Abstract
A 29 year old Thai woman presented with non-specific features and examination revealed left upper zone consolidation and hepatosplenomegaly. The initial clinical differential diagnosis included tuberculosis and melioidosis. She died four days after admission, while still under investigation. Postmortem examination revealed antibodies to human immunodeficiency virus, disseminated Penicillium marneffei infection, and Salmonella enteritidis infection. Penicillium marneffei is a well described AIDS defining pathogen in South East Asia but is very rare in the UK. Appropriate antifungal treatment may be associated with a successful outcome. Increased awareness of this clinical association may enable correct diagnosis in affected patients from South East Asia presenting within the UK.
Keywords: penicilliosis, salmonella, human immunodeficiency virus
A 29 year old Thai woman was admitted to hospital with a three week history of cough, lethargy and non-specific malaise eight months after moving to the UK from north east rural Thailand. No specific risk factors for human immunodeficiency virus (HIV) infection were elicited despite careful questioning related to sexual history. Examination revealed crusted facial skin lesions, decreased air entry within the left upper lung field, and hepatosplenomegaly. Initial investigations revealed anaemia, lymphopenia, mild neutrophilia, and abnormal liver function (haemoglobin concentration, 106 g/litre (normal range, 120–150); white blood cell count, 10.2 × 109/litre (normal range, 4.0–11.0); lymphocyte count 0.7 × 109/litre (normal range, 1.5–4.0); neutrophil count, 9.1 × 109/litre (normal range, 2.0–7.5); serum albumin, bilirubin, alanine transaminase, and alkaline phosphatase concentrations, 22 g/litre (normal range, 32–47), 31 μmol/litre (normal range, 0–17), 73 IU/litre (normal range, 5–42), and 969 IU/litre (normal range, 100–260), respectively). Chest radiology revealed left upper lobe consolidation and a prominent left hilum. Abdominal ultrasound examination confirmed hepatosplenomegaly and revealed retroperitoneal lymphadenopathy. Blood and urine culture revealed no bacterial growth. Sputum microscopy was negative for tumour cells and acid fast bacilli, whereas culture was negative for mycobacteria. Bronchoscopy two days after admission revealed no obvious cause for the chest abnormality. Bronchoalveolar lavage fluid microscopy revealed yeast organisms but microscopy and culture for mycobacteria was again negative.
Four days after admission her clinical state suddenly deteriorated and she died before further investigation or treatment was possible. A premortem blood film revealed a profoundly leucoerythroblastic picture consistent with severe sepsis, together with organisms within neutrophils (fig 1). The identity of the organisms was unknown at this time but the differential diagnosis included histoplasmosis and visceral leishmaniasis. Tuberculosis and melioidosis were also considered as possible co-infections.
Figure 1.
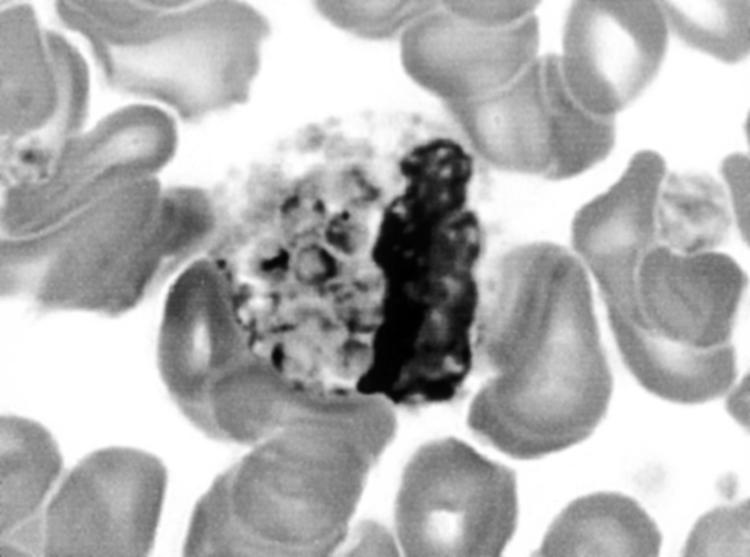
Blood smear showing Penicillium marneffei organisms within a monocyte. Giemsa stain; original magnification, ×1000.
Postmortem examination revealed a 50 mm area of consolidation with a central 15 mm cavity within the left upper lobe. The adjacent lung parenchyma showed patchy consolidation and the remaining lobes showed vascular congestion. Pronounced hepatosplenomegaly was present (liver, 3070 g; spleen, 1360 g) with no discrete lesions within either organ. Small volume lymphadenopathy was present at the hilum of the left lung, together with several para-aortic lymph nodes measuring up to 20 mm across. The entire colon contained multiple discrete apthous ulcers. The remainder of the gastrointestinal tract and major organs were macroscopically normal.
Postmortem histology revealed numerous budding yeast forms within alveolar macrophages in the left lung and within phagocytic cells in dilated hepatic sinusoids (fig 2), spleen, lymph nodes, bone marrow, renal interstitium, and arachnoid mater.
Figure 2.
