Aortic stenosis (AS) has become the most frequent valvar heart disease and the most frequent cardiovascular disease after hypertension and coronary artery disease in Europe and North America. It primarily presents as calcific AS in adults of advanced age. The prevalence in the population older than 65 years has been reported between 2–7% and aortic sclerosis, the precursor of AS, has been found in 25%.1 Considering this high prevalence and the poor outcome of AS without cardiac surgery, this disease has definitely become a major health problem.
Besides calcific AS, the second most frequent aetiology which dominates in the younger age group is congenital AS, whereas rheumatic AS has become very rare in developed countries. Among patients with calcific AS, bicuspid valves are very common in those presenting in their 70s and 80s, whereas tricuspid valves become more common in octogenarians.
Proper physical examination remains essential in AS. It is the characteristic systolic murmur that draws attention and guides further diagnostic workup in the right direction. Doppler echocardiography is the ideal tool to confirm diagnosis and quantify AS by calculating pressure gradients and valve area, although the technique remains investigator dependent requiring special skill and experience. Heart catheterisation is mostly restricted to preoperative evaluation of coronary arteries rather than for evaluation of the valve lesion itself.
During a long latent period with increasing outflow tract obstruction, which results in increasing left ventricular pressure load, patients remain asymptomatic and acute complications are rare. However, as soon as symptoms such as exertional dyspnoea, angina, or dizziness and syncope occur, outcome becomes dismal. Average survival after the onset of symptoms has been reported to be less than 2–3 years.2 In this situation, valve replacement not only results in dramatic symptomatic improvement but also in good long term survival.2 This holds true even for patients with already reduced left ventricular function, as long as functional impairment is indeed caused by AS. Thus, there is general agreement that urgent surgery must be strongly recommended in symptomatic patients.3,4
This article primarily addresses two controversial issues on which current research efforts focus in particular: (1) the pathogenesis of calcific AS and possible ways to halt progression to severe symptomatic AS; and (2) the question of whether and when to operate on asymptomatic, haemodynamically severe AS.
PATHOGENESIS OF CALCIFIC AORTIC STENOSIS AND PREVENTION OF PROGRESSION
Calcific AS is a chronic progressive disease, starting with thickening and calcification of valve cusps without haemodynamic significance (that is, aortic sclerosis) and eventually ending in heavily calcified stiff cusps causing severe valve stenosis. The progression from aortic sclerosis, which can already easily be detected by echocardiography or computed tomography, to haemodynamically severe AS takes many years. Thus, we are faced with the rather unique situation in valvar heart disease that the disorder can be diagnosed at an early stage, offering the chance of interfering with its further progression to a clinically relevant valve problem. While calcific aortic valve disease was until recently considered a degenerative and unmodifiable process basically induced by long lasting mechanical stress, histopathologic studies have made it clear that it is an active process sharing a number of similarities with atherosclerosis.5 Inflammation, lipid infiltration, dystrophic calcification, ossification, platelet deposition, and endothelial dysfunction have been observed in both diseases and hypercholesterolaemia, raised lipoprotein Lp(a), smoking, hypertension, and diabetes have been reported to be common risk factors for both of them.5 Thus, modification of atherosclerotic risk factors may slow progression of aortic valve calcification. In addition, the renin–angiotensin system—which has been shown to play a role in atherosclerosis—may also be important in the pathogenesis of calcific AS.5,6 Thus, drugs that interfere with this system may have the potential for delaying disease progression.
The agents that have, however, gained most interest in recent years with regard to AS progression prevention are definitely statins.
