Abstract
Objectives
Teriparatide [rhPTH (1-34)] is an effective treatment for osteoporosis administered by daily subcutaneous injection. The objective of this study was to determine how much benefit women expect teriparatide to confer before agreeing to perform daily injections.
Methods
We recruited postmenopausal women who had recently undergone bone densitometry and were found to have either a T score less than −2.5 at the hip or spine and/or had a Fracture Index (FI) of ≥ 6. Participants completed an Adaptive Conjoint Analysis questionnaire to determine their treatment preferences.
Results
The study sample included 185 women, mean age 71 (range 46 to 90). An increasing number of subjects preferred rhPTH (1-34) as the efficacy of teriparatide increased, but most women demanded efficacy advantages greater than those demonstrated in clinical studies. We found no association between absolute fracture risk and preference for rhPTH (1-34); however, subjects with an excessively high perceived risk of future fracture were more likely to accept daily subcutaneous injections compared to subjects with a lower perceived risk of future fracture (40% versus 15%, p=0.001).
Conclusions
Our results suggest that most women demand benefits far greater than those conferred by rhPTH (1-34) in order to administer daily subcutaneous injections to decrease their future risk of fractures.
Practice Implications
Given the poor adherence for treatment of osteoporosis, and the choices older adults must make when paying for medications, development of novel treatment approaches should be based on older adults' treatment preferences.
Keywords: Osteoporosis, Bisphosphonates, Recombinant Human Parathyroid Hormone, Decision-Making
1. Introduction
In the U.S. today, 10 million Americans have osteoporosis, and 50% of women and 25% of men will have an osteoporotic fracture in their lifetime [1]. Osteoporotic fractures result in significant functional impairment, decreased quality of life, and increased mortality [2, 3]. After one year, 40% of hip fracture survivors are unable to walk independently, 80% can no longer perform activities such as shopping or driving, and approximately one third become permanent nursing home residents [3]. The impact of this major public health problem is expected to increase exponentially as the population ages.
The most widely prescribed medications used to treat osteoporosis are bisphosphonates. Bisphosphonates are antiresorptive agents which have been shown to prevent postmenopausal and glucocorticoid associated bone loss and to decrease the risk of vertebral and hip fractures in large randomized controlled trials by approximately 50% [4-9]. Apart from gastrointestinal adverse events, bisphosphonates are generally very well tolerated.
Teriparatide is the generic name for recombinant human parathyroid hormone [rhPTH (1-34)] which has recently become available for the treatment of patients with osteoporosis. Unlike the anti-resorptive agents, rhPTH (1-34) exerts its protective effect, in part, by stimulating bone growth. rhPTH (1-34) is seen as a breakthrough in treatment of osteoporosis, because it is the first Food and Drug Administration (FDA) approved agent available that stimulates bone growth. FDA approval of teriparatide was based on a double-blind controlled trial of teriparatide involving 1,637 postmenopausal women with prior vertebral fractures [10]. In this study the risk of new vertebral fractures was reduced by 65%. Vertebral fractures occurred in 14% of the women in the placebo group and in 5% of the women receiving rhPTH (1-34) [10]. The impact of rhPTH (1-34) on total non-vertebral fractures yielded a statistically significant relative risk reduction of 53% [10]. The main disadvantage related to rhPTH (1-34), apart from its cost, is that it must be administered by daily subcutaneous injections.
Adherence to treatment for osteoporosis is poor [11]. Given that patients' health beliefs are strongly related to adherence to medications [12], incorporation of patient preferences to maximize treatment efficacy is particularly important for this disease [13-17]. Moreover, some studies have shown that increased patient participation in medical decision-making may lead to improved adherences rates and outcomes [14, 16]. To the best of our knowledge, there have been no studies examining patients' preferences for rhPTH (1-34). The objective of this study was to determine how much benefit patients expect rhPTH (1-34) to confer before agreeing to perform daily subcutaneous injections.
2. Methods
2.1 Participants
Consecutive English speaking postmenopausal women undergoing bone densitometry in six centers serving the greater New Haven (Connecticut) area were asked whether they agreed to be contacted by a research assistant to learn more about, and potentially participate in, a study examining patients' opinions about medications for osteoporosis. Participants were asked to fill out a form indicating whether or not they wished to be contacted, and if yes to provide their phone number. A research assistant then telephoned all women agreeing to be contacted to explain the study in further detail, obtain consent and determine eligibility.
Postmenopausal women with osteoporosis [T score (at total hip or lumbar spine) at or below −2.5] and/or a Fracture Index Score ≥ 6 [21] were eligible to participate. Women with known secondary causes of osteoporosis, esophagitis, severe heartburn, the inability to sit upright for at least 30 minutes, or previous allergic reactions to bisphosphonates (ascertained by self-report) were excluded. These criteria were meant to exclude patients for whom bisphosphonates would not be a medically reasonable choice. The research protocol was approved by the Human Investigations Committee at our institution.
