Hypertension, currently defined as a blood pressure > 140 mm Hg (systolic) and/or > 90 mm Hg (diastolic), is a common problem. In a western adult population the prevalence of hypertension exceeds 20%.1 The prevalence of hypertension increases with age and is higher in ethnic minority groups in the UK. In the Health Survey for England (2001) the prevalence of hypertension was 3.3% in those aged < 40 years, 27.9% in those aged between 40–79 years, and 49.9% in those aged 80 years and older.2
The two main ethnic origin groups within the UK are the Afro-Caribbean and South Asians. The majority of studies have reported a higher prevalence and significantly higher mean blood pressure levels among both Afro-Caribbean populations and South Asians compared to their white counterparts.3 In a south London community based study, compared with whites, age and sex standardised prevalence ratios for hypertension were 2.6 in people of African descent and 1.8 in those of South Asian origin.4 However, average blood pressure varies between different subgroups of South Asians, being highest in Sikhs, similar to whites in Muslims, and intermediate in Hindus.5 In addition, Indians have higher blood pressures, Pakistanis lower blood pressures, with Bangladeshis having even lower blood pressures than the native white population.6
CONSEQUENCES OF HYPERTENSION FOR ETHNIC MINORITIES
Hypertension is a major risk factor for cardiovascular and cerebrovascular disease, the major causes of death in the UK and other western countries. Recent studies indicate substantial ethnic differences in cardiovascular mortality.7 For example, compared to whites, Afro-Caribbean and people of African descent have a higher incidence of stroke8 and end stage renal failure,9 whereas coronary artery disease is less common. Conversely, South Asians (defined as people originating from the Indian subcontinent and East Africa) have a higher incidence of coronary heart disease.8
There is increased prevalence of left ventricular hypertrophy (LVH) in Afro-Caribbeans. This is thought to be, in part, due to their higher night time blood pressure with a smaller degree of nocturnal blood pressure dip. LVH is an independent predictor of morbidity and mortality. Ethnic differences in morbidity and mortality may, in part, be explained by the differences in other cardiovascular risk factors. Both diabetes mellitus and obesity are common in ethnic minority groups, with a high prevalence among Afro-Caribbean females.1 Plasma lipid concentrations, however, show a different pattern with South Asians having higher concentrations than whites and Afro-Caribbeans having lower values. This may, in part, explain why, despite a high prevalence of hypertension and type 2 diabetes mellitus, coronary heart disease is less common in Afro-Caribbean than the other two ethnic groups.10
PATHOPHYSIOLOGY OF HYPERTENSION IN ETHNIC MINORITIES
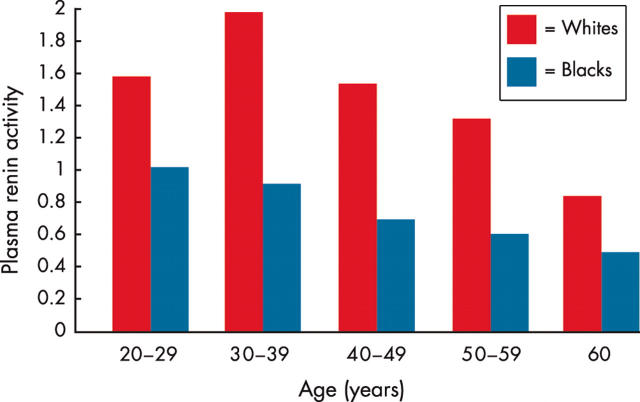
The pathophysiology of hypertension differs in black adults compared to South Asians and whites. For example, hypertension in this population is commonly of the low renin type (fig 1); sensitivity of blood pressure to salt intake is often increased, and the ability to excrete ingested salt is impaired (60–70%).11 This leads to an overall expansion of intravascular volume. Obesity is especially prevalent in black women and is associated with an increase in total body sodium content.12 Intake of dietary potassium, in the form of fruit and vegetables, is generally lower in blacks than in whites. Black patients may also have relatively higher concentrations of intracellular calcium.13 All of these factors are associated with an increased incidence of hypertension.
Figure 1.
