Abstract
Medical practice encompasses a diverse spectrum of specialties. Factors that impact selection of clinical disciplines by young physicians may have recently evolved associated with changes in medical school demographics. We assessed whether physicians gravitate to certain practice specialties due to preexisting personality traits. The Neuroticism-Extraversion-Openness Personality Inventory Revised Test was administered prospectively to 130 first-year students the week before they began medical school. Scores for five traits (neuroticism, extraversion, openness, agreeableness, conscientiousness) were compared with the selection among nine medical residencies at the conclusion of medical school. Personality scores for medical students selecting psychiatry residencies showed greater degrees of neuroticism (P < 0.01) and openness (P < 0.03). Students electing family practice also deviated from other specialties, showing a lower degree of neuroticism (P < 0.03). Unexpectedly, personality traits in prospective surgical residents did not differ from those of students choosing nonsurgical residencies. Personality profiles present before medical school appear to predict the selection of some residencies and clinical specialties but not others.
Medicine is a heterogeneous profession in which a variety of clinical specialties are associated with differences in clinical environment, physician responsibility, and patient exposure (1–6). It perhaps follows intuitively that physicians practicing in certain disciplines may also share distinctive personality characteristics that differ from those demonstrated by their colleagues in other specialties. Indeed, previous studies have reported that personality profiles identifiable at entry to or during medical school may be predictive of, or associated with, the specialty ultimately selected by students (7–19). These observations have also promoted the notion that disciplines within the medical profession attract specific personality traits, which in turn are determinants of career choices.
However, in the 10 to 15 years that followed the publication of such data, the methodologies and measures available to assess personality have evolved. In addition, the demographics of medical students have changed considerably. For example, the number of women in medical school has greatly increased, and women now comprise approximately 50% of most classes. Financial demands, and incurred debt with the rising cost of medical education, may also ultimately dictate specialty choice. Further, students' perceptions of the lifestyle related to various medical specialties have changed, given their diverse urban and rural backgrounds, the changing public imagery of medicine, and the growing complexity of medical practice. Prior studies have suggested that variables as diverse as student academic standing and achievement in medical school, religious preference, family medical traditions, medical school curriculum, strong faculty mentors, and lifestyle considerations may play important roles in determining the choice of specialty. Many of these factors may have altered the landscape sufficiently to make personality factors less important in the selection of a medical specialty.
Therefore, it is of potential value to reexamine these issues to assess in a prospective fashion the relationship between the personality characteristics present just before medical studies begin and the type of residency program selected by these same students at the conclusion of medical school.
METHODS
Selection of study subjects
The test subjects comprised the entering first-year medical school class of Tulane University School of Medicine (New Orleans, Louisiana) in August 1999. The medical school assembles a diverse student body with respect to personality, experiences, and geographic origin, although a large proportion of students come from southeastern states. The Neuroticism-Extraversion-Openness Personality Inventory Revised Test (NEO PI-R) (20) was administered to 146 (96%) of the 152 medical students. Of these 146 students, 9 were not included in the analysis due to class attrition (e.g., school transfer or delayed graduation). For the remaining 137 students, medical specialty selection was obtained from the National Residency Matching Program as published by Tulane University (Table 1). For purposes of statistical power, only specialties chosen by ≥7 students were included in the analysis (excluding 7 other students). Therefore, the final study group comprised 130 students (74 men, 56 women), distributed among 9 medical specialties. The project was approved by the institutional review board of Tulane University School of Medicine.
Table 1.
Medical residencies selected by fourth-year students
| Specialty | n | Men:Women |
| Internal medicine | 30 | 15:15 |
| Surgery∗ | 24 | 16:8 |
| Pediatrics | 15 | 4:11 |
| Radiology | 14 | 11:3 |
| Anesthesiology | 12 | 10:2 |
| Family medicine | 12 | 8:4 |
| Psychiatry | 9 | 4:5 |
| Emergency medicine | 7 | 5:2 |
| Obstetrics-gynecology | 7 | 1:6 |
∗In addition to general surgery (n = 10), includes neurosurgery (n = 1), orthopedics (n = 6), otolaryngology (n = 4), ophthalmology (n = 2), and urology (n = 1).
