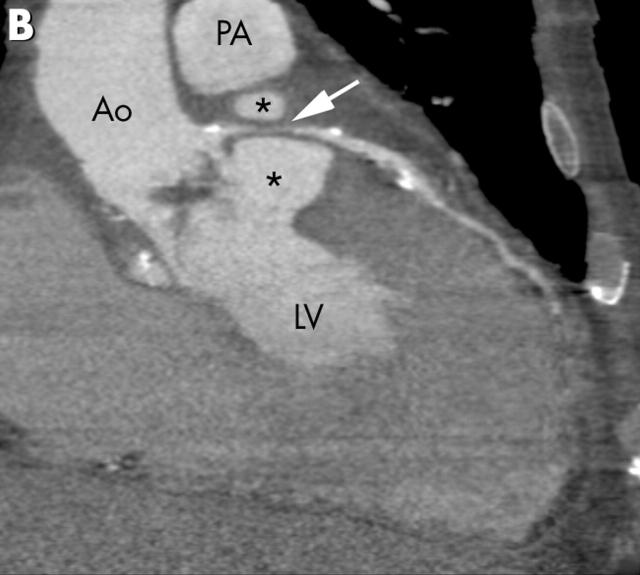
A 73 year old man with active endocarditis and high grade valvar aortic stenosis underwent biological valve replacement. His postoperative course was complicated by persistent fever and delayed recovery. Two months later he presented with chest pain, dyspnoea, and ST segment elevation on the ECG suggesting myocardial ischaemia. An electrocardiographically gated, isotropic 16 slice cardiac computed tomography (CT) examination demonstrated a destructed subvalvar portion of the left ventricular outflow tract with a leakage feeding a perivalvar cavity (panels A and B, asterisks: Ao, aorta; LA, left atrium; LV, left ventricle; PA, pulmonary artery; RVOT, right ventricular outflow tract). This cavity encircled and compressed the main branch of the left coronary artery (panels A and B, arrow). Thus, the patient underwent immediate surgery with resection of a paravalvar abscess and reconstruction of the left ventricular outflow tract.
Paravalvar abscess is an often fatal complication of aortic valve endocarditis. Thus, early diagnosis and treatment are of utmost importance. However, even transoesophageal echocardiography can miss an abscess. The case presented here demonstrates the usefulness of the latest CT technology for depicting a paravalvar abscess. The main advantages of isotropic CT are the wide field of view and the multiplanar viewing capabilities without restriction to specific imaging windows, which makes it attractive as an additional imaging method in patients with suspected endocarditis but persistent diagnostic uncertainty.