2.2 Preference Measurement
Participants first underwent a standardized educational session with the research assistant to briefly explain the pathophysiology of osteoporosis and its complications. The information presented to participants was based on patient information materials published by the National Osteoporosis Foundation. The educational session was performed to ensure that all participants had the same information available to them before performing the preference task.
Consenting participants completed an Adaptive Conjoint Analysis (ACA) questionnaire to determine their treatment preferences [18]. When faced with multiple alternatives, people make decisions by making trade-offs between the specific features of competing products. Conjoint analysis derives preferences by examining these trade-offs through a series of rating exercises, and subsequently determines which combination of features would be most preferred by each respondent.
There are several ways to collect data for conjoint analyses. ACA collects and analyzes preference data using an interactive computer program (Sawtooth Software ®). ACA is unique in that it uses an individual respondent's answers to update and refine questions through a series of paired-comparisons. The main advantage of ACA's interactive design is that it allows a large number of attributes to be evaluated without resulting in information overload or respondent fatigue [18]. Conjoint analysis has a strong theoretical basis and obtains high levels of internal consistency [19-24]. For example, in one study examining choices for prevention of osteoporosis where 95% of subjects were able to correctly identify a dominant alternative [25]. A recent study found that ACA accuracy in predicting choice ranged from 61% to 89% [26], and we have previously demonstrated that ACA preferences for medications which result in premature ovarian failure are significantly higher among women wanting more children compared to their counterparts [19]. ACA uses an interactive format that engages participants' attention and results in greater gains in knowledge compared to standard educational materials. In addition, ACA is administered by computer, minimizing interviewer biases and facilitating data collection and management. Because ACA can be programmed to present the outcomes in random order, it eliminates ordering effects [27].
ACA assumes that each treatment option is a composite of different characteristics. The four characteristics included in this study were: 1) route of administration, 2) absolute risk reduction of vertebral fractures over five years, 3) absolute risk reduction of hip fractures over five years, and 4) risk of adverse effects. Risk information was presented using natural frequencies and pictographs to facilitate communication of probabilistic data [28, 29]. Medication characteristics were first explained in detail to participants using lay terminology and then, because of space constraints, presented in abbreviated format in the computerized questionnaire.
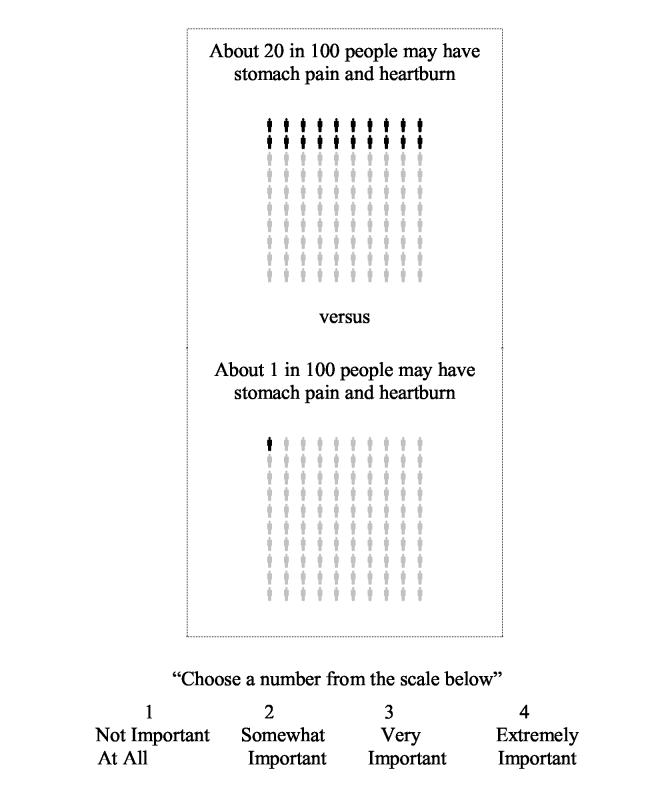
In this study, the ACA survey contained two sets of questions. First, respondents were asked to rate the importance of the difference between the highest and lowest estimate of each characteristic on a four point scale, thereby allowing ACA to learn enough about each respondent's values to construct initial utility estimates. In this context “utility” is a number that represents the value a respondent associates with a particular characteristic, with higher utilities indicating increased value.