Statins and aortic stenosis
The observation that AS and atherosclerosis share risk factors such as low density cholesterol and Lp(a) elevation, and the fact that statins can slow the progression of atherosclerosis, raised the hypothesis that these drugs may also delay the progression of calcific AS. Indeed, several retrospective studies have consistently demonstrated that statin treatment is associated with notably lower haemodynamic progression of AS.7–9 The question of whether this effect is dependent on cholesterol lowering or not, however, remains controversial. While Novaro et al8 have reported an association between AS progression and cholesterol values, Bellamy and colleagues7 and our group in Vienna9 could not find such an association, supporting the hypothesis that the effects of statins may rather be caused by their pleiotropic and anti-inflammatory properties than by cholesterol lowering. The beneficial effects of statin treatment do not appear to be restricted to the early stage of disease.9 Since a rapid increase of the peak aortic jet velocity among patients with severe AS and moderately to severely calcified valves has been shown to indicate a poor outcome,10 slowing disease progression in these patients may still beneficially alter their outcome with respect to the development of symptoms and the necessity of surgery. Thus, current data suggest that statin treatment may be indicated in any patient with AS, regardless of AS severity and cholesterol values.
Final conclusions on the efficacy of statin treatment can, however, only be drawn from prospective randomised controlled trials. Preliminary data with surprisingly negative results were presented at the last annual sessions of the American Heart Association.11 However, this study may not have comprised enough patients (n = 155) and the follow up may have been too short (26 months on average). Therefore, one must wait for the results of ongoing large multicentre trials.
Renin–angiotensin system and aortic stenosis
The fact that angiotensin converting enzyme (ACE) and angiotensin II can be found in sclerotic but not in normal aortic valves suggests a potential role for the renin–angiotensin system in the pathogenesis of calcific AS.5,6 ACE is also found in atherosclerotic lesions and angiotensin II is assumed to contribute to the atherosclerotic process via its pro-inflammatory effects. Clinical trials have demonstrated clinical benefit of treatment with agents that block the renin–angiotensin system components in patients who either have had or are at high risk for atherosclerosis, suggesting similar effects in calcific AS. Indeed, ACE inhibitors have recently been shown to slow the calcium accumulation in aortic valves in a retrospective study using electron beam computed tomography.12 So far, there has only been one study evaluating the effects of ACE inhibitors on the haemodynamic progression of AS.9 This retrospective analysis, however, could not find any difference in progression rates between patients with and without ACE inhibitor treatment. Nevertheless, it could still be that the initiation of ACE inhibitor treatment at an earlier stage of disease and longer treatment may have positive effects on disease progression. Further studies may therefore be required.
In conclusion, there is so far no solid evidence that AS progression can be prevented with any medical treatment and it is too early for treatment recommendations.
WHEN TO OPERATE ON ASYMPTOMATIC AS
While there is consensus that urgent valve replacement is required in symptomatic AS, the management of asymptomatic patients with severe AS remains a matter of controversy.2,3 Because of the widespread use of Doppler echocardiography it is estimated that about 50% of patients who come to medical attention with severe AS are still asymptomatic. Thus, cardiologists are increasingly faced with the difficult decision whether to operate on asymptomatic patients with severe AS or not. The following prognostic reasons could potentially favour elective surgery in an asymptomatic patient: prevention of sudden cardiac death; prevention of irreversible myocardial damage; lowering surgical risk by performing valve replacement early; and certainty that the symptom-free phase of haemodynamically severe AS can only be very short and surgery is inevitable within a short time interval anyway.
Prevention of sudden cardiac death
Sudden death is probably the major concern when asymptomatic patients with severe AS are followed conservatively. How likely is sudden death in asymptomatic AS? Besides several studies which included patients with non-severe AS and did not observe sudden deaths, there are now two prospective studies reporting the outcome of sizeable cohorts of patients with exclusively severe AS (peak aortic jet velocity ⩾ 4.0 m/s). Pellikka et al13 observed two sudden deaths among 113 patients during a mean follow up of 20 months. Both patients, however, had developed symptoms at least three months before death. We have reported one sudden death that was not preceded by any symptoms among 104 patients followed for 27 months on average.10 Thus, sudden death—although a common cause of death in symptomatic patients—appears to be a very rare event in asymptomatic AS (< 1%/year). It also has to be considered that sudden death has even been reported after successful valve replacement and, thus, this risk can apparently not be entirely eliminated by surgical treatment. Thus, prevention of sudden death is not a strong argument for surgery in asymptomatic patients.