Plasma renin in black and white hypertensive patients. Adapted from Freis et al.14
MANAGEMENT OF HYPERTENSION IN ETHNIC MINORITIES
Treatment with lifestyle modifications
Lifestyle modifications can result in improvements in blood pressure control. A 3.18 kg reduction in body weight can significantly reduce blood pressure.15 An increase in potassium intake may also significantly reduce blood pressure in normokalaemic hypertensive patients.16 This occurs, in part, because of a natriuretic effect of potassium.
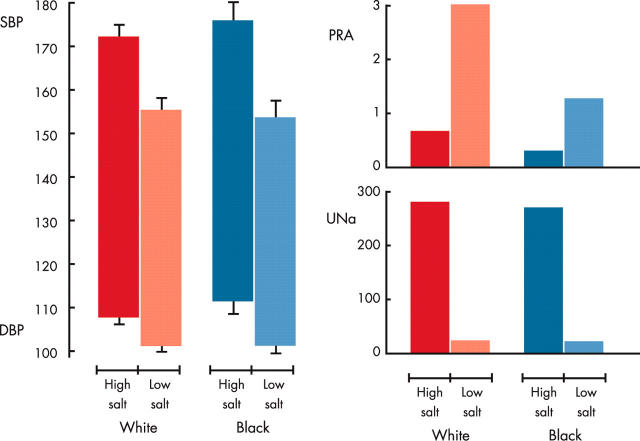
In view of the increased sensitivity of black patients to salt, restricting dietary salt intake to less than 6 g daily is particularly effective at reducing blood pressure (fig 2).17 Approximately 10% of hypertensive black adults (the percentage is higher in those who are very overweight) have an extremely high dietary sodium intake (that is, 24 hour urinary sodium excretion of 200–400 mmol per day, equivalent to a salt intake of 11–17 g daily) that is not suspected by either the patient or the physician. In these patients, it is impossible to control blood pressure adequately without using a diuretic or providing very specific dietary counselling to identify food(s) high in sodium. Optimising weight, reduction in unsaturated fat intake, and regular exercise also improves cardiovascular risk profiles.
Figure 2.
Effect of salt restriction on blood pressure in Europeans and Afro-Caribbeans. PRA, plasma renin activity (ng/ml/hour); DBP, 24 hour diastolic blood pressure (mm Hg); SBP, 24 hour systolic blood pressure; UNa, urinary sodium excretion (mmol/day). Adapted from He et al.18
Treatment with antihypertensive drugs
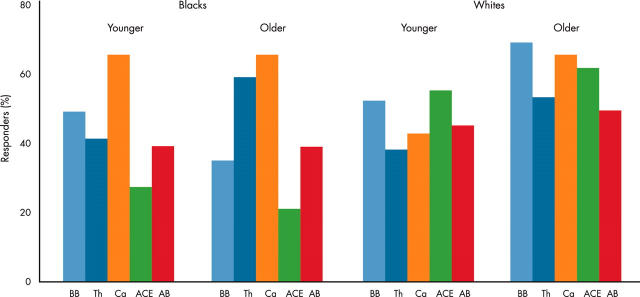
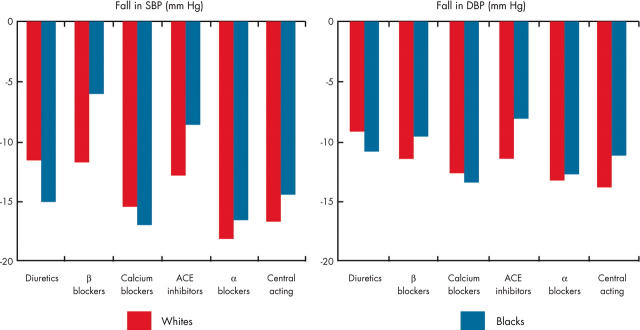
South Asians appear to respond to antihypertensive drug treatment in a similar manner to whites.2 However, there is insufficient information on this point and South Asians are under-represented in studies. The excellent blood pressure lowering efficacy of diuretics and calcium channel antagonists in hypertensive black patients is related to their characteristic volume expansion, salt sensitivity and low renin profile (figs 3–5). Diuretics should be used for initial treatment unless there is an absolute or relative contraindication (for example, gout). Randomised controlled trials have shown that diuretics reduce hypertension related morbidity and mortality in black as well as in white populations, but there is evidence of a greater decrease in blood pressure among hypertensive black patients when compared to white patients when they receive an equivalent dose of a diuretic.19 Hydrochlorothiazide in a dosage of 12.5–25.0 mg daily is a good choice but, if the concentration of serum creatinine is 2 mg/dl (177 µmol/l) or more, thiazide diuretics are usually ineffective, and a loop-type diuretic should be substituted.20 Calcium channel blockers are also extremely effective antihypertensive drugs in black patients.21
Figure 3.