Testing procedure
The test was administered during a single session as part of the student orientation activities and was supervised by the principal investigator (B.A.M.). Personalized identification numbers were used to protect anonymity and maintain test result confidentiality. Participants were debriefed regarding the implications and limitations of the personality inventory and were provided full disclosure of their test results.
About 4 years after administration of the personality test, the residency specialty selection of each participant was obtained. Based on the residency matching results, participants were assigned to one medical specialty category. In some cases, specialty categories with small numbers were combined; for example, subjects who chose the surgical subspecialties of neurosurgery, orthopedics, otolaryngology, ophthalmology, or urology were analyzed together with general surgery. For residencies in neurology (n = 1), dermatology (n =1), combined psychiatry and medicine (n = 1), and physical medicine and rehabilitation (n = 2), students were included for analysis in the internal medicine category.
Test inventory
The NEO PI-R form S English version test was used in this study (20). This personality test has been widely used in cardiovascular medicine and has been shown to have high reliability (21). The test is designed for adult subjects and requires approximately 1 hour for completion. It consists of 240 questions that assess general personality type, as characterized by five major domains: neuroticism, extraversion, openness, agreeableness, and conscientiousness (NEOAC) (Table 2). A domain is defined as one of these five personality traits, which taken together form the common thread of an individual's personality type. Internal consistency for each of the five domains—i.e., the degree to which different questions for a given domain measure the same construct—is 0.86 to 0.957. Retest reliability for the domains—i.e., the extent to which individuals approximate the same scores on two different occasions—is 0.86 to 0.917. Each of these domains is, in turn, composed of several specific intercorrelated traits, termed facets. A cluster of six specific personality facets comprises a personality domain (internal consistency = 0.56 to 0.81; retest reliability = 0.66 to 0.92).
Table 2.
Definition of personality traits analyzed in relation to medical specialty
| Personality domain | Definition | Facets |
| Neuroticism | General tendency to experience negative affects (e.g., fear, embarrassment, anger) in response to stress | Anxiety Angry hostility Depression Self-consciousness Impulsiveness Vulnerability |
| Extraversion | General sociability with a cheerful disposition and strong interest in enterprising occupations | Warmth Gregariousness Assertiveness Activity Excitement-seeking Positive emotions |
| Openness | General attentiveness to inner feelings, intellectual curiosity, and independence of judgment | Fantasy Aesthetics Feelings Actions Ideas Values |
| Agreeableness | A measure of interpersonal tendencies, assessing how an individual values different aspects of a relationship | Trust Straightforwardness Altruism Compliance Modesty Tender-mindedness |
| Conscientiousness | Management of impulses and desires with predisposed investment in planning, organizing, and carrying out tasks | Competence Order Dutifulness Achievement striving Self-discipline Deliberation |
Administration of the test and scoring were conducted in compliance with the inventory guidelines outlined in the NEO PI-R instructions. There are eight questions per facet, and answers to questions fall along a scale between “strongly agree” and “strongly disagree.” Respondent answers are awarded a numerical value, and these are summed, resulting in an overall facet score. Facet scores are, in turn, summed to obtain a given domain score.
Statistical analysis
To assess whether patterns of scores across the five personality trait domains (NEOAC) differed as a function of medical specialty, analysis of variance (ANOVA) was performed with the medical specialty representing the intersubject factor and scores on each of the five NEOAC categories representing the intrasubject factor. Also, one-way ANOVAs were conducted on specific personality dimensions, with the medical specialty the intersubject factor.
RESULTS
Group analysis
A mixed-model ANOVA showed a statistically significant overall relationship between the scores on the five personality trait domains and the nine medical specialties selected by students through the National Residency Matching Program (P = 0.02). Therefore, the distribution of the specialties selected by medical students was not random and deviated as a function of personality profile.