However, patients unfortunately do not always promptly report their symptoms. In addition it has to be considered that in some countries patients may wait several months for surgery. Mortality has, however, been reported to be quite significant already within the following months after symptom onset. In a Scandinavian study,14 for example, seven of 99 patients with severe aortic stenosis who were scheduled for surgery died during an average waiting period of six months.
Prevention of irreversible myocardial damage
In contrast to valvar regurgitation, patients with asymptomatic severe AS who have already developed impaired systolic left ventricular function are extremely uncommon. It has been speculated, however, that myocardial fibrosis and severe left ventricular hypertrophy that may not be reversible after delayed surgery could preclude an optimal postoperative long term outcome. However, there are, so far, no data to confirm this hypothesis,3 and the excellent outcome after valve replacement in isolated AS with normal systolic left ventricular function raises doubts that the risk of developing irreversible hypertrophy and myocardial fibrosis during the asymptomatic phase may become a strong argument to operate on asymptomatic patients. Further studies are, however, required to clarify this question.
Surgical considerations
Patients with severe symptoms have been found to have a significantly higher operative mortality than those with no or only mild symptoms. According to the Society of Thoracic Surgeons US cardiac surgery database 1997, for example, patients in New York Heart Association (NYHA) classes I or II had an operative mortality of less than 2% compared with 3.7% and 7.0% for patients in NYHA class III and IV, respectively.15 In addition, urgent or emergent valve replacement carries a significantly higher risk than elective surgery.15 Nevertheless, operative risk, even if it is small, must always be weighed against the potential benefit. Although operative mortality can ideally be in the range of 2–3% it may be as high as 10% in the elderly and even higher in the presence of significant co-morbidity.16 Even more importantly, not only must operative risk be considered but also prosthetic valve related long term morbidity and mortality must be taken into account. Thromboembolism, bleeding, endocarditis, valve thrombosis, paravalvar regurgitation, and valve failure occur at the rate of at least 2–3% per year and death directly related to the prosthesis has been reported at a rate of up to 1% per year.3 This again underscores that surgery cannot be justified early when a net benefit is not proven for the patient.
Duration of the asymptomatic phase
Some studies reported a very rapid progression and thus poor outcome, with up to 80% of the patients requiring valve replacement within two years.17 Such observations have also raised the question of whether it is worthwhile to delay surgery in still asymptomatic patients. However, other investigators have reported better outcome and individual outcome varies widely. For example, survival free of death or valve replacement indicated by the development of symptoms was 56 (5)% at two years in our series of asymptomatic patients with severe AS.10 These discrepant results may be explained by the fact that in some studies patients underwent surgery without having developed symptoms while these interventions were, nevertheless, counted as events. Thus, the event-free survival reported in the literature has to be viewed with caution.
In conclusion, it appears unlikely from current data that the potential benefit of valve replacement can outweigh the risk of surgery and the long term risk of prosthesis related complications in all asymptomatic patients. Surgery is, therefore, not generally recommended in AS before symptom onset.3,4 In particular, the fact that patients frequently do not present immediately when symptoms develop and that some need to wait some time for surgery while being symptomatic represents, however, significant risk; the ideal approach would therefore be to refer patients for surgery just before symptom onset. Risk stratification with identification of those patients who are likely to develop symptoms within a short time interval could definitely optimise the timing of surgery.
RISK STRAFICATION IN ASYMPTOMATIC SEVERE AORTIC STENOSIS
Risk stratification by echocardiography
Among the echocardiographic parameters, peak aortic jet velocity and ejection fraction13 as well as the rate of haemodynamic progression17 have been identified as independent predictors of outcome. However, these findings were obtained retrospectively and did not allow any specific recommendations on how to select prospectively high risk patients who may benefit from early elective surgery.