For example:
“If two medications were acceptable in all other ways, how important would this difference be”
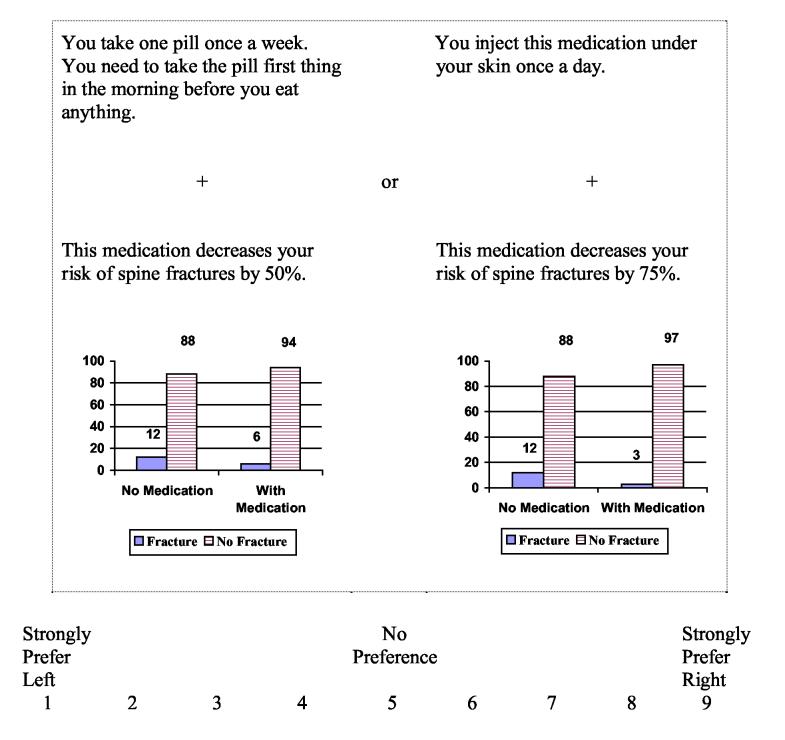
To refine respondents' utilities, respondents evaluated a series of paired concepts tailored to the patient's initial utility estimates. Each question involved choosing one option from a pair in which one is superior in one characteristic and the opposing option is superior in the other. ACA constructs pairs by examining all the possible ways the characteristics can be combined and then chooses pairs of options with similar utilities for which it expects respondents to be indifferent (based on previous responses).
For example:
“Which would you prefer?”
The program uses the information obtained from each paired comparison to update the estimates of each respondent's utilities and to select the next pair of options. Final utilities are generated using regression analysis [18].
We created two versions of the ACA questionnaire (high fracture risk: Fracture Index > 7, lower fracture risk: Fracture Index = 6 or 7), so that each patient was presented with individualized risk information. Estimates of risk were obtained using the Fracture Index scoring system developed by Black et al [30]. Patients were informed of their own risk after completing the Fracture Index Survey [30]. Participants completed the computer questionnaire with the aid of a research assistant when needed. Assistance from the research assistant was limited to reading the information presented on the screen and providing standardized explanations for the characteristics presented.
2.3 Covariates
Sociodemographic data and attitudes towards osteoporosis and its complications were collected by self-report in face-to face interviews with the research assistant. Perceived risk of future fracture over five years was coded on a five item response scale:“1 in 100 people like me”, “5 in 100 people like me”, “10 in 100 people like me”, “20 in 100 people like me”, and “30 in 100 people like me will have an osteoporotic fracture in the next five years”. Responses of “10 in 100 people like me” or more were, a priori, coded as having a high relatively higher perceived risk of fracture. Worry about developing a stooped posture and hip fracture were each evaluated using a seven item response scale ranging from “None of the time” to “All of the time”. Respondents stating that they were worried about either becoming stooped or having a hip fracture “A good bit of the time” or more were classified as being worried about future fractures.
2.4 Analyses
Preference data derived from ACA (version 3.0, Sawtooth Software, Inc., Sequim, WA) were imported into SAS (version 8.0) and merged with the patient characteristics data set.
ACA calculates a preliminary estimate of each respondent's utilities based on their initial ratings of the characteristics (i.e. the first set of questions described above). The utility estimates are then updated based on responses in the paired-comparison task using Bayesian analyses [18, 20]. At the end of the ACA task, the utility estimates are true least-squares. Details regarding the methods underlying these calculations are available at http://www.sawtoothsoftware.com/technicaldownloads.shtml#acatech.
Note that the participant does not evaluate treatment alternatives directly. Rather, the participant considers the trade-offs between conflicting characteristics. Answers to carefully selected patient-specific questions allow the investigator to infer values for specific treatment characteristics. These values are then used to predict which option most closely suits each patient's individual priorities.
We performed simulations based on women's values for route of administration, absolute reduction in risk of hip and vertebral fractures over five years and risk of adverse effects to predict each individual respondent's treatment choice. For each simulation, ACA predicts preferences based on the utilities derived from the conjoint questionnaire using least squares regression analysis [18, 20]. Given that bisphosphonates are the most widely prescribed medication for osteoporosis, we used preference for bisphosphonates as a reference point, and measured strength of preference for rhPTH (1-34) versus weekly oral bisphosphonates. We did not include monthly oral bisphosphonates because this option was not available at the time of the study. In the base case scenario, we modeled rhPTH (1-34) as being more effective than bisphosphonates (vertebral and hip fracture risk reduced by 50% for bisphosphonates and 75% for rhPTH (1-34) respectively). Although higher than that demonstrated in randomized controlled trials, a 75% risk reduction was chosen for rhPTH (1-34) to represent a meaningful increment in benefit. In the base case scenario, neither rhPTH (1-34) nor bisphosphonates were described as being associated with an increased risk of adverse events. We then performed sensitivity analyses to ascertain the influence of modifying the probability of benefit and risk of adverse events on treatment preference.
