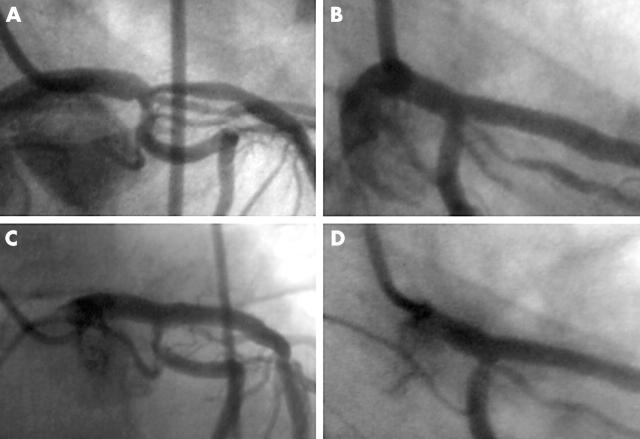
A 35 year old man underwent elective angioplasty for a severe stenosis at the ostium of the left anterior descending artery (LAD) involving the distal left main stem (LMS) (panel A). Abciximab was administered and a 3.5 × 24 mm Taxus stent (Boston Scientific, USA) was deployed in the proximal LAD extending into the distal LMS, bridging the circumflex ostium. Flow was now compromised in the circumflex and a second stent (2.5 × 16 mm Taxus) was deployed at the circumflex ostium in a “T” configuration. Further dilatations were performed to both stents and a good final angiographic result was obtained (panel B).
Against medical advice the patient stopped clopidogrel at 10 days. Thirty days post-angioplasty he presented to the emergency room at a referring hospital with acute chest pain. ECG showed anterior ST depression and lateral ST elevation. The patient was thrombolysed with tenecteplase and transferred for urgent coronary angiography. The LAD/LMS stent was widely patent, however, the circumflex stent contained thrombus (panel C) with TIMI 3 flow in the circumflex. As he was pain-free and stable a decision was made to attempt medical treatment. Tirofiban was administered for 48 hours. Angiography at 48 hours showed the thrombus in the circumflex had resolved (panel D). His ECG returned to normal and he suffered no further chest pain.
Stent thrombosis is believed to have occurred because of premature discontinuation of clopidogrel and was successfully managed medically with a combination of thrombolysis and glycoprotein IIb/IIIa inhibition. At four months follow up the patient was free of angina.