Individual medical specialty analysis
Psychiatry
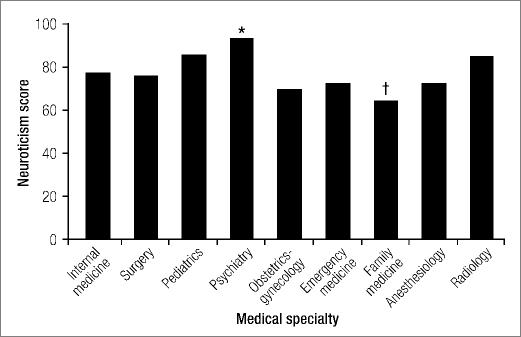
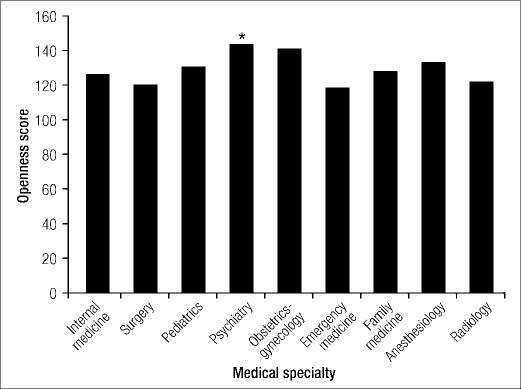
The specialty that deviated most with respect to overall pattern of NEOAC personality scores from the other medical disciplines analyzed was psychiatry (P < 0.01). Specifically, compared with other students, those choosing psychiatry showed significantly higher neuroticism (P < 0.01) (Figure 1) and openness (P < 0.03) (Figure 2). In addition, psychiatry students scored lower on extraversion than did those choosing other specialties, although this difference did not achieve statistical significance (P = 0.1). There were no discernable differences between students specializing in psychiatry and other disciplines with regard to agreeableness and conscientiousness (P > 0.05).
Figure 1.
Relationship between the nine medical specialties chosen by fourth-year students and their neuroticism personality score. ∗P < 0.01; †P < 0.03.
Figure 2.
Relationship between the nine medical specialties chosen by fourth-year students and their openness personality score. ∗P < 0.03.
Family practice
Students choosing family practice deviated from those selecting other medical specialties on overall NEOAC personality scores (ANOVA P = 0.05). In addition, compared with others, family medicine students scored particularly low in neuroticism (P < 0.03) (Figure 1). Students choosing family practice scored higher in agreeableness and conscientiousness than did those selecting other specialties, although these differences did not achieve statistical significance (P = 0.1).
Other specialties
None of the remaining seven clinical specialties demonstrated an overall personality profile that deviated significantly from the others. However, scores on certain specific personality traits did differ among the medical specialties. For example, students selecting internal medicine scored higher in agreeableness than did those selecting other specialties(P = 0.05). Students in surgery scored lower in openness compared with those in other specialties, although this analysis only achieved borderline significance(P = 0.06). There were no statistically significant differences with regard to personality traits between students selecting internal medicine and those selecting surgery.
In addition, students specializing in anesthesiology scored lower in conscientiousness than did other subjects (P = 0.01), and those selecting radiology scored lower in agreeableness, although only with borderline significance (P = 0.06).
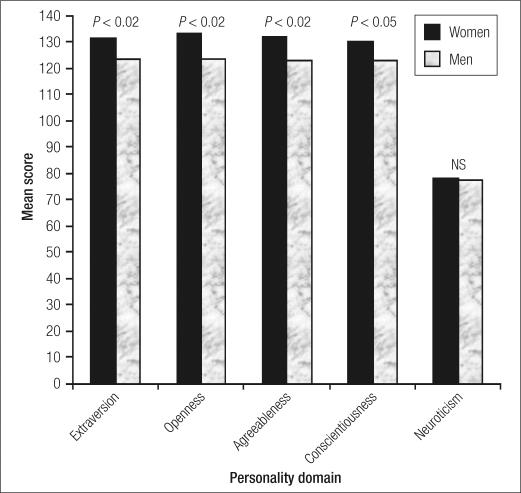
Gender
Significant differences by gender emerged for four of the five personality domains. Women scored higher than men, independent of specialty, in extraversion (P < 0.02), openness (P < 0.02), agreeableness (P < 0.02), and conscientiousness (P < 0.05) (Figure 3). There were no gender differences with regard to neuroticism.