Response of whites and blacks to differing antihypertensive medication: Veterans Administration study. AB, α receptor blockers; ACE, angiotensin converting enzyme inhibitors; BB, β blockers; Ca, calcium channel blockers, Th, thiazide diuretics. Adapted from Materson, et al.21
Figure 5.
Meta-analysis of monotherapy in black and white hypertensives. Adapted from Sehgal.31
Angiotensin converting enzyme (ACE) inhibitors, β blockers, and angiotensin receptor antagonists are generally less effective as monotherapy in black hypertensives,22,23 because of the tendency towards a low renin state and a lower cardiac output, with increased peripheral resistance. For example, with β blocker treatment, there was an average reduction in blood pressure of about 7/7 mm Hg in black patients compared with an average reduction of about 15/11 mm Hg in white patients.24 Increasing the dosage of the ACE inhibitor provides a slightly greater average lowering of blood pressure (to a total of about 10/8 mm Hg), but the decrease is still less than desirable.25 Ensuring a low dietary salt intake can improve the blood pressure response to ACE inhibitors in black patients.26
The effectiveness of β blockers and ACE inhibitors, in lowering blood pressure, can be increased if diuretics are used as initial or second line drug treatment in black patients with hypertension. The combination of diuretics and ACE inhibitors or β blockers produces equivalent lowering of blood pressure in whites and blacks, perhaps as a result of diuretic induced stimulation of renin release. This is true even for combination-type drugs that contain as little as 6.25–12.5 mg of hydrochlorothiazide.27 Most hypertensive black patients require two or more antihypertensive drugs to control systolic blood pressure to < 140 mm Hg and diastolic blood pressure to < 90 mm Hg. In the Veterans Affairs cooperative study,28 only 46% of black hypertensive patients with stage 1 or stage 2 disease achieved a diastolic blood pressure below 90 mm Hg with monotherapy.
However, in situations where a β blocker or an ACE inhibitor is indicated, the use of high doses and/or the addition of a diuretic improves the blood pressure response in black populations. Examples include the use of β blockers after myocardial infarction and the use of ACE inhibitors in patients with systolic heart failure (that is, ejection fraction < 40%) or those with type 1 diabetes (formerly known as insulin dependent diabetes) with proteinuria. These compelling indications apply equally to black and white patients. In these cases, the protective effect of the drugs is due to more than just reduction of blood pressure. In black hypertensive patients with type 2 (non-insulin dependent) diabetic nephropathy, evidence now shows that non-dihydropyridine calcium channel antagonists (as well as ACE inhibitors) can slow the chronic progression of renal disease.29 However, there is evidence of significant under use of these drugs for these conditions in both racial groups.22
There is limited information to date about the efficacy and tolerability of angiotensin receptor antagonists in black patients. One subgroup analysis of patients treated with valsartan suggests that it may reduce mean blood pressure, but the mean reduction is less than that seen for other ethnic groups.30
ALLHAT
With the inclusion of over 42 000 patients, ALLHAT (antihypertensive and lipid-lowering treatment to prevent heart attack trial)32 is the largest randomised controlled trial of antihypertensive treatment to date. Patients aged 55 years and older, with hypertension and at least one other risk factor for coronary heart disease (CHD)—for example, type 2 diabetes mellitus, previous myocardial infarction or stroke, left ventricular hypertrophy or smoking—were included in the study. They were randomised to either chlorthalidone, amlodipine, lisinopril, or doxazosin and assessed on the basis of morbidity and mortality from coronary artery disease.