Associations between respondent characteristics and treatment preferences were examined using t-test and chi-square tests for continuous and categorical covariates respectively. Multivariate analyses were subsequently performed using multiple logistic regression.
3. Results
3.1 Participant Characteristics
The study sample included 183 women, mean age ± SD = 71 ± 9 years (range 46 to 90). The vast majority (94%) of the sample was white; 46% were married; and 67% had at least some college education. One hundred fifty-two (83%) women knew of bisphosphonates as a possible treatment option for osteoporosis, none were familiar with rhPTH (1-34), and none had talked about using an injectable medication with their physician prior to the study. Participant characteristics are further described in Table 1.
Table 1.
Participant Characteristics
| Characteristic | Number (Total = 185) |
|---|---|
| Age (mean ± SD, range) | 71 ± 9 (46-90) |
| Caucasian (%) | 174 (94) |
| Married (%) | 87 (47) |
| At least some college education (%) | 125 (68) |
| High Fracture Index (%) | 71 (38) |
| High perceived risk of fracture (%) | 47 (25) |
| Currently using bisphosphonates (%) | 106 (57) |
| Currently using rhPTH (1-34) (%) | 0 |
| Health status very good or excellent (%) | 91 (49) |
| Worried about developing a stooped posture at least a good bit of the time (%) | 51 (28) |
| Worried about having a hip fracture at least a good bit of the time (%) | 27 (15) |
| Previous vertebral fracture (%) | 15 (8) |
| Previous hip fracture (%) | 4 (2) |
3.2 Treatment Preferences
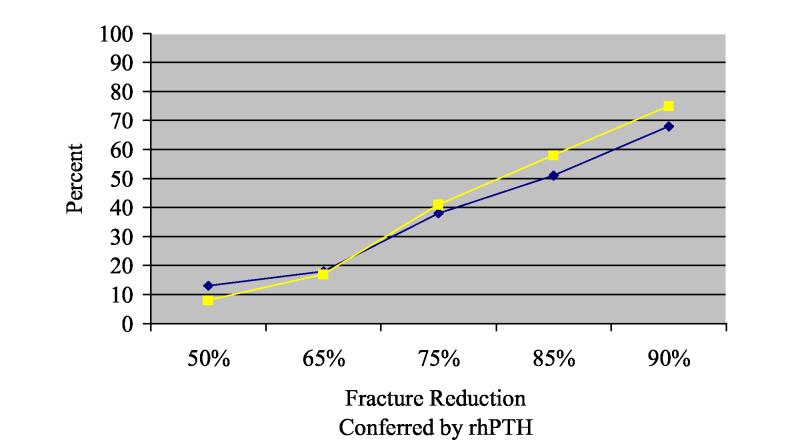
Overall, for the base case scenario in which rhPTH (1-34) was modeled as being 25% more effective than bisphosphonates in preventing both vertebral and hip fractures, 72 (39%) women preferred rhPTH (1-34) over weekly oral bisphosphonates. Treatment preferences for rhPTH (1-34) among women at high versus low risk for osteoporotic fractures did not differ (see Table 2). An increasing number of women (regardless of risk) preferred rhPTH (1-34) over bisphosphonates as the efficacy of teriparatide increased (see Figure 1). However, rhPTH (1-34) became the preferred treatment option for the majority of respondents only when it is described as having benefits far greater than expected based on results of randomized trials (Figure 1) [10, 31-33].
Table 2.
Percent of Respondents Preferring rhPTH (1-34) by Risk Group
| Low Risk (Fracture Index ≤ 7) N (%) | High Risk (Fracture Index > 7) N (%) | Chi-Square | P value | |
|---|---|---|---|---|
| Base Case | 45 (39) | 29 (41) | 0.03 | 0.9* |
Figure 1.