Figure 3.
Relationship between mean personality score and gender with respect to the five personality domains.
DISCUSSION
The selection of a medical specialty is a profound decision that defines the professional career of a physician. However, the practice of medicine is extraordinarily diverse, including disciplines and lifestyles as varied as surgery, pediatrics, family practice, and radiology. Indeed, the spectrum of medical specialties available to medical students likely draws upon different attributes, motivations, and personality traits (7—18, 22—33).
In this study, we found evidence that certain personality traits, present even at the early juncture of exposure to medicine, were in fact associated with the ultimate decision to elect specialization in family practice and psychiatry. The personality traits associated with psychiatry and family practice intuitively correspond to results of prior reports and the perceptions and stereotypes traditionally attributed to practicing physicians in those specialties (7–9, 11, 34). However, it is also noteworthy that our data do not appear to support assumptions regarding the personality types associated with other medical specialties such as surgery (12, 31–33). For example, Zeldow and Daugherty (7–9) conducted a comprehensive analysis of the relationship between personality and medical specialty choice in the early 1990s and found significant linkage between a distinctive psychological profile and the selection of a surgical residency. Certainly, those data are consistent with the general stereotypic profile that persists among the general public and health care professionals—i.e., that the special requirements of surgery dictate a highly dominant and aggressive personality, low in inhibition(12, 31–33). Also, given the methodical and detail-oriented nature of surgical practice, we expected students choosing that residency to deviate from others in personality dimensions such as conscientiousness and perhaps extraversion. Nevertheless, despite our original intuition and the prevalent stereotypes, we found that prospective surgical residents entered medical school with personality profiles that were indistinguishable from the remainder of their class. These data suggest that personality profile is only one variable playing a role in specialty residency choices and that these decisions may ultimately be shaped by a myriad of other factors, either in the background of the students (such as temperament and character) or the experiences or events occurring during medical school (7, 18).
We found that the basic personality traits of women students differed distinctly from those of men at the onset of medical school (32). Their attributes of greater extraversion, openness, agreeableness, and conscientiousness are generally regarded as consistent with good medical practice. However, the present study sample was not of sufficient size to permit analysis of personality determinants of residency selection specifically with respect to gender. Even in those specialties dominated by women such as obstetrics-gynecology and pediatrics, female personality traits were not statistically significant determinants of medical specialty selection.
In the study design, we did not conduct intermediate personality assessments during the 4 years of medical school, in contrast to prior studies of students at Rush Medical School (9). However, the present study was not designed to assess the impact of medical education itself on personality dynamics.
Rather, we prospectively chose a strategy focused only on the extent to which basic personality traits evident prior to medical school influenced future choices in medicine.
Our findings raise the question of whether prospectively ascertained personality profiles could be of any practical value in medical student selection or career counseling. For example, personality profiles could possibly be of value in manpower planning by identifying students predisposed to enter certain specialties, such as family practice and psychiatry. When shortages exist in specific medical specialties, personality-based methodologies could influence the demographics of medical practice. Whether such considerations would prove to be practical, or even desirable, is presently unresolved.