The study included 35% (15 094 patients) black patients. The black patients were younger, had higher diastolic blood pressure levels, higher mean fasting glucose values, and greater incidence of diabetes at baseline.27 There were no significant difference in primary outcomes of non-fatal myocardial infarction or fatal CHD between chlorthalidone, amlodipine, and lisinopril in the black patients. In addition, in terms of secondary end points—namely, all cause mortality, stroke, combined CHD, and cardiovascular disease—there were no significant differences between chlorthalidone and amlodipine. In comparison to lisinopril, chlorthalidone treatment was associated with a lower risk of stroke, combined coronary artery disease, and combined cardiovascular death. The differences may be explained, in part, by the lesser blood pressure lowering effects of angiotensin converting enzyme inhibitors in black Americans. In terms of combined cardiovascular death, chlorthalidone was favourable compared to doxazosin. There was a reduced relative risk of heart failure with chlorthalidone compared to amlodipine, lisinopril, and doxazosin.
Management of hypertension in patients from ethnic minorities: key points.
In a western adult population the prevalence of hypertension exceeds 20%
Hypertension is a major risk factor for cardiovascular and cerebrovascular disease
The pathophysiology of hypertension differs in black adults compared to South Asians and whites
South Asians appear to respond to antihypertensive drug treatment in a similar manner to whites
There is excellent blood pressure lowering efficacy of diuretics and calcium channel antagonists in hypertensive black patients
ACE inhibitors, β blockers, and angiotensin receptor antagonists are generally less effective as monotherapy in black hypertensives
CONCLUSION
Hypertension is associated with significant morbidity and mortality, some of which can be reduced with effective blood pressure lowering. The prevalence of hypertension is greater in ethnic minority groups, compared to whites, within the UK. The management of hypertensives from ethnic minorities should recognise their different responses to drug treatment, the predisposing factors, and the cardiovascular consequences of hypertension.
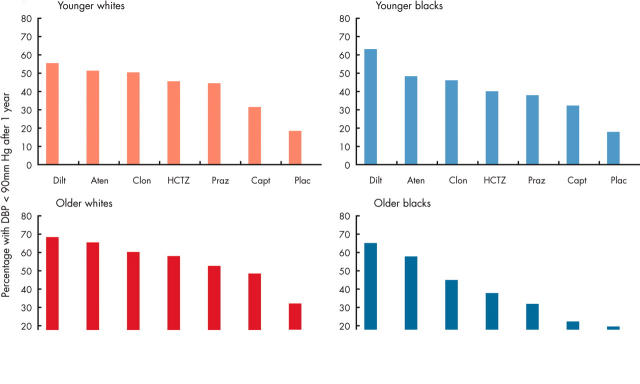
Figure 4.
Effect of age and ethnicity on response to antihypertensive medication. Aten, atenolol; Capt, captopril; Clon, clonidine; Dilt, diltiazem; HCTZ, hydrochlorothiazide; Plac, placebo; Praz, prazosin. Adapted from Materson et al.21
In compliance with EBAC/EACCME guidelines, all authors participating in Education in Heart have disclosed potential conflicts of interest that might cause a bias in the article
REFERENCES
- 1.Mayet J, Brady A. Hypertension: special issues in different ethnic groups. New perspectives in hypertension. Brady, Petrie: Merit Publishing International, 2003:124–9.
- 2.Beevers DG, Lip GYH, O’Brien E. ABC of hypertension. 4th ed. London: BMJ Publishing Group, 2001:12.