Aortic valve calcification has turned out to be a powerful independent predictor of outcome.10 Event-free survival at four years was 75 (9)% in patients with no or only mild calcification versus 20 (5)% in those with moderately or severely calcified valves. The worse outcome of patients with more severe calcification appeared to be paralleled by a more rapid haemodynamic progression. However, even in the presence of calcification the rate of haemodynamic progression varies widely.2,10 In fact, the haemodynamic progression as determined by serial echocardiographic examination appears to yield important prognostic information in addition to the degree of calcification. The combination of a notably calcified valve with a rapid increase in velocity of ⩾ 0.3 m/s from one to the following visit within one year has been shown to identify a high risk group of patients. Approximately 80% of them required surgery or died within two years.10 This criterion has been included in the European recommendations as a IIa indication for valve replacement.4
Risk stratification by exercise testing
Although an abnormal exercise test is considered a probable indication for valve replacement in current guidelines,3,4 this recommendation was based on weak data. Amato and colleagues18 performed exercise testing in 66 asymptomatic patients with an aortic valve area < 1.0 cm2 and followed them for 15 (12) months. Criteria for a positive test were occurrence of symptoms, new ST segment depression, systolic blood pressure increase < 20 mm Hg or complex ventricular arrhythmias. At 24 months, event-free survival with events defined as development of symptoms in daily life or death was 85% in 22 patients with negative test but only 19% (including four sudden deaths) in patients with a positive test. Although these results look impressive they leave many open questions. The majority of patients with a positive test fulfilled the criterion of symptom development. In particular, three of the patients who died had symptoms during the test. Although the study allowed the conclusion that patients with a negative exercise test appear to have a good outcome and may not require surgery whereas those limited by typical symptoms should undergo valve replacement, the positive predictive value of an abnormal blood pressure response and/or ST segment depression without occurrence of symptoms remained unclear.
Until recently, there were no other studies providing more detailed data on the predictive accuracy of these criteria. However, Das and colleagues19 were able to clarify some of the open questions. In 125 patients with asymptomatic AS (effective valve area 0.9 (0.2) cm2), they assessed the accuracy of exercise testing in predicting symptom onset within 12 months. Similar to previous reports, approximately one third of the patients were found to develop symptoms on exercise. Abnormal blood pressure response, more strictly defined as no increase in systolic blood pressure at peak exercise compared to baseline, was found in 23% and ST segment depression of >2 mm in 26% of patients. There were no deaths during follow up but 29% of their patients developed spontaneous symptoms. Absence of limiting symptoms had a high negative predictive accuracy of 87%. An abnormal blood pressure response or ST segment depression, however, gave no significant benefit above limiting symptoms with respect to predictive accuracy. In the absence of limiting symptoms, only two patients with abnormal blood pressure response, two with ST depression, and one with both developed symptoms during follow up. Negative predictive values were 78% and 77% and positive predictive values 48% and 45%, respectively. These findings suggest that abnormal blood pressure response and ST depression are rather non-specific findings and not helpful for identifying asymptomatic patients who may benefit from elective valve replacement.
Even limiting symptoms on exercise testing had a positive predictive accuracy of only 57% in the present study when including all patients and all symptoms. When considering only physically active patients younger than 70 years, positive predictive accuracy rose to 79%. Apparently, it also matters which symptoms occur on exercise testing: in the entire study group, 83% of patients with dizziness developed spontaneous symptoms compared to only 50% of patients with chest tightness and 54% of patients with breathlessness. The most likely explanation for these findings is that breathlessness on exercise may be difficult to interpret in patients with only low physical activity and particularly in older patients (> 70 years). In this group it will be difficult to decide whether breathlessness on exercise is indeed a symptom of AS.