References
- 1.Linn LS, Yager J, Cope D, Leake B. Health status, job satisfaction, job stress, and life satisfaction among academic and clinical faculty. JAMA. 1985;254(19):2775–2782. [PubMed] [Google Scholar]
- 2.Ramirez AJ, Graham J, Richards MA, Cull A, Gregory WM. Mental health of hospital consultants: the effects of stress and satisfaction at work. Lancet. 1996;347(9003):724–728. doi: 10.1016/s0140-6736(96)90077-x. [DOI] [PubMed] [Google Scholar]
- 3.Keller KL, Koenig WJ. Management of stress and prevention of burnout in emergency physicians. Ann Emerg Med. 1989;18(1):42–47. doi: 10.1016/s0196-0644(89)80309-9. [DOI] [PubMed] [Google Scholar]
- 4.McPherson S, Hale R, Richardson P, Obholzer A. Stress and coping in accident and emergency senior house officers. Emerg Med J. 2003;20(3):230–231. doi: 10.1136/emj.20.3.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bergus GR, Randall CS, Winniford MD, Mueller CW, Johnson SR. Job satisfaction and workplace characteristics of primary and specialty care physicians at a bimodal medical school. Acad Med. 2001;76(11):1148–1152. doi: 10.1097/00001888-200111000-00020. [DOI] [PubMed] [Google Scholar]
- 6.Linzer M, Konrad TR, Douglas J, McMurray JE, Pathman DE, Williams ES, Schwartz MD, Gerrity M, Scheckler W, Bigby JA, Rhodes E. Managed care, time pressure, and physician job satisfaction: results from the physician worklife study. J Gen Intern Med. 2000;15(7):441–450. doi: 10.1046/j.1525-1497.2000.05239.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zeldow PB, Devens M, Daugherty SR. Do person-oriented medical students choose person-oriented specialties? Do technology-oriented medical students avoid person-oriented specialties? Acad Med. 1990;65(9 Suppl):S45–S46. doi: 10.1097/00001888-199009000-00037. [DOI] [PubMed] [Google Scholar]
- 8.Zeldow PB, Preston RC, Daugherty SR. The decision to enter a medical specialty: timing and stability. Med Educ. 1992;26(4):327–332. doi: 10.1111/j.1365-2923.1992.tb00177.x. [DOI] [PubMed] [Google Scholar]
- 9.Zeldow PB, Daugherty SR. Personality profiles and specialty choices of students from two medical school classes. Acad Med. 1991;66(5):283–287. doi: 10.1097/00001888-199105000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Wasserman E, Yufit RI, Pollock GH. Medical specialty choice and personality: II. Outcome and postgraduate follow-up results. Arch Gen Psychiatry. 1969;21(5):529–535. doi: 10.1001/archpsyc.1969.01740230017003. [DOI] [PubMed] [Google Scholar]
- 11.Schumacher CF. Interest and personality factors as related to choice of medical career. J Med Educ. 1963;38:932–942. [PubMed] [Google Scholar]
- 12.Yufit RI, Pollock GH, Wasserman E. Medical specialty choice and personality. I. Initial results and predictions. Arch Gen Psychiatry. 1969;20(1):89–99. doi: 10.1001/archpsyc.1969.01740130091009. [DOI] [PubMed] [Google Scholar]
- 13.Kassebaum DG, Szenas PL. Factors influencing the specialty choices of 1993 medical school graduates. Acad Med. 1994;69(2):163–170. doi: 10.1097/00001888-199402000-00027. [DOI] [PubMed] [Google Scholar]
- 14.Martini CJM, Veloski JJ, Barzansky B, Xu G, Fields SK. Medical school and student characteristics that influence choosing a generalist career. JAMA. 1994;272(9):661–668. [PubMed] [Google Scholar]
- 15.Kassebaum DG, Szenas PL, Schuchert MK. Determinants of the generalist career intentions of 1995 graduating medical students. Acad Med. 1996;71(2):198–209. doi: 10.1097/00001888-199602000-00030. [DOI] [PubMed] [Google Scholar]
- 16.Mowbray RM, Davies B. Personality factors in choice of medical specialty. Br J Med Educ. 1971;5(2):110–117. doi: 10.1111/j.1365-2923.1971.tb02013.x. [DOI] [PubMed] [Google Scholar]