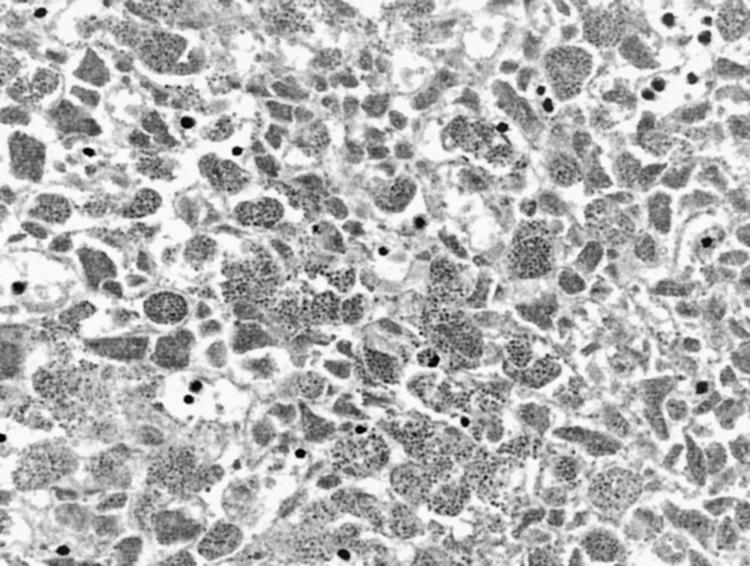
Histological section of liver showing expansion of sinusoids with numerous Penicillium marneffei organisms. Haematoxylin and eosin stain; original magnification, ×400.
Tests for anti-HIV antibody in serum obtained after death were positive (Vidas positive and HIV-1 Serodia positive). Salmonella enteritidis was cultured from the blood, spleen, bone marrow, and cerebrospinal fluid, whereas a fungus subsequently identified as Penicillium marneffei was cultured from the lung and bone marrow and seen within the cerebrospinal fluid. The fungus seen within the bronchoalveolar lavage fluid was also subsequently identified as P marneffei. Microscopy and culture of cerebrospinal fluid and lung tissue for mycobacteria was negative.
DISCUSSION
Salmonella enteritidis is a relatively common pathogen with a wide geographical distribution among HIV positive patients, which may result in gastroenteritis, widespread infection, and septicaemia in HIV positive individuals.1
Penicillium marneffei, a dimorphic fungus, is a common AIDS defining pathogen among HIV infected individuals in Southeast Asia and South China. Within Thailand, the organism is most common within the north of the country.2 Penicilliosis occurring beyond this locality is rare and is associated with HIV infection and a history of origin from or travel to endemic areas.3 Disseminated infection occurs in susceptible patients, including papular skin lesions, hepatosplenomegaly mimicking visceral leishmaniasis (rare in Thailand), and tuberculosis-like cavitating pulmonary infection.4 Diagnosis requires culture of the organism from skin aspirates, blood, sputum, or fine needle aspirate/biopsy material.4 In the appropriate clinical context, the identification of organisms in a peripheral blood film is highly suggestive of disseminated P marneffei infection.5 Systemic antifungal treatment with amphotericin B and itraconazole may result in clinical response.4 The clinical course in our case suggests that, although HIV infection and disseminated penicilliosis would account for the steady decline in the patient's health and would have soon proved fatal, the sudden dramatic collapse and death was probably the result of the development of the S enteritidis Gram negative septicaemia.
“This case highlights the occurrence of an infectious disease that is extremely rare in the UK but endemic in the patient's native country”
HIV infection was considered as a possibility soon after the patient's admission to hospital. However, formal HIV counselling would have been required before the test and counselling staff were not immediately available. Therefore, the patient's sudden decline and death occurred before an HIV test could be performed. Biopsy of the skin lesions was also planned but could not be performed for the same reason.
Take home messages.
Clinicians should be aware that Penicillium marneffei infection is common among human immunodeficiency virus infected individuals in Southeast Asia and South China
This is particularly important because appropriate antifungal treatment can be successful even in disseminated penicilliosis
This case highlights the occurrence of an infectious disease that is extremely rare in the UK but endemic in the patient's native country. Increased awareness of P marneffei as a pathogen in this clinical setting will prompt clinicians and pathologists to arrange appropriate diagnostic investigations, enabling correct diagnosis and differentiation from conditions such as visceral leishmaniasis and histoplasmosis. This is particularly important in the light of reported successful treatment even in disseminated penicilliosis.
Acknowledgments
We thank the Biomedical Imaging Department at Southampton General Hospital for their assistance with preparation of the images for this manuscript.
Abbreviations
HIV
human immunodeficiency virus
REFERENCES
- 1.Levine WC, Buehler JW, Bean NH, et al. Epidemiology of nontyphoidal Salmonella bacteremia during the human immunodeficiency virus epidemic. J Infect Dis 1991;164:81–7. [DOI] [PubMed] [Google Scholar]
- 2.Vanittanakom N, Sirisanthana T. Penicillium marneffei infection in patients infected with human immunodeficiency virus. Curr Top Med Mycol 1997;8:35–42. [PubMed] [Google Scholar]
- 3.Peto TE, Bull R, Millard PR, et al. Systemic mycosis due to Penicillium marneffei in a patient with antibody to human immunodeficiency virus. J Infect 1988;16:285–90. [DOI] [PubMed] [Google Scholar]
- 4.Duong TA. Infection due to Penicillium marneffei, an emerging pathogen: review of 155 reported cases. Clin Infect Dis 1996;23:125–30. [DOI] [PubMed] [Google Scholar]
- 5.Supparatpinyo K, Sirisanthana T. Disseminated Penicillium marneffei infection diagnosed on examination of a peripheral blood smear of a patient with human immunodeficiency virus infection. Clin Infect Dis 1994;18:246–7. [DOI] [PubMed] [Google Scholar]