- 3.Lane DA, Lip GYH, Ethnic differences in hypert, blood pressure control in the UK. QJM 2001;94:391–6. ▸ An excellent review detailing the prevalence, treatment, and clinical implications of hypertension in ethnic minority groups in the UK. The review clarifies the conflicting epidemiological data on ethnic differences in blood pressure in the UK. [DOI] [PubMed] [Google Scholar]
- 4.Cappuccio FP, Cook DG, Atkinson RW, et al. Prevalence, detection, and management of cardiovascular risk factors in different ethnic groups in South London. Heart 1997;78:555–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McKeigue PM, Shah B, Marmot MG. Relationship of central obesity and insulin resistance with high diabetes prevalence and cardiovascular risk in South Asians. Lancet 1991;344:450–2. [DOI] [PubMed] [Google Scholar]
- 6.Agyemang C, Bhopal RS. Hypertension and coronary heart disease in South Asians. The epidemic of coronary heart disease in South Asian populations: causes and consequences. South Asian Heart Foundation 2003:108. ▸ Data from an authoritative book on cardiovascular disease in the South Asian population in the UK. The book was published by the South Asian Heart Foundation and describes evidence based practice to reduce the high burden of cardiovascular disease in South Asians.
- 7.Cruickshank JK, Beevers DG, Osbourne VL, et al. Heart attack, stroke, diabetes, and hypertension in West Indians, Asians and whites in Birmingham, England. BMJ 1980;281:1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Balarajan R. Ethnicity and variations in mortality from coronary heart disease. Health Trends 1996;28:45–51. [Google Scholar]
- 9.Raleigh VS, Kiri V, Balarajan R. Variations in mortality from diabetes mellitus, hypertension and renal disease in England and Wales by country of birth. Health Trends 1997;28:122–7. [Google Scholar]
- 10.Chaturvedi N. Ethnic differences in cardiovascular disease. Heart 2003;89:681–6. ▸ A review article that comprehensively describes the striking ethnic differences in cardiovascular disease risk. It details the differences in modes of presentation of disease and therapeutics necessitating an increased awareness among healthcare professionals of cultural differences. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hall WD. Cardiovascular therapy in black patients. In: Messerli FH, ed. Cardiovascular drug therapy. Philadelphia: Saunders, 1996:280–91.
- 12.Aloia JF, Vaswani A, Ma R, et al. Sodium distribution in black and white women. Miner Electrolyte Metab 1997;23:74–8. [PubMed] [Google Scholar]
- 13.Cho JH, Nash F, Fekete Z, et al. Increased calcium stores in platelets from African Americans. Hypertension 1995;25:377–83. [DOI] [PubMed] [Google Scholar]
- 14.Freis ED, Materson BJ, Flamenbaum W. Comparison of propranolol or hydrochlorothiazide alone for treatment of hypertension. III. Evaluation of the renin-angiotensin system. Am J Med 1983;74:1029–41. ▸ An interesting study looking at the relationship between renin activity and therapeutic response to hydrochlorothiazide and propranolol. [DOI] [PubMed] [Google Scholar]
- 15.Whelton PK, Appel LJ, Espeland MA, et al. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE) [erratum in JAMA 1998;279:1954]. JAMA 1998;279:839–46. [DOI] [PubMed] [Google Scholar]
- 16.Matlou SM, Isles CG, Higgs A, et al. Potassium supplementation in blacks with mild to moderate essential hypertension. J Hypertens 1986;4:61–4. [DOI] [PubMed] [Google Scholar]
- 17.Williams B, Poulter NR, Morris JB, et al. British Hypertension Society guidelines for hypertension management 2004 (BHS-IV). BMJ 2004;328:634–40. ▸ Latest update of the BHS incorporating new epidemiological data on cardiovascular disease risk and the importance of systolic hypertension as a determinant of risk. The guidelines hope to address the suboptimal management of hypertensive patients in the UK.15016698 [Google Scholar]
- 18.He FJ, Markandu ND, Sagnella GA, et al. Salt restriction in Europeans and Afro-Caribbeans. Hypertension 1998;32:820–4. [DOI] [PubMed] [Google Scholar]