Thus, exercise testing is primarily helpful in physically active patients younger than 70 years. A normal exercise test indicates a very low likelihood of symptom development within 12 months and watchful waiting is safe. On the other hand, clear symptom development on exercise testing in physically active patients younger than 70 years indicates a very high likelihood of symptom development within 12 months and valve replacement should be recommended. However, abnormal blood pressure response and/or ST segment depression without symptoms on exercise have a low positive predictive value and may not justify elective surgery.
Risk stratification by neurohormones
Plasma concentrations of cardiac neurohormones have been shown to increase with the haemodynamic severity of AS and with increasing symptoms. More importantly, we recently reported that plasma concentrations of neurohormones may predict symptom-free survival in AS.20 Patients with brain natriuretic peptide (BNP) concentrations < 130 pg/ml or N-terminal BNP concentrations < 80 pmol/l were unlikely to develop symptoms within nine months (symptom-free survival close to 90%) whereas those with higher concentrations frequently required surgery within this time period (symptom-free survival less than 50%). Thus, serial measurements of neurohormones during follow up may also help to identify the optimal time for surgery.
Recommendations for surgery in current American and European practice guidelines and suggestions for a practical approach to the management of AS are summarised in fig 1 and table 1.
Figure 1.
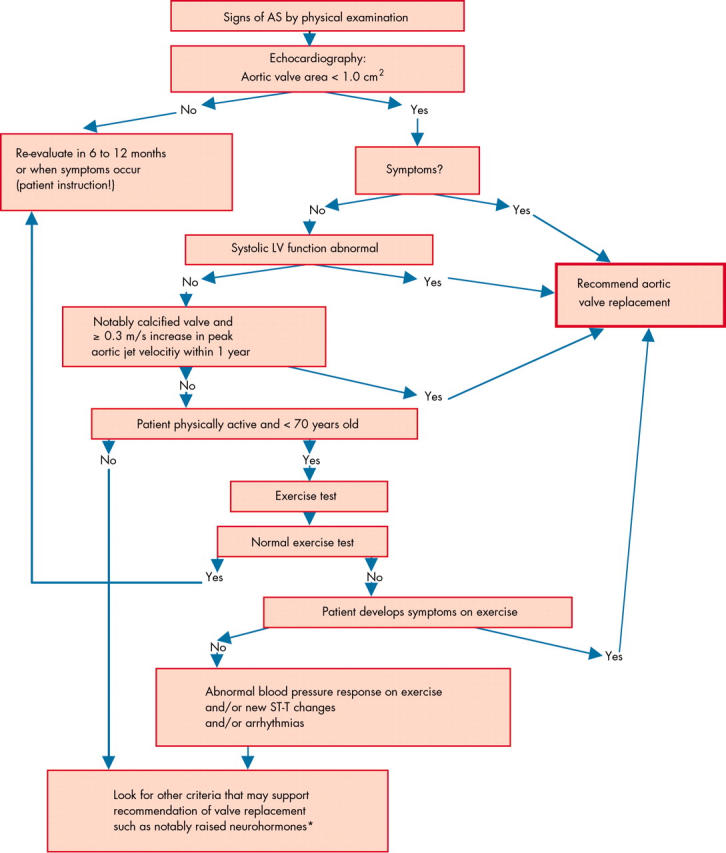
Stepwise approach to the management of patients with aortic stenosis. *Raised plasma concentrations of neurohormones may become an independent indication for surgery when confirmed by further studies and then may step up in the decision algorithm. Their serial measurement at follow up visits may be helpful. LV, left ventricle.
Table 1.