Percent of Women Preferring rhPTH (1-34) over Bisphosphonates as Benefit of rhPTH (1-34) is Increased
Legend:
Yellow Line: High Fracture Risk (Fracture Index Score = > 7)
Blue Line: Low Fracture Risk (Fracture Index = 6 or 7)
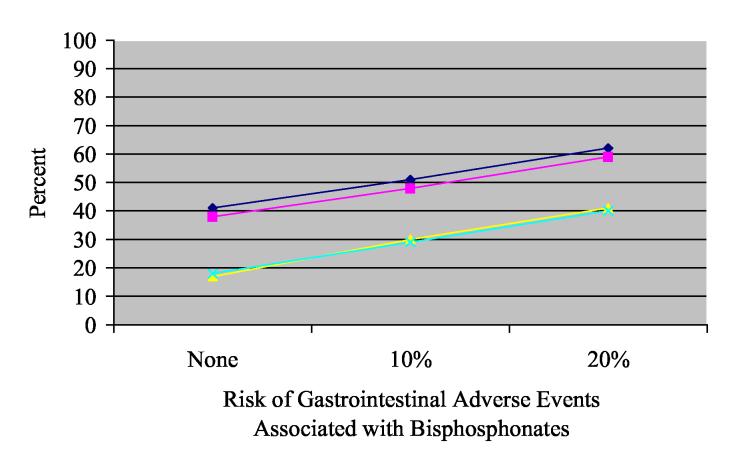
Preference for both treatment options as the risk of gastrointestinal adverse events associated with bisphosphonates is increased are shown in Figure 2. The reluctance of women to accept daily subcutaneous injections is further demonstrated in this figure, as most respondents continue to prefer bisphosphonates even when this option is described as having an increased risk of adverse events compared to rhPTH (1-34).
Figure 2.
Percent of Women Preferring rhPTH (1-34) over Bisphosphonates as Adverse Effects
Associated with Bisphosphonates are Increased
Legend:
Yellow Line: High Fracture Risk (Fracture Index = > 7) assuming rhPTH (1-34) is associated with a 65% reduction in risk of fractures.
Blue Line: Low Fracture Risk (Fracture Index = 6 or 7) assuming rhPTH (1-34) is associatedwith a 65% reduction in risk of fractures.
Green Line: High Fracture Risk (Fracture Index = > 7) assuming rhPTH (1-34) is associated with a 75% reduction in risk of fractures.
Pink Line: Low Fracture Risk (Fracture Index = 6 or 7) assuming rhPTH (1-34) is associated with a 75% reduction in risk of fractures.
3.3 Associations Between Participant Characteristics and Treatment Preferences
Bivariate associations between preference for rhPTH (1-34) and patient characteristics are shown in Table 3. There was no association between sociodemographic characteristics and preference for rhPTH (1-34) except for age. In this study, younger women were significantly more likely than older women to be willing to perform daily subcutaneous injections in exchange for improved benefits. Current use of bisphosphonates was inversely associated with preference for rhPTH (1-34). Preference for rhPTH (1-34) was also stronger among women with a relatively higher perceived risk of fracture and among women who worried more about having a fracture. However, there was no association between respondents' actual fracture risk and preference for rhPTH (1-34) (Table 3). Perceived fracture risk [Adjusted Odds Ratio (95% confidence interval) = 4.0 (1.8-8.9)] remained associated with preference for rhPTH (1-34) after controlling for the preceding covariates (Table 4).
Table 3.
Participant Characteristics and Preference for rhPTH (1-34): Bivariate Analyses
| Characteristic | Percent Preferring rhPTH (1-34) | Percent Not Preferring rhPTH (1-34) | Chi-Square Test | p value |
|---|---|---|---|---|
| Age ≥ 65 | 74 | 86 | 4.4 | 0.05 |
| Fracture Index > 7 | 39 | 37 | 0.03 | 0.8 |
| Some College | 69 | 67 | 0.1 | 0.7 |
| Married | 47 | 47 | 0.004 | 0.9 |
| Annual household income ≥ $40,000 | 72 | 77 | 0.8 | 0.4 |
| Health status very good or excellent | 40 | 55 | 3.7 | 0.05 |
| High perceived risk of fracture | 40 | 15 | 14.9 | 0.001 |
| Worried about vertebral fractures at least a good bit of the time | 35 | 22 | 3.5 | 0.06 |
| Worried about hip fractures at least a good bit of the time | 22 | 10 | 4.9 | 0.03 |
| Currently using bisphosphonates | 46 | 65 | 6.5 | 0.01 |
Table 4.
Participant Characteristics and Preference for rhPTH (1-34): Multivariate Analyses*
| Characteristic | Adjusted Odds Ratio (95% Confidence Interval) |
|---|---|
| Age ≥ 65 | 0.5 (0.2-1.1) |
| Health status very good or excellent | 0.8 (0.4-1.5) |
| High perceived risk of fracture | 3.8 (1.8-8.1) |
| Worried about vertebral fractures at least a good bit of the time | 1.2 (0.6-2.7) |
| Worried about hip fractures at least a good bit of the time | 1.8 (0.7-4.8) |
| Currently using bisphosphonates | 0.4 (0.2-0.8) |
Independent variables included in the model = age, health status, perceived risk of fracture, worry related to hip and vertebral fractures and current use of bisphosphonates.
4. Discussion and Conclusion
4.1 Discussion
In summary, we found that the majority of women participating in this study strongly preferred a once weekly oral medication over rhPTH (1-34). Based on currently available risk reduction rates, few women, regardless of fracture risk, would choose rhPTH (1-34) over other treatment options. Subjects at risk for future osteoporotic fractures were willing to take rhPTH (1-34), but most demanded efficacy advantages greater than that demonstrated in clinical trials to date [10, 31-33].