- 19.Veterans Administration Cooperative Study Group on Antihypertensive Agents. Comparison of propranolol and hydrochlorothiazide for the initial treatment of hypertension: I. Results of short-term titration with emphasis on racial differences in response. JAMA 1982;248:1996–2003. ▸ An early study showing evidence of the increased efficacy and sensitivity of black patients to thiazide diuretics compared to whites. The study showed that race was an important determinant in deciding first line drug treatment. [PubMed] [Google Scholar]
- 20.Laragh JH, Cannon PJ, Stason WB, et al. Physiologic and clinical observations on furosemide and ethacrynic acid. Ann N Y Acad Sci 1966;139:453–65. [DOI] [PubMed] [Google Scholar]
- 21.Materson BJ, Reda DJ, Cushman WC, et al. Single-drug therapy for hypertension in men. A comparison of six antihypertensive agents with placebo. N Engl J Med 1993;328:914–21. ▸ An excellent study with direct comparison of six antihypertensive drugs with placebo in mild to moderately severe hypertension. Efficacy according to age and race was also determined, showing that antihypertensive treatment should be tailored to individual patients. [DOI] [PubMed] [Google Scholar]
- 22.Ventura HO, Frohlich ED, Messerli FH, et al. Cardiovascular effects and regional blood flow distribution associated with angiotensin converting enzyme inhibition (captopril) in essential hypertension. Am J Cardiol 1985;55:1023–6. [DOI] [PubMed] [Google Scholar]
- 23.Soumerai SB, McLaughlin TJ, Spiegelman D, et al. Adverse outcomes of underuse of beta-blockers in elderly survivors of acute myocardial infarction. JAMA 1997;277:115–21. [PubMed] [Google Scholar]
- 24.Hall WD, Israili ZI. The use of ACE inhibitors in blacks and whites. In: Schachter M, ed. ACE inhibitors: current use and future prospects. London: Dunitz, 1995:123–43.
- 25.Saunders E, Weir MR, Kong BW, et al. A comparison of the efficacy and safety of a beta-blocker, a calcium channel blocker, and a converting enzyme inhibitor in hypertensive blacks. Arch Intern Med 1990;150:1707–13. ▸ A direct comparison of the efficacy and safety of atenolol, captopril, and sustained release verapamil in black patients. This study showed that side effects of all three were minimal and comparable and that verapamil was the most effective agent. [PubMed] [Google Scholar]
- 26.Weir MR, Chrysant SG, McCarron DA, et al. Influence of race and dietary salt on the antihypertensive efficacy of an angiotensin-converting enzyme inhibitor or a calcium channel antagonist in salt-sensitive hypertensives. Hypertension 1998;31:1088–96. [DOI] [PubMed] [Google Scholar]
- 27.Moser M, Prisant LM. Low-dose combination therapy in hypertension [editorial]. Am Fam Physician 1997;56:1275–6, 1279, 1282. [PubMed] [Google Scholar]
- 28.Materson BJ. Lessons on the interaction of race and antihypertensive drugs from the VA cooperative study group on antihypertensive agents. Am J Hypertens 1995;8 (12 pt 2) :91S–3S. [DOI] [PubMed] [Google Scholar]
- 29.Bakris GL, Copley JB, Vicknair N, et al. Calcium channel blockers versus other antihypertensive therapies on progression of NIDDM associated nephropathy. Kidney Int 1996;50:1641–50. [DOI] [PubMed] [Google Scholar]
- 30.Oparil S, Dyke S, Harris F, et al. The efficacy and safety of valsartan compared with placebo in the treatment of patients with essential hypertension. Clin Ther 1996;18:797–810. [DOI] [PubMed] [Google Scholar]
- 31.Sehgal AR. Meta analysis of monotherapy in black and white hypertensives. Hypertension 2004;43:566–72. ▸ A comprehensive meta-analysis on more than 12 000 patients quantitating how often black and white patients have similar responses to specific antihypertensive drugs.14757779 [Google Scholar]
- 32.ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high risk patients randomised to angiotensin-converting enzyme inhibitor or calcium channel blocker versus diuretic. The antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT). JAMA 2002;288:2981–97. ▸ With over 42 000 patients ALLHAT was the largest randomised control trial of antihypertensive treatment to date and included 15 094 black patients. It showed that thiazide type diuretics provided effective treatment at low cost. [DOI] [PubMed] [Google Scholar]