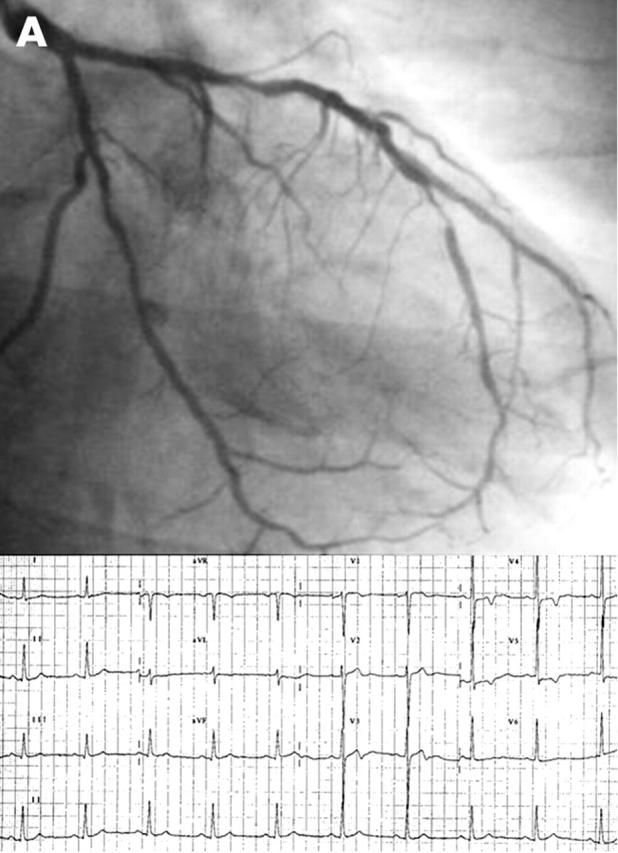
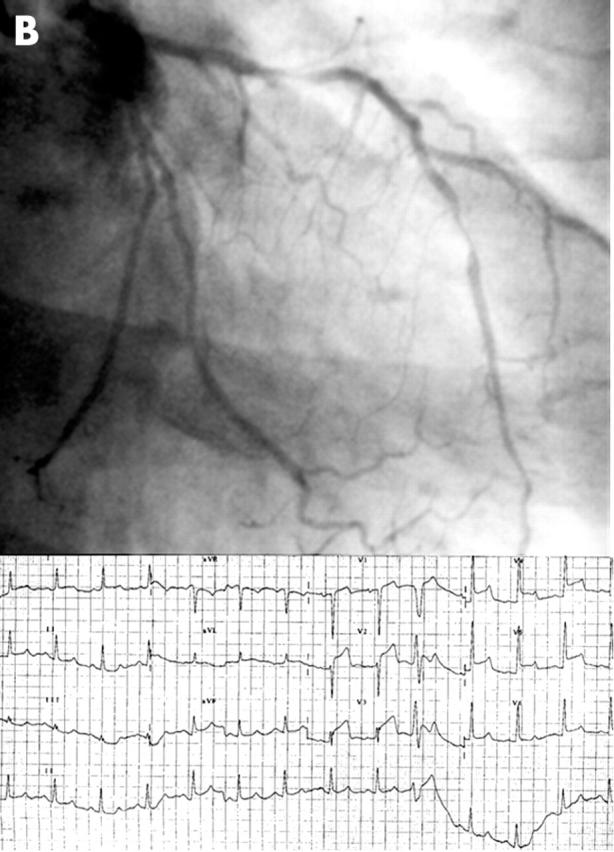
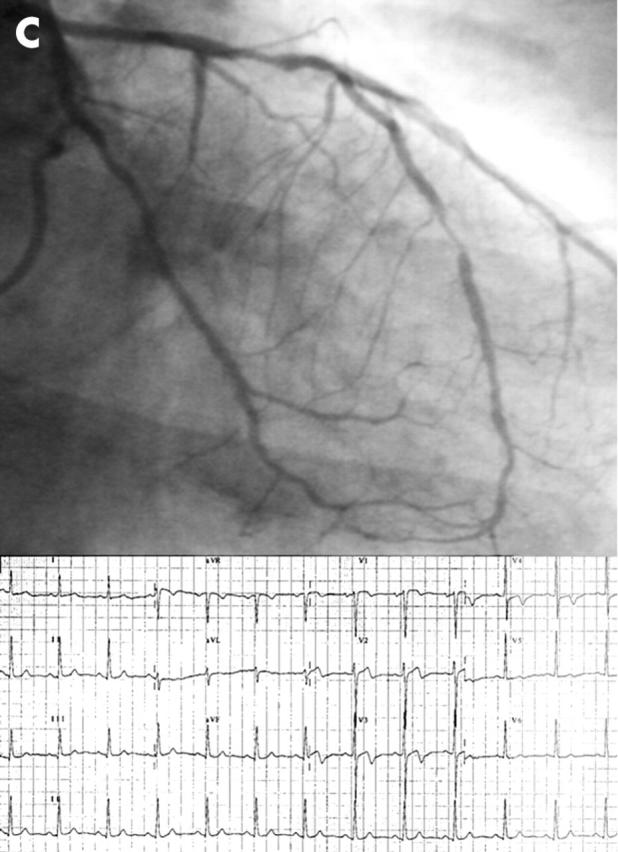
A 61 year old man was admitted to our department suffering from prolonged chest pain at rest complicated by syncope. He reported frequent episodes of typical chest pain mainly in the early morning with preserved effort tolerance. ECG recorded during chest pain revealed transient ST elevation in leads V2–V5. Coronary angiography showed irregularities of the proximal left anterior descending coronary artery (LAD) and an 80% stenosis in its middle segment (panel A). As the clinical history was suggestive of coronary spasm, we performed an intracoronary ergonovine test. After 8 μg of ergonovine, the patient developed severe LAD spasm in the proximal segment associated with angina and ST segment elevation (panel B). Notably, the severity of the stenosis in the mid LAD remained unchanged. Intracoronary nitrate administration quickly resolved the spasm, symptoms, and ST changes (panel C). We decided not to perform angioplasty on the mid LAD stenosis, because of its distal location, the increased risk conferred by spasm, and the good effort tolerance. We started medical treatment with a calcium antagonist. A maximal treadmill test on treatment was negative for inducible ischaemia. At six months follow up, the patient was symptom-free and did not show transient ECG changes on Holter monitoring.
This case underlines the importance of the clinical history for the diagnosis of vasospastic angina. Furthermore, spasm occurred proximal to the site of a critical stenosis, thus suggesting that smooth muscle hyperreactivity, rather than endothelial dysfunction, is likely to play a key role in its pathogenesis.
Figure 1.