A 65 year old woman, who was diagnosed with non-obstructive apical hypertrophic cardiomyopathy 10 years ago, presented with heart failure symptoms and incessant ventricular tachycardia despite amiodarone therapy. Coronary angiogram showed normal coronary arteries.
Supplemental material showing the left ventriculography (right anterior oblique view) is available on the Heart website (http://www.heartjnl.com/supplemental/). There was severe mid-ventricular obliteration with typical features of hour-glass appearance and a large apical aneurysm. The systolic bulging of the apical aneurysm was followed by early diastolic contraction together with persistent cavity narrowing between the two chambers. A significant gradient of 100 mm Hg existed across the midventricular obliteration.
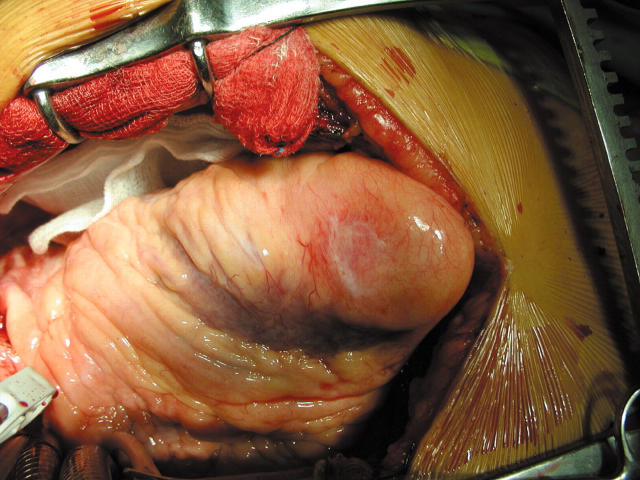
The figure shows the apical aneurysm during surgical septal myotomy and myectomy. It appeared as a thin-wall pouch arising from the LV apex with marked endocardial thinning and scarring. Successful septal myectomy was subsequently performed through the ventriculotomy after excision of the aneurysm.
Patients with mid-ventricular obliteration variant of hypertrophic obstructive cardiomyopathy are often symptomatic and prone to ventricular arrhythmias arising from the distal left ventricular aneurysm. The underlying mechanism is not known: whether the midventricular obstruction was the consequence of apical infarction in patients with hypertrophic cardiomyopathy and cavity obliteration or whether it was the high apical pressure resulting in apical infarction and apical aneurysm.
Supplementary Material
Figure 1.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.