Although rhPTH (1-34) is generally reserved for patients at high risk for future fractures, in this study women at higher risk for fractures were not more willing to take rhPTH (1-34), regardless of benefit, compared to women at lower risk for fractures. However, women with a relatively higher perceived risk of future fracture were more willing to perform subcutaneous injections for added efficacy. This finding is consistent with previous studies demonstrating the strong influence of risk perception on healthcare beliefs and behaviors [34-37].
Women's preferences were based on trade-offs between medication characteristics and therefore were not biased by recognition of specific treatment options. Furthermore, participants held no preconceived opinions regarding rhPTH (1-34) since none were aware of rhPTH (1-34) as a possible treatment option and none of the women had discussed this option with their physician prior to participating in the study.
Numerous studies have demonstrated that conjoint analysis produces internally consistent responses, and that it is a reliable and valid method of measuring preferences [19, 21-24, 38]. Results from this study are consistent with previous studies demonstrating that patient preferences vary and frequently differ from physicians' practices and or guidelines [39-41]. Other strengths of this technique are the minimization of interviewer bias, the elimination of brand name or product recognition bias, and the ability to ensure that respondents evaluate all characteristics under consideration.
In view of the known difficulties associated with communicating probabilistic information, we tried to maximize understanding of risk magnitude using several strategies. We provided both numerical estimates (natural frequencies) as well as graphical representations of probability data. In addition, outcomes were provided for women both on and off medication and we used the same denominator throughout the survey.
Our results must be interpreted in view of the limitations of this study. We did not consider preferences for rhPTH (1-34) among women who “failed” bisphosphonates or other treatments, nor did we examine preferences for cyclic therapies since outcomes using this approach were not available at the time of the study. We could not include all medication characteristics, because this would have overly complicated the questionnaire. However, inclusion of additional adverse effects (such as the theoretical possibility of osteogenic sarcoma) and cost would be expected to further widen the gap between patient preferences for bisphosphonates over rhPTH (1-34). Many of the participants interviewed were already on treatment for osteoporosis, because we could not recruit sufficient numbers of treatment naïve women. In addition, most participants were Caucasian, female, and well-educated, thereby limiting the generalizability of the results.
There is a large literature describing the effects of risk perception on decision-making and choice behavior [34-37]. These studies demonstrate variable influence of risk perception on choice and patient behavior. This is especially true in health care where multiple factors, such as physicians' recommendations, strongly influence patients' decision-making [42]. This study adds to the current literature demonstrating the importance of perceived risk, or worry about specific risks, as an important determinant of patients' preferences and highlight the need for clinicians to be aware of patients' individual ‘health beliefs’ when discussing potential treatment options.
4.2 Conclusion
We conclude that few women would agree to take rhPTH (1-34) based on currently available outcome data and that treatment preferences in this population are more strongly related to perceived versus actual risk.
4.3 Practice Implications
Given the concerns regarding osteoporosis medication use in older adults with multiple co-morbidities, including adverse effects associated with polypharmacy, poor adherence, and costs, our results suggest that efforts towards development of novel therapeutics should incorporate patient preferences in order to ensure investment in options most likely to be acceptable to patients.
ACKNOWLEDGEMENTS
Dr. Fraenkel had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. We would like to thank Janet Mahoney (research assistant), the technicians at participating bone centers, and all the participants for their time and effort. Dr. Fraenkel is supported by the K23 Award AR048826-01 A1. This study was also funded by the Arthritis Foundation Clinical Science Grant. This work was presented in part at the American College of Rheumatology and Shared Decision-Making annual meetings.
Footnotes
Dr. Fraenkel is supported by the K23 Award AR048826-01 A1. This study was also funded by the Arthritis Foundation Clinical Science Grant. This work was presented in part at the American College of Rheumatology and Shared Decision-Making annual meetings.