- 17.Gorenflo DW, Ruffin MT, IV, Sheets KJ. A multivariate model for specialty preference by medical students. J Fam Pract. 1994;39(6):570–576. [PubMed] [Google Scholar]
- 18.Vaidya NA, Sierles FS, Raida MD, Fakhoury FJ, Przybeck TR, Cloninger CR. Relationship between specialty choice and medical student tempera ment and character assessed with Cloninger Inventory. Teach Learn Med. 2004;16(2):150–156. doi: 10.1207/s15328015tlm1602_6. [DOI] [PubMed] [Google Scholar]
- 19.Babbott D, Baldwin DC, Jr, Killian CD, Weaver SO. Trends in evolution of specialty choice. Comparison of US medical school graduates in 1983 and 1987. JAMA. 1989;261(16):2367–2373. Erratum in JAMA 1990;263(6):815. [PubMed] [Google Scholar]
- 20.Costa PT, McCrae RR. The NEO Personality Inventory Manual. Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- 21.Costa PT, McCrae RR, Dembroski TM. Agreeableness vs. antagonism: explication of a potential risk factor for CHD. In: Siegman A, Dembroksi TM, editors. In Search of Coronary-Prone Behavior: Beyond Type A. Hillsdale, NJ: Lawrence Erlbaum Associates; 1989. pp. 41–63. [Google Scholar]
- 22.Siegman AW, Dembroski TM, Ringel N. Components of hostility and the severity of coronary artery disease. Psychosom Med. 1987;49(2):127–135. doi: 10.1097/00006842-198703000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Sliwa JA, Shade-Zeldow Y. Physician personality types in physical medicine and rehabilitation as measured by the Myers-Briggs Type Indicator. Am J Phys Med Rehabil. 1994;73(5):308–312. doi: 10.1097/00002060-199409000-00002. [DOI] [PubMed] [Google Scholar]
- 24.McGrath E, Zimet CN. Female and male medical students: differences in specialty choice selection and personality. J Med Educ. 1977;52(4):293–300. [PubMed] [Google Scholar]
- 25.Stilwell NA, Wallick MM, Thal SE, Burleson JA. Myers-Briggs type and medical specialty choice: a new look at an old question. Teach Learn Med. 2000;12(1):14–20. doi: 10.1207/S15328015TLM1201_3. [DOI] [PubMed] [Google Scholar]
- 26.Wallick MM, Cambre KM, Randall HM. Personality type and medical specialty choice. J La State Med Soc. 1999;151(9):463–469. [PubMed] [Google Scholar]
- 27.Tardiff K, Cella D, Seiferth C, Perry S. Selection and change of specialties by medical school graduates. J Med Educ. 1986;61(10):790–796. doi: 10.1097/00001888-198610000-00002. [DOI] [PubMed] [Google Scholar]
- 28.Walters GD. Academic and personality correlates of career indecision in medical students entering training. Med Educ. 1982;16(6):314–318. doi: 10.1111/j.1365-2923.1982.tb00943.x. [DOI] [PubMed] [Google Scholar]
- 29.Nuthalapaty FS, Jackson JR, Owen J. The influence of quality-of-life, academic, and workplace factors on residency program selection. Acad Med. 2004;79(5):417–425. doi: 10.1097/00001888-200405000-00010. [DOI] [PubMed] [Google Scholar]
- 30.Kluger MT, Laidlaw TM, Kruger N, Harrison MJ. Personality traits of anesthetists and physicians: an evaluation using the Cloninger Temperament and Character Inventory (TCI-125) Anesthesia. 1999;54(10):926–935. doi: 10.1046/j.1365-2044.1999.01112.x. [DOI] [PubMed] [Google Scholar]
- 31.Coombs RH, Fawzy FI, Daniels ML. Surgeons' personalities: the influence of medical school. Med Educ. 1993;27(4):337–343. doi: 10.1111/j.1365-2923.1993.tb00278.x. [DOI] [PubMed] [Google Scholar]
- 32.Gordin R, Jacobsen SJ, Rimm AA. Similarities in the personalities of women and men who were first-year medical students planning careers as surgeons. Acad Med. 1991;66(9):560. [PubMed] [Google Scholar]
- 33.Schwartz RW, Barclay JR, Harrell PL, Murphy AE, Jarecky RK, Donnelly MB. Defining the surgical personality: a preliminary study. Surgery. 1994;115(1):62–68. [PubMed] [Google Scholar]
- 34.Bruhn JG, Parsons OA. Medical student attitudes toward four medical specialties. J Med Educ. 1964;39:40–49. [PubMed] [Google Scholar]