Recommendations for aortic valve replacement in asymptomatic severe AS
| Indication class | ACC/AHA guidelines3 | ESC Recommendations4 |
| I | Patients undergoing coronary artery bypass surgery | Patients undergoing coronary artery bypass surgery |
| I | Patients undergoing surgery of the ascending aorta | Patients undergoing surgery of the ascending aorta |
| IIa | Patients with systolic left ventricular dysfunction | Patients with systolic left ventricular dysfunction |
| IIa | Patients with abnormal response to exercise (for example, hypotension) | Patients with abnormal response to exercise (development of symptoms, blood pressure fall, blood pressure rise <20 mm Hg, impaired exercise tolerance (<80%), new ST depression >2 mm, complex ventricular arrhythmias) |
| IIa | Patients with moderate to severe valve calcification, a peak jet velocity >4 m/s, and a rate of peak velocity progression ⩾0.3 m/s/year | |
| IIb | Patients with excessive LV hypertrophy (⩾15 mm) | Patients with severe LV hypertrophy (>15 mm) |
| Unless this is due to hypertension | ||
| IIb | Patients with ventricular tachycardia | Patients with complex ventricular arrhythmias for which no other cause can be identified |
| IIb | Patients with valve area <0.6 cm2 |
ACC, American College of Cardiology; AHA, American Heart Association; AS, aortic stenosis; ESC, European Society of Cardiology; LV, left ventricle.
MULTIPLE CHOICE QUESTIONS.
Education in Heart Interactive (www.heartjnl.com/misc/education.shtml)
There are six multiple choice questions associated with each Education in Heart article (these questions have been written by the authors of the articles). Each article is submitted to EBAC (European Board for Accreditation in Cardiology; www.ebac-cme.org) for 1 hour of external CPD credit.
How to find the MCQs: Click on the Online Learning: [Take interactive course] link on the table of contents for the issue online or on the Education in Heart collection (www.heartjnl.com/cgi/collection/heart_education).
Free access: This link will take you to the BMJ Publishing Group’s online learning website. Your Heart Online user name and password will be recognised by this website. As a Heart subscriber you have free access to these MCQs but you must register on the site so you can track your learning activity and receive credit for completed courses.
How to get access: If you have not yet activated your Heart Online access, please do so by visiting http://www.bmjjournals.com/cgi/activate/basic and entering your six digit (all numeric) customer number (found above your address label with your print copy). If you have any trouble activating or using the site please contact subscriptions@bmjgroup.com
Case based Heart: You might also be interested in the interactive cases published in association with Heart (http://cpd.bmjjournals.com/cgi/hierarchy/cpd_node;CBH)
In compliance with EBAC/EACCME guidelines, all authors participating in Education in Heart have disclosed potential conflicts of interest that might cause a bias in the article
REFERENCES
- 1.Stewart BF, Siscovick D, Lind BK, et al. Clinical factors associated with calcific aortic valve disease. Cardiovascular health study. J Am Coll Cardiol 1997;29:630–4. [DOI] [PubMed] [Google Scholar]
- 2.Rosenhek R, Maurer G, Baumgartner H. Should early elective surgery be performed in patients with severe but asymptomatic aortic stenosis. Eur Heart J 2002;23:1417–21. ▸ Comprehensive review providing more references regarding natural history and surgical outcome. Discussion of pros and cons for elective surgery. [DOI] [PubMed] [Google Scholar]
- 3.Bonow RO, Carabello B, de Leon AC, et al. ACC/AHA guidelines for the management of patients with valvular heart disease. A report of the American College of Cardiology/American Heart Association task force on practice guidelines (committee on management of patients with valvular heart disease). J Am Coll Cardiol 1998;32:1486–588. ▸ Current ACC/AHA practice guidelines including a comprehensive overview of the available literature until 1998. [DOI] [PubMed] [Google Scholar]