REFERENCES
- 1.Black D. Report From the Fifth International Symposium on Recent Clinical Advances in Osteoporosis, International Symposium on Recent Clinical Advances in Osteoporosis. Honolulu, Hawaii: 2002. [Google Scholar]
- 2.Ben Sedrine W, Radican L, Reginster JY. On conducting burden-of-osteoporosis studies: a review of the core concepts and practical issues. A study carried out under the auspices of a WHO Collaborating Center. Rheumatology. 2001;40:7–14. doi: 10.1093/rheumatology/40.1.7. [DOI] [PubMed] [Google Scholar]
- 3.Cooper C. The crippling consequences of fractures and their impact on quality of life. Am J Med. 1997;103(2A):12S–19S. doi: 10.1016/s0002-9343(97)90022-x. [DOI] [PubMed] [Google Scholar]
- 4.Black DM, Cummings SR, Karpf DB, et al. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Lancet. 1996;348:1535–41. doi: 10.1016/s0140-6736(96)07088-2. [DOI] [PubMed] [Google Scholar]
- 5.Cummings SR, Black DM, Thompson DE, et al. Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures: results from the Fracture Intervention Trial. J Amer Med. 1998;280:2077–82. doi: 10.1001/jama.280.24.2077. [DOI] [PubMed] [Google Scholar]
- 6.Cummings SR, Karpf DB, Harris F, et al. Improvement in spine bone density and reduction in risk of vertebral fractures during treatment with antiresorptive drugs. Am J Med. 2002;112:281–9. doi: 10.1016/s0002-9343(01)01124-x. [DOI] [PubMed] [Google Scholar]
- 7.Ensrud KE, Black DM, Palermo L, et al. Treatment with alendronate prevents fractures in women at highest risk: results from the Fracture Intervention Trial. Arch Intern Med. 1997;157:2617–24. [PubMed] [Google Scholar]
- 8.Orwoll E, Ettinger M, Weiss S, et al. Alendronate for the treatment of osteoporosis in men. N Engl J Med. 2000;343:604–10. doi: 10.1056/NEJM200008313430902. [DOI] [PubMed] [Google Scholar]
- 9.Woolf AD, Akesson K. Preventing fractures in elderly people. Brit Med J. 2003;327:89–95. doi: 10.1136/bmj.327.7406.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Neer RM, Arnaud CD, Zanchetta JR, et al. Effect of parathyroid hormone (l-34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med. 2001;344:1434–41. doi: 10.1056/NEJM200105103441904. [DOI] [PubMed] [Google Scholar]
- 11.Solomon DH, Avorn J, Katz JN, et al. Compliance with osteoporosis medication. Arch Intern Med. 2005;165:2414–19. doi: 10.1001/archinte.165.20.2414. [DOI] [PubMed] [Google Scholar]
- 12.Horne R, Weinman J. Patients' beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47:555–67. doi: 10.1016/s0022-3999(99)00057-4. [DOI] [PubMed] [Google Scholar]
- 13.Conrad P. The meaning of medications: another look at compliance. Soc Sci Med. 1985;20:29–37. doi: 10.1016/0277-9536(85)90308-9. [DOI] [PubMed] [Google Scholar]
- 14.Greenfield S, Kaplan SH, Ware JE, Jr., Yano EM, Frank HJ. Patients' participation in medical care: effects on blood sugar control and quality of life in diabetes. J Gen Intern Med. 1988;3:448–57. doi: 10.1007/BF02595921. [DOI] [PubMed] [Google Scholar]
- 15.Oldridge NB. Future directions: what paths do researchers need to take? What needs to be done to improve multi-level compliance? In: Burke LE, Ocken IS, editors. Compliance in Health Care and Research. Futura; Armonk: 2001. [Google Scholar]
- 16.van Dam HA, van der Horst F, van den Borne B, Ryckman R, Crebolder H. Provider-patient interaction in diabetes care: effects on patients self-care and outcomes. Pt Educ Counsel. 2003;51:17–28. doi: 10.1016/s0738-3991(02)00122-2. [DOI] [PubMed] [Google Scholar]
- 17.Ward MM, Sundaramurthy S, Lotstein D, Bush TM, Neuwelt CM, Street RJ. Participatory patient-physician communication and morbidity in patients with systemic lupus erythematosus. Arthritis Rheum. 2003;49:810–18. doi: 10.1002/art.11467. [DOI] [PubMed] [Google Scholar]
- 18.Johnson RM. Adaptive Conjoint Analysis; Sawtooth Software Conference Proceedings; Ketchum, ID. 1987. [Google Scholar]
- 19.Fraenkel L, Bodardus S, Wittink DR. Understanding patient preferences for the treatment of lupus nephritis with adaptive conjoint analysis. Med Care. 2001;39:1203–16. doi: 10.1097/00005650-200111000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Green PE, Srinivasan V. Conjoint analysis in marketing: new developments with implications for research and practice. J Marketing. 1990;54:3–17. [Google Scholar]
- 21.Phillips KA, Maddala T, Johnson FR. Measuring preferences for health care interventions using conjoint analysis: an application to HIV testing. Health Serv Res. 2002;37:1681–705. doi: 10.1111/1475-6773.01115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ryan M, Farrar S. Using conjoint analysis to elicit preferences for health care. Brit Med J. 2000;320:1530–3. doi: 10.1136/bmj.320.7248.1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Singh J, Cuttler L, Mincheol S, Silvers JB, Neuhauser D. Medical decision making and the patient: understanding preference patterns for growth hormone therapy using conjoint analysis. Med Care. 1998;36:AS31–AS45. doi: 10.1097/00005650-199808001-00005. [DOI] [PubMed] [Google Scholar]
