et al. Observer bias in blood pressure studies. J Hypertens 1988;6:375–80. [PubMed] [Google Scholar]
- 19.Heart Protection Study Collaborative Group. MRC/BHF heart protection study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet 2002;360:7–22.12114036 [Google Scholar]
- 20.Whincup PH, Emberson JR, Lennon L, et al. Low prevalence of lipid lowering drug use in older men with established coronary heart disease. Heart 2002;88:25–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yusuf S . Two decades of progress in preventing vascular disease. Lancet 2002;360:2–3. [DOI] [PubMed] [Google Scholar]
- 22.Wald NJ, Law MR. A strategy to reduce cardiovascular disease by more than 80%. BMJ 2003;326:1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shaughnessy AF, Slawson DC. What happened to the valid POEMs? A survey of review articles on the treatment of type 2 diabetes. BMJ 2003;327:266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Department of Health. National service framework for diabetes: modern standards and service models. London: Department of Health, 2001.