Abnormalities of coronary microcirculation without large vessel atherosclerosis have been known in patients with non-insulin dependent diabetes mellitus (NIDDM). Coronary flow reserve (CFR) has been considered an important physiological parameter in the coronary circulation reflecting the function of large epicardial arteries and the microcirculation, including endothelial function. Reduced CFR and impaired endothelium mediated, nitric oxide dependent coronary vasodilatation1,2 have been observed in NIDDM without overt coronary artery disease.
Asymmetric dimethylarginine (ADMA) is a major endogenous nitric oxide synthase inhibitor and has been considered a novel risk factor of cardiovascular disease.3 Serum or plasma concentration of ADMA is increased in patients with NIDDM3 and may attenuate vascular function. However, to our knowledge, the relation between ADMA and CFR has not been examined in patients with NIDDM. Our goal was to examine the relation between serum ADMA concentration and CFR in patients with NIDDM by means of non-invasive transthoracic Doppler echocardiography.
METHODS
We studied 47 patients with NIDDM without a history of cardiovascular disease. We limited our study population to non-smokers and patients treated with diet or oral hypoglycaemic agents alone. All patients underwent two dimensional echocardiography and a treadmill exercise test to exclude patients with wall motion abnormality, atrial fibrillation, left ventricular hypertrophy (wall thickness at end diastole > 12 mm), valvar heart disease, and overt coronary artery disease. We sampled venous blood and measured coronary flow velocity by transthoracic Doppler echocardiography after obtaining written informed consent. The study protocol was approved by the committee on medical ethics and clinical investigation of Chiba University Hospital.
Blood samples were taken immediately before transthoracic Doppler echocardiography to determine the serum concentration of ADMA, fasting blood sugar, glycated haemoglobin (HbA1c), and lipid profile. We obtained serum ADMA concentration measurements from SRL, Inc (Tachikawa, Tokyo, Japan). High performance liquid chromatography was used to measure ADMA by orthophthaldialdehyde for fluorescence determination.
Echocardiographic examinations were performed with a SONOS 5500 digital ultrasound system (Philips Medical Systems, Andover, Massachusetts, USA). We obtained standard M mode images and calculated left ventricular mass according to the cube formula. Coronary blood flow velocity in the distal portion of the left anterior descending coronary artery was measured by transthoracic Doppler echocardiography with a high frequency transducer (5–7 MHz) under the guidance of colour Doppler flow mapping.4 Intravenous adenosine was administered (0.14 mg/kg/min) to induce hyperaemia. Mean diastolic velocities were measured at baseline and peak hyperaemic conditions and were averaged over three cardiac cycles. CFR was defined as the ratio of hyperaemic to basal mean diastolic velocity.
Relations between CFR and age, body mass index, blood pressure, heart rate, left ventricular mass, fasting blood sugar, HbA1c, lipid profile, and ADMA were evaluated by Pearson’s method. Multiple regression analysis was performed for independent effects of potential determinants on CFR. A probability value of p < 0.05 was considered significant.
RESULTS
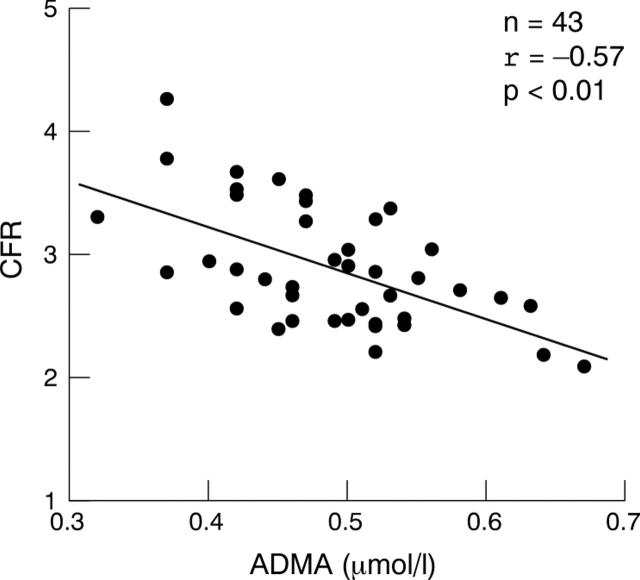
Because four patients were excluded by treadmill exercise testing, we studied 43 patients (mean (SD) age 65 (10) years, body mass index 23.3 (3.2) kg/m2, 26 men). Thirty eight patients (88%) received the oral hypoglycaemic agent sulfonylurea. Two patients were receiving lipid lowering treatment; none were taking thiazolidinediones or any other medication known to affect endothelial function. Table 1 shows the results of venous blood sample, haemodynamic, and echocardiographic data. Adequate recordings of coronary flow for the assessment of CFR were obtained from all patients. Interobserver and intraobserver variabilities for the measurement of Doppler velocity recordings were 5.0% and 3.9%, respectively. There were no correlations between CFR and body mass index, blood pressure, heart rate, left ventricular mass, fasting blood sugar, HbA1c, and lipid profile. On the other hand, CFR was inversely correlated with age (r = −0.34, p < 0.05) and serum ADMA concentration (r = −0.57, p < 0.01) (fig 1). Multiple regression analysis to assess independent associations of CFR (with age, sex, body mass index, blood pressure, heart rate, left ventricular mass, fasting blood sugar, HbA1c, lipid profile, and ADMA) showed that only serum ADMA concentration was independently associated with CFR (β = −0.41, p < 0.05).