- 4.Iung B, Gohlke-Barwolf, Tornos P, et al. on behalf of the Working Group on Valvular Heart Disease. Recommendations on the management of the asymptomatic patient with valvular heart disease. Eur Heart J 2002;23:1253–66. ▸ Current recommendations of the working group on valvular heart disease of the European Society of Cardiology including studies published after 1998 (compare with reference 3). [DOI] [PubMed] [Google Scholar]
- 5.Mohler ER. Mechanisms of aortic valve calcification. Am J Cardiol 2004;94:1396–402. ▸ Comprehensive overview of the pathologic mechanisms of calcific aortic stenosis. [DOI] [PubMed] [Google Scholar]
- 6.O’Brien KD, Shavelle DM, Caulfield MT, et al. Association of angiotensin-converting enzyme with low-density lipoprotein in aortic valvular lesions and in human plasma. Circulation 2002;106:2224–30. [DOI] [PubMed] [Google Scholar]
- 7.Bellamy MF, Pellikka PA, Klarich KW, et al. Association of cholesterol levels, hydroxymethylglutaryl coenzyme-A reductase inhibitor treatment, and progression of aortic stenosis in the community. J Am Coll Cardiol 2002;40:1723–30. ▸ This study, together with references 8 and 9, provided much of the current information on the effect of statins on the progression of aortic stenosis. [DOI] [PubMed] [Google Scholar]
- 8.Novaro GM, Tiong IY, Pearce GL, et al. Effect of hydroxymethylglutaryl coenzyme A reductase inhibitors on the progression of calcific aortic stenosis. Circulation 2001;104:2205–9. [DOI] [PubMed] [Google Scholar]
- 9.Rosenhek R, Rader F, Loho N, et al. Statins but not ACE inhibitors delay progression of aortic stenosis. Circulation 2004;110:1291–5. [DOI] [PubMed] [Google Scholar]
- 10.Rosenhek R, Binder T, Porenta G, et al. Predictors of outcome in severe, asymptomatic aortic stenosis. N Engl J Med 2000;343:611–7. ▸ This study, together with reference 13, provided important information on the natural history of asymptomatic severe aortic stenosis. [DOI] [PubMed] [Google Scholar]
- 11.Cowell SJ, Newby DE, White A, et al. Intensive lipid-lowering therapy does not halt the progression of calcific aortic stenosis. Circulation 2004;110 (suppl III) :III710. [Google Scholar]
- 12.O’Brien KD, Probstfield J, Caulfield MT, et al. Angiotensin-converting enzyme inhibitors and change in aortic valve calcium. Arch Intern Med 2005;165:858–62. [DOI] [PubMed] [Google Scholar]
- 13.Pellikka PA, Nishimura RA, Bailey KR, et al. The natural history of adults with asymptomatic, hemodynamically significant aortic stenosis. J Am Coll Cardiol 1990;15:1012–17. [DOI] [PubMed] [Google Scholar]
- 14.Lund O, Nielsen TT, Emmertsen K, et al. Mortality and worsening of prognostic profile during waiting time for valve replacement in aortic stenosis. Thorac Cardiovasc Surg 1996;44:289–95. [DOI] [PubMed] [Google Scholar]
- 15.Society of Thoracic Surgeons. STS national database: STS U.S. cardiac surgery database: 1997, Aortic valve replacement patients: preoperative risk variables. Chicago: Society of Thoracic Surgeons, 2000. http://www.ctsnet.org/doc/3031.
- 16.Otto CM. Timing of aortic valve surgery. Heart 2000;84:211–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Otto CM, Burwash IG, Legget ME, et al. Prospective study of asymptomatic valvular aortic stenosis. Clinical, echocardiographic, and exercise predictors of outcome. Circulation 1997;95:2262–70. [DOI] [PubMed] [Google Scholar]
- 18.Amato MC, Moffa PJ, Werner KE, et al. Treatment decision in asymptomatic aortic valve stenosis: role of exercise testing. Heart 2001;86:381–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Das P, Rimington H, McGrane H, et al. Exercise testing to stratify risk in aortic stenosis. Eur Heart J 8April2005; [Epub ahead of print]. ▸ This study provided, so far, the most detailed information on the predictive value of exercise testing in asymptomatic aortic stenosis. [DOI] [PubMed]
- 20.Bergler-Klein J, Klaar U, Herger M, et al. Natriuretic peptides predict symptom-free survival and postoperative outcome in severe aortic stenosis. Circulation 2004;109:2302–8. [DOI] [PubMed] [Google Scholar]