- 24.Wittink DR, Bergenstuen T. Forecasting with conjoint analysis. In: Armstrong JS, editor. Principles of forecasting: a handbook for researchers and practitioners. Kluwer Academic Publishers; Norwell, MA: 2001. [Google Scholar]
- 25.Fraenkel L, Constantinescu F, Oberto-Medina M, Wittink D. Women's preferences for prevention of bone loss. J Rheumatol. 2005;32:1086–92. [PubMed] [Google Scholar]
- 26.Beusterien KM, Dziekan K, Flood E, Harding G, Jordan JC. Understanding patient preferences for HIV medications using adaptive conjoint analysis: feasibility assessment. Value in Health. 2005;8:453–61. doi: 10.1111/j.1524-4733.2005.00036.x. [DOI] [PubMed] [Google Scholar]
- 26.Ryan M, McIntosh E, Shackley P. Methodological issues in the application of conjoint analysis in health care. Health Economics. 1998;7:373–8. doi: 10.1002/(sici)1099-1050(199806)7:4<373::aid-hec348>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 27.Gigerenzer G. Calculated Risks. Simon & Schuster; New York: 2002. [Google Scholar]
- 28.Rothman AJ, Kiviniemi MT. Treating people with information: an analysis and review of approaches to communicating health risk information. J Natl Cancer Inst Monographs. 1999;25:44–51. doi: 10.1093/oxfordjournals.jncimonographs.a024207. [DOI] [PubMed] [Google Scholar]
- 29.Black DM, Steinbuch M, Palermo L, et al. An assessment tool for predicting fracture risk in postmenopausal women. Osteoporosis Int. 2001;12:519–28. doi: 10.1007/s001980170072. [DOI] [PubMed] [Google Scholar]
- 30.Body JJ, Gaich GA, Scheele WH, et al. A randomized double-blind trial to compare the efficacy of teriparatide [recombinant human parathyroid hormone (1-34)] with alendronate in postmenopausal women with osteoporosis. J Clin Endocrinol Metab. 2002;87:4528–35. doi: 10.1210/jc.2002-020334. [DOI] [PubMed] [Google Scholar]
- 31.Lindsay R, Scheele WH, Neer R, et al. Sustained vertebral fracture risk reduction after withdrawal of teriparatide in postmenopausal women with osteoporosis. Arch Intern Med. 2004;164:2024–30. doi: 10.1001/archinte.164.18.2024. [DOI] [PubMed] [Google Scholar]
- 32.Sugiyama T, Tanaka H, Kawai S. Effects of parathyroid hormone and alendronate alone or in combination in osteoporosis. N Engl J Med. 2004;350:189–92. [PubMed] [Google Scholar]
- 33.Klos A, Weber EU, Weber M. Investment decisions and time horizon: Risk perception and risk behavior in repeated gambles. Management Sci. 2005;51:1777–90. [Google Scholar]
- 34.Lucidi F, Russo PM, Mallia L, Devoto A, Lauriola M, Violani C. Sleep-related car crashes: Risk perception and decision-making processes in young drivers. Accident Anal Prev. 2006;38:302–9. doi: 10.1016/j.aap.2005.09.013. [DOI] [PubMed] [Google Scholar]
- 35.Peters E, McCaul KD, Stefanek M, Nelson W. A heuristics approach to understanding cancer risk perception: Contributions from judgment and decision-making research. Ann Behav Med. 2006;31:45–52. doi: 10.1207/s15324796abm3101_8. [DOI] [PubMed] [Google Scholar]
- 36.Slovic P, Peters E, Finucane ML, MacGregor DG. Affect, risk, and decision making. Health Psychol. 2005;24:S35–S40. doi: 10.1037/0278-6133.24.4.S35. [DOI] [PubMed] [Google Scholar]
- 37.Bryan S, Buxton M, Sheldon R, Grant A. Magnetic resonance imaging for the investigation of knee injuries: an investigation of preferences. Health Economics. 1998;7:595–603. doi: 10.1002/(sici)1099-1050(1998110)7:7<595::aid-hec381>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 38.Montgomery AA, Fahey T. How do patients' treatment preferences compare with those of clinicians? Qual Health Care. 2001;10(suppl):i39–i43. doi: 10.1136/qhc.0100039... [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Spoorenberg A, van Tubergen A, Landewe R, et al. Measuring disease activity in ankylosing sponylitis: patient and physician have different perspectives. Rheumatology. 2005;44:789–95. doi: 10.1093/rheumatology/keh595. [DOI] [PubMed] [Google Scholar]
- 40.Suarez-Almazor ME, Conner-Spady B, Kendall CJ, Russell AS, Skeith K. Lack of congruence in the ratings of patients' health status by patients and their physicians. Med Decis Making. 2001;21:113–21. doi: 10.1177/0272989X0102100204. [DOI] [PubMed] [Google Scholar]
- 41.Gurmankin AD, Baron J, Hershey JC, Ubel PA. The role of physicians' recommendations in medical treatment decisions. Med Decis Making. 2002;22:262–71. doi: 10.1177/0272989X0202200314. [DOI] [PubMed] [Google Scholar]