Table 1.
Venous blood sample, haemodynamic, and echocardiographic data
| Variable | Mean (SD) |
| FBS (mmol/l) | 9.5 (2.8) |
| HbA1c (%) | 7.2 (1.0) |
| Total cholesterol (mmol/l) | 5.1 (0.9) |
| Triglycerides (mmol/l) | 1.6 (1.1) |
| HDL cholesterol (mmol/l) | 1.4 (0.3) |
| LDL cholesterol (mmol/l) | 2.9 (0.8) |
| ADMA (µmol/l) | 0.49 (0.07) |
| Blood pressure (mm Hg) | 127.7 (20.6)/66.3 (11.0) |
| Heart rate (beats/min) | 69.5 (11.8) |
| Left ventricular mass (g) | 146.7 (40.4) |
| Basal MDV (m/s) | 0.22 (0.06) |
| Hyperaemic MDV (m/s) | 0.63 (0.16) |
| Coronary flow reserve | 2.89 (0.49) |
ADMA, asymmetric dimethylarginine; FBS, fasting blood sugar; HbA1c, glycated haemoglobin; HDL, high density lipoprotein; LDL, low density lipoprotein; MDV, mean diastolic velocity.
Figure 1.
Inverse correlation between coronary flow reserve (CFR) and serum asymmetric dimethylarginine (ADMA) concentration.
DISCUSSION
The present study shows that in patients with NIDDM serum ADMA concentration and CFR are inversely correlated and circulating ADMA and CFR are independently inversely associated. Coronary endothelial vasodilator dysfunction is known to predict long term atherosclerotic disease progression and cardiovascular event rates. Coronary endothelial vasodilator dysfunction has also been reported in patients with NIDDM2 and has been considered to be the earliest change in the process of atherosclerosis. In addition, experimental study showed that increased plasma ADMA concentration is important in the pathophysiology of coronary endothelial vasodilator dysfunction in NIDDM.5 Our results suggest that in NIDDM endothelial dysfunction by ADMA accumulation may partly explain the attenuated CFR in the clinical setting and, therefore, ADMA may be a useful marker of coronary microcirculation. In this study, we found no relation between fasting blood sugar, HbA1c, and CFR in our patients, although a correlation between long term glycaemic control and myocardial flow reserve was previously reported in NIDDM.1 This finding indicates that coronary microcirculation cannot be estimated from short term glycaemic control because temporal fasting blood sugar and HbA1c may not necessarily reflect CFR. Therefore, serum ADMA concentration may be related more sensitively than fasting blood sugar and HbA1c to coronary microcirculation.
In summary, serum ADMA concentration correlates with CFR in patients with NIDDM, independently of temporary glycaemic control. Serum ADMA concentration may be a sensitive marker of coronary microcirculation in patients with NIDDM without evidence of coronary artery disease.
Acknowledgments
This study was supported by a research grant for cardiovascular disease (14C-3) from the Ministry of Health, Labour, and Welfare, Japan.
Abbreviations
ADMA, asymmetric dimethylarginine
CFR, coronary flow reserve
HbA1c, glycated haemoglobin
NIDDM, non-insulin dependent diabetes mellitus
REFERENCES
- 1.Yokoyama I, Momomura S, Ohtake T, et al. Reduced myocardial flow reserve in non-insulin dependent diabetes mellitus. J Am Coll Cardiol 1997;30:1472–7. [DOI] [PubMed] [Google Scholar]
- 2.Nitenberg A, Valensi P, Sachs R, et al. Impairment of coronary vascular reserve and ACh-induced coronary vasodilation in diabetic patients with angiographically normal coronary arteries and normal left ventricular systolic function. Diabetes 1993;42:1017–25. [DOI] [PubMed] [Google Scholar]
- 3.Cooke JP. Does ADMA cause endothelial dysfunction? Arterioscler Thromb Vasc Biol 2000;20:2032–7. [DOI] [PubMed] [Google Scholar]
- 4.Hozumi T, Yoshida K, Akasaka T, et al. Noninvasive assessment of coronary flow velocity and coronary flow velocity reserve in the left anterior descending coronary artery by Doppler echocardiography: comparison with invasive technique. J Am Coll Cardiol 1998;32:1251–9. [DOI] [PubMed] [Google Scholar]
- 5.Lin KY, Ito A, Asagami T, et al. Impaired nitric oxide synthase pathway in diabetes mellitus. Role of asymmetric dimethylarginine and dimethylarginine dimethylaminohydrolase. Circulation 2002;106:987–92. [DOI] [PubMed] [Google Scholar]