A 60 year old male presented with complaints of cough, dyspnoea, reduced appetite, and a history of 70 pound (30 kg) weight loss over the previous year.
Chest radiograph showed complete opacification of the left hemithorax with only minimal aeration of the most cephaloid lung apex.
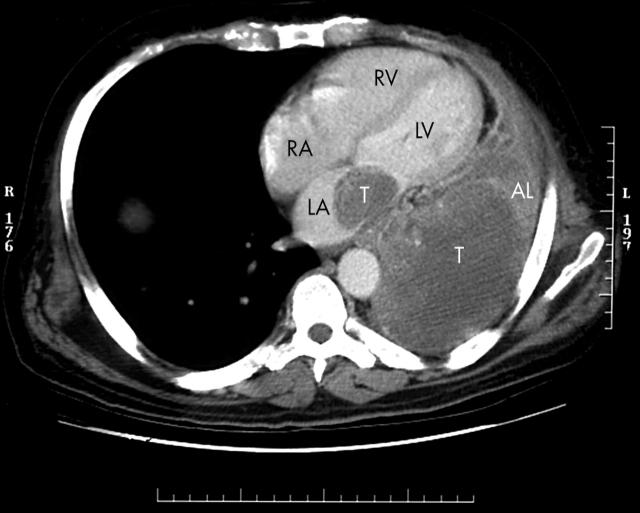
A computed tomographic (CT) scan (below left) of the chest showed a 10 cm mass in the posterior left lower lobe with invasion into the left atrium by way of the left inferior pulmonary vein. There was left basilar lung atelactasis with a small left pleural effusion. The panel shows the lung mass and tumour extension into the left atrium (AL, atelactatic lung; LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle, T, tumour).
A bronchoscopy was performed. This showed complete occlusion of the left main stem bronchus secondary to an endobronchial lesion arising from the lower left bronchial tree.
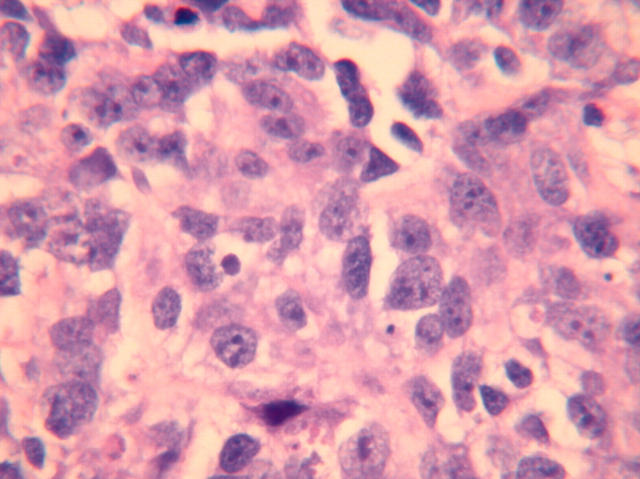
Bronchoscopic biopsy was performed. This showed poorly differentiated carcinoma with large, hyperchromatic, pleomorphic nuclei with prominent nucleoli and coarse chromatin (below right: haematoxylin and eosin, ×40 magnification). The cells had pale, vacuolated cytoplasm with indistinct cell borders. Features to suggest squamous cell carcinoma, such as sharp cytoplasmic borders and cytoplasmic keratinisation, were not seen. Features diagnostic of adenocarcinoma, such as intracytoplasmic mucin, glandular differentiation, and a papillary growth pattern, were not identified. These findings were consistent with a large cell undifferentiated carcinoma of lung.
The patient was treated with carboplatin and paclitaxel chemotherapy.