A 76 year old man with no prior cardiac history was admitted after three episodes of syncope. With symptoms, telemetry revealed a rapid monomorphic rhythm (panel A) consistent with ventricular tachycardia (VT). ECG and cardiac markers were unremarkable. Echocardiography revealed an apical defect emptying into a large thin-walled chamber (panels B, C, D). Doppler interrogation revealed bidirectional flow between the left ventricle (LV) and this chamber, consistent with true aneurysm of the LV apex versus contained rupture of the LV apex with pseudoaneurysm formation. Cardiac catheterisation showed a 40% plaque in the mid left anterior descending coronary artery. At cardiac surgery, the abnormality was resected and the LV repaired with a pericardial patch. Recovery was uneventful with no further VT on telemetry and no VT inducible at electrophysiology study. Pathological examination of the resected tissue revealed true aneurysm with surviving myocytes scattered throughout areas of scar. Aetiology was likely an old myocardial infarction, caused by left anterior descending coronary artery thrombosis or spasm at the site of a focal and intrinsically non-obstructive plaque.
Differentiation of true aneurysm from pseudoaneurysm by echocardiography can be difficult. Here, true aneurysm was indicated by the presence of continuous endomyocardial and pericardial layers extending from the normal portion of the left ventricle throughout the aneurysmal sac. Aneurysms of the left ventricle, often associated with ventricular arrhythmias, typically form by dilation of infarct or infarct scars, although congenital and inflammatory aneurysms have been described. Resection of the aneurysm and surrounding abnormal myocardium can cure the ventricular arrhythmias, as in this case.
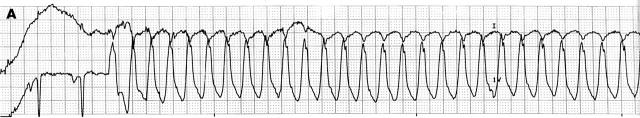
Figure 1.
Telemetry strip of leads I and V1 demonstrating the spontaneous onset of monomorphic ventricular tachycardia with a right bundle branch block pattern at approximately 280 beats/min.
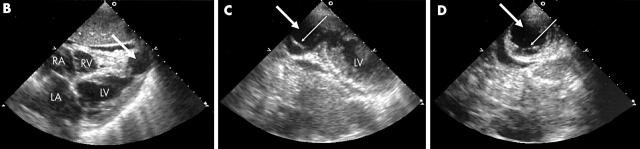
Figure 2.
Subcostal (B) and off-axis apical (C) views from transthoracic echocardiogram demonstrating left ventricular apical defect. Panel D is another apical view showing a cross section of the aneurysmal sac. Heavy arrows indicate an echo-free chamber communicating with the left ventricular cavity by an orifice with a narrow neck. Here, the definitive feature distinguishing true aneurysm from pseudoaneurysm is the presence of an endomyocardial border lining the cavity, as well as a continuous pericardial layer. Thin arrows indicate the residual myocardial layer in the wall of the aneurysmal chamber. Other findings that have been described to help distinguish between these two entities are the ratio of the maximal diameter of the neck to maximal diameter of the cavity (0.25 and 0.5 for pseudoaneurysm and 0.9 to 1 for aneurysm), and the flow characteristics of the chamber (turbulent flow by pulse Doppler in neck or within cavity in the pseudoaneurysm), which were not helpful in this case. LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle.