Abstract
Aims: To document demography, changing workload patterns, job satisfaction, morale, and prevalence of stress and psychological morbidity among UK consultant medical microbiologists and virologists.
Method: A questionnaire survey of all identified UK practising consultant medical microbiologists and virologists (n= 464).
Results: Among 367 respondents (79%), there were 33 virologists and at least 89 single handed consultants. Over half the respondents (58%) were working a 1 : 1 or 1 : 2 on call rota during the week and a similar proportion (51%) at weekends. Of all consultants (including those working part time), 56% were working more than 48 hours weekly. Working more than 48 hours weekly, and being on call 1 : 1 or 1 : 2 at weekends, were both independently associated with increased psychological morbidity. Those on call 1 : 1 or 1 : 2 at weekends were also more likely to have low or very low morale. Female consultants were more likely to have higher stress scores. More than half of the respondents (208 of 363; 57%) were making active financial provision to retire early, and 198 of 363 (55%) did not intend to work beyond the age of 60.
Conclusions: The long hours worked by many consultant microbiologists and virologists are in breach of the European Working Time Directive and are associated with a higher degree of psychological morbidity. For most consultants, the frequency of on call commitments is demanding and job satisfaction and morale have deteriorated. Urgent action is needed, particularly to support those working more than 48 hours each week and those on call at weekends 1 : 1 or 1 : 2. However, a major expansion of the consultant establishment cannot be achieved rapidly, and will be slowed further if early retirements become more frequent.
Keywords: medical microbiology, virology, workload, stress, workforce planning
For some years there has been concern over workplace stress among senior doctors in the UK.1–4 A recent report concluded that without urgent remedial action the National Health Service (NHS) could find itself with a deeply demoralised consultant workforce, with increasing numbers of consultants seeking early retirement or alternative employment.5
Workload in microbiology laboratories has grown steadily over the past 30 years6 (and unpublished Public Health Laboratory Service (PHLS) data). The range and complexity of work undertaken by consultant medical microbiologists and virologists has risen faster still, with increasing requirements for sophisticated clinical services allied to demands for greater input into infection control, antimicrobial prescribing, audit, and management.
“A recent report concluded that without urgent remedial action the NHS could find itself with a deeply demoralised consultant workforce, with increasing numbers of consultants seeking early retirement or alternative employment”
Despite these pressures, over the period 1987 to 1997, the numbers of consultant microbiologists and virologists rose by only 12.5%, compared with much larger percentage rises in other specialties—ranging from 27% in general and specialist medicine to 105% in accident and emergency medicine, and including general surgery and urology, anaesthetics, diagnostic radiology, care of the elderly, orthopaedic surgery, and paediatrics (UK Department of Health's Medical and Dental Workforce Census).
In our study, a questionnaire was distributed to all identified practising UK medical microbiologists and virologists seeking information on personal circumstances, workload, departmental resources, job satisfaction, morale, stress, and psychological wellbeing. The questionnaire was endorsed by the Association of Clinical Pathologists (ACP), the Royal College of Pathologists (RCPath), and the Association of Medical Microbiologists (AMM). Here, we describe the questionnaire survey, the principal findings, and the implications for the profession.
METHODS
Identification of microbiologists
Consultant medical microbiologists and virologists were identified from datasets of the RCPath, the ACP, the AMM, and the PHLS, by enquiry of all PHLS regional epidemiologists and of knowledgeable individuals within NHS regions.
The questionnaire
The questionnaire comprised six sections:
personal details and details of current appointment
departmental workload and resources
personal workload
job satisfaction and workload pressures
indices of stress
indices of psychological morbidity.
Questions on stress were based closely on those used in a 1995 survey of NHS consultants in Scotland7 and adapted for microbiologists. Psychological morbidity was assessed through the 12 item version of the General Health Questionnaire, a widely accepted screen in occupational settings.8, 9 Analysis of psychological morbidity was based on the numbers of respondents scoring 4 or more (out of a possible 12).
A pilot distribution of a draft questionnaire to all relevant consultants in the PHLS south west group permitted minor modifications before the main distribution in June 1999 to all identified practising consultant medical microbiologists and virologists in the UK. Although anonymised, each questionnaire included a unique reference number, permitting non-responders to be sent a second questionnaire. At all times, the study organisers remained unaware of the identity of the respondents.
Data entry, validation, and analysis
Data were entered using Epi-Info version 6.10 A check file was used to avoid data entry errors. In the sections on stress and psychological morbidity, a small number of missing values were imputed by best subset regression. Data were analysed using Stata version 6 (Intercooled Stata 6.0 for Windows 98/95/NT).
Single handed consultants were provisionally identified as those who cited a consultant establishment figure for their laboratory of 1.0 whole time equivalent or less and those who were without an associate specialist, clinical assistant, or consultant clinical scientist colleague. These individuals were sent a further letter, requesting them to confirm their status as single handed practitioners.
Statistical methods
Single variable analysis of job satisfaction, morale, and psychological morbidity was performed using the χ2 test and, for stress, one way analysis of variance was used. The risk factors considered were age (≤ 39, 40–49, 50–59, > 60 years), sex (male, female), average weekly hours worked (≤ 48 hours, ≥ 49 hours), virologist (yes, no), hospital (teaching, district general hospital (DGH) plus other), single handed (yes, no), head of department (yes, no), frequency of weekend on call (1 : 1 or 1 : 2, 1:3 or less often), and employment status (full time, part time).
To estimate the independent association of each possible risk factor, a logistic regression analysis was conducted for psychological morbidity. The most simple adequate model was selected by a backwards stepwise procedure. Likelihood ratio tests were used to test significance. Risk ratios were estimated using the “log” link function.
RESULTS
We identified 464 practising consultant medical microbiologists and virologists in the UK. Three hundred and sixty seven completed questionnaires were received, giving a response rate of 79%. Most respondents answered most questions. Where individuals did not respond to particular questions and their answers could not be imputed they were excluded from those analyses. For example, some respondents did not specify the type of hospital at which they worked, or whether they were employed as a microbiologist or virologist. Of 98 letters dispatched to provisionally identified single handed consultants, replies were received from 91 (93%).
Details of respondents and their current appointments
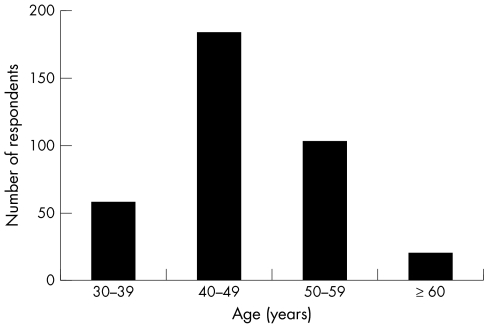
There was a predominance of men (224 of 359; 62%), particularly in the older age groups. Figure 1 shows the numbers of consultants by age. The age distributions of consultant medical microbiologists and virologists were similar. Two hundred and thirty seven (65%) were employed by NHS trusts, 92 by the PHLS, and 37 by universities and other employers. Most respondents (340 of 365; 93%) were in full time employment. Forty three respondents (12%) held combined appointments. There were 33 specialist virologists (9%).
Figure 1.
Age of respondents.
Departmental workload and resources
Most respondents (219 of 366; 60%) worked in DGHs, and almost all the remainder (138 of 366; 38%) worked in teaching hospitals. One fifth (78 of 367; 21%) of consultants worked in laboratories located on more than one site.
A third (113 of 356; 32%) of respondents, including eight of 29 virologists, reported their total consultant establishment (including their own post) as 1.0 whole time equivalent or less. Of these, 98 were sent a second letter. Of 91 who replied, 89 confirmed that they were single handed and two were no longer single handed.
Numbers of specimens processed annually by laboratories varied from under 50 000 to more than 400 000. Eighteen of 33 virologists responded to the question on population served, and of these, 10 worked in departments serving populations of up to 750 000; the remaining eight worked in departments serving populations ranging from one to three million people.
A fifth (70 of 357; 20%) of respondents did not have personal secretarial support. A further 22 did not have a personal secretary, but had secretarial support available within the department.
Personal workload
Table 1 details personal workload, on call commitments, and workload trends.
Table 1.
Personal workload, on call commitments, workload trends
| Microbiologists | Virologists | Total | ||||||||||
| DGH (excl. “Other*”) | Teaching hospital | |||||||||||
| n | N | (%) | n | N | (%) | n | N | (%) | n | N | (%) | |
| Head of department or head of section | 172 | 208 | 83 | 63 | 98 | 64 | 23 | 33 | 70 | 273 | 356 | 77 |
| Infection control doctor | 170 | 213 | 80 | 62 | 101 | 61 | 5 | 33 | 15 | 249 | 365 | 68 |
| Other managerial or professional role | 80 | 208 | 38 | 51 | 97 | 53 | 13 | 31 | 42 | 154 | 354 | 44 |
| Saturday a.m. in lab 1:1 or 1:2 | 90 | 205 | 44 | 9 | 100 | 9 | 2 | 30 | 7 | 101 | 352 | 29 |
| Sunday a.m. in lab 1:1, 1:2, 1:3, or 1:4 | 36 | 186 | 19 | 23 | 98 | 23 | 2 | 29 | 7 | 61 | 329 | 19 |
| First on call during week 1:1 or 1:2 | 172 | 211 | 82 | 14 | 98 | 14 | 10 | 29 | 34 | 204 | 354 | 58 |
| First on call at weekends 1:1 or 1:2 | 147 | 208 | 71 | 8 | 79 | 10 | 7 | 28 | 25 | 170 | 331 | 51 |
| Cover >1 acute hospital when on call | 97 | 211 | 46 | 68 | 99 | 69 | 20 | 28 | 71 | 194 | 356 | 54 |
| Weekly hours >48 (excluding on call) | 102 | 206 | 50 | 67 | 101 | 66 | 19 | 30 | 63 | 197 | 353 | 56 |
| Weekly hours >5 years ago | 109 | 157 | 69 | 48 | 71 | 68 | 14 | 23 | 61 | 179 | 263 | 68 |
| Compared with 5 years ago, more time spent on | ||||||||||||
| Clinical microbiology | 133 | 205 | 65 | 45 | 100 | 45 | 20 | 32 | 63 | 205 | 354 | 58 |
| Management | 167 | 203 | 82 | 75 | 100 | 75 | 26 | 32 | 81 | 285 | 353 | 81 |
| Research and development | 38 | 198 | 19 | 29 | 101 | 29 | 14 | 33 | 42 | 87 | 349 | 25 |
| Infection control | 157 | 204 | 77 | 70 | 100 | 70 | 15 | 31 | 48 | 253 | 353 | 72 |
| Teaching | 84 | 203 | 41 | 51 | 101 | 51 | 21 | 33 | 64 | 165 | 354 | 47 |
*Other, N=9.
DGH, district general hospital; N, total number; n, number answering “yes”.
Job satisfaction, morale, workload pressures, and retirement planning
Table 2 gives details of current levels and trends of job satisfaction and morale, and details of retirement planning. More than half the respondents (208 of 363; 57%) reported making active financial provision to retire early, with similar proportions in all age ranges except those aged 60 years and over. Of the 362 for whom a retirement age could be deduced, 15 (4%) cited 54 years or less, 91 (25%) an age of 55–59 years, and 92 (25%) cited 60 years. Only nine (2%) cited 61–64, and the remaining 155 (43%) were making no financial provision to retire early. Thirty three per cent (19 of 57) of those aged 30–39 and 24% (45 of 184) of those aged 40–49 planned to retire at age 55 or earlier (p = 0.23).
Table 2.
Job satisfaction and morale
| Microbiologists | Virologists | Total | ||||||||||
| DGH (excl. “Other*”) | Teaching hospital | |||||||||||
| n | N | (%) | n | N | (%) | n | N | (%) | n | N | (%) | |
| Job satisfaction now | ||||||||||||
| High/very high | 88 | 213 | 41 | 51 | 102 | 50 | 18 | 33 | 55 | 165 | 366 | 45 |
| Low/very low | 36 | 213 | 17 | 16 | 102 | 16 | 5 | 33 | 15 | 60 | 366 | 16 |
| Job satisfaction compared with 5 years ago | ||||||||||||
| Better/much better | 44 | 209 | 21 | 23 | 100 | 23 | 11 | 33 | 33 | 86 | 360 | 24 |
| Worse/much worse | 103 | 209 | 49 | 51 | 100 | 51 | 15 | 33 | 45 | 176 | 360 | 49 |
| Morale now | ||||||||||||
| High/very high | 52 | 214 | 24 | 31 | 102 | 30 | 10 | 33 | 30 | 99 | 367 | 27 |
| Low/very low | 68 | 214 | 32 | 20 | 102 | 20 | 8 | 33 | 24 | 101 | 367 | 28 |
| Morale compared with 5 years ago | ||||||||||||
| Better/much better | 30 | 208 | 14 | 20 | 98 | 20 | 6 | 31 | 19 | 62 | 355 | 17 |
| Worse/much worse | 121 | 208 | 58 | 56 | 98 | 57 | 16 | 31 | 52 | 202 | 355 | 57 |
| Contemplated early retirement as a result of changes in the NHS in last 5 years | 105 | 171 | 61 | 45 | 79 | 57 | 10 | 23 | 43 | 167 | 284 | 59 |
| Making financial plans to retire early | 125 | 210 | 60 | 60 | 102 | 59 | 15 | 33 | 45 | 208 | 363 | 57 |
*Other, N=9.
DGH, district general hospital; N, total number; n, number answering “yes”.
Most respondents (290 of 359; 81%) reported that recent changes in the NHS had led to an increase in their hours at work, a decrease in leisure time (287 of 357; 80%), and a decrease in the quality of their home life (222 of 350; 63%); 139 of 347 (40%) had noted an increase in the strain on their marriage or personal relationships.
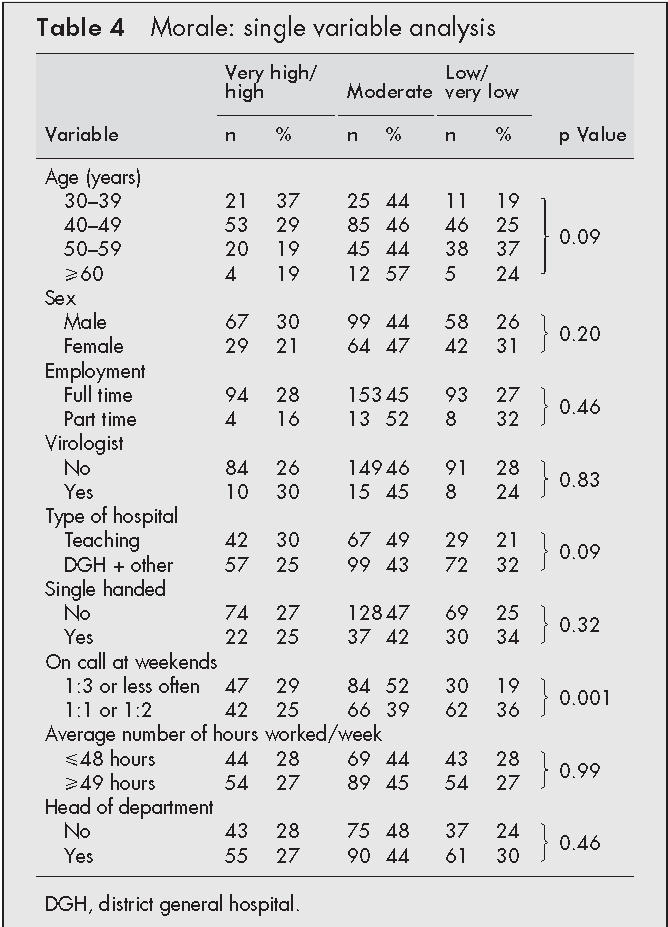
Tables 3 and 4 give details of single variable analyses of job satisfaction and morale. Of the variables considered, there was only one significant association, namely that morale was lower in those more frequently on call at weekends. Of those on call at weekends 1 : 3 or less frequently, 19% had low or very low morale, whereas 36% of those on call at weekends 1 : 1 or 1 : 2 had low or very low morale (p = 0.001).
Table 3.
Job satisfaction: single variable analysis
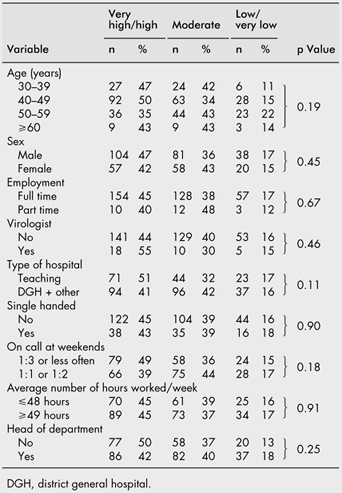
Table 4.
Morale: single variable analysis
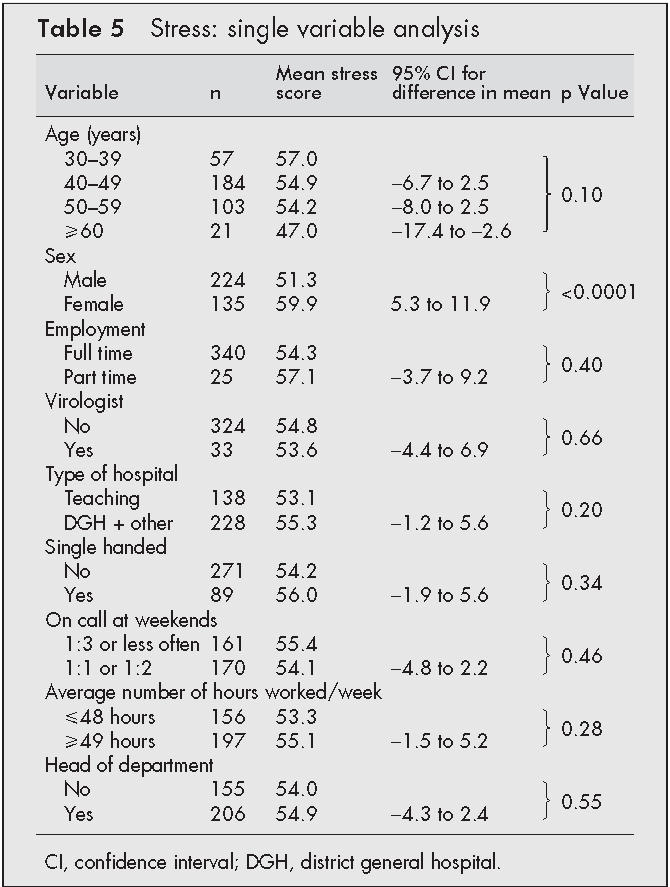
Stress
The sex of the individual was the only significant variable (p < 0.0001; table 5). Other than lower scores in those aged 60 or more, there were no pronounced differences in stress scores between any of the other age groups. Those reporting low or very low job satisfaction had higher mean stress scores than those with high or very high job satisfaction (63 v 50; p < 0.00005).
Table 5.
Stress: single variable analysis
Psychological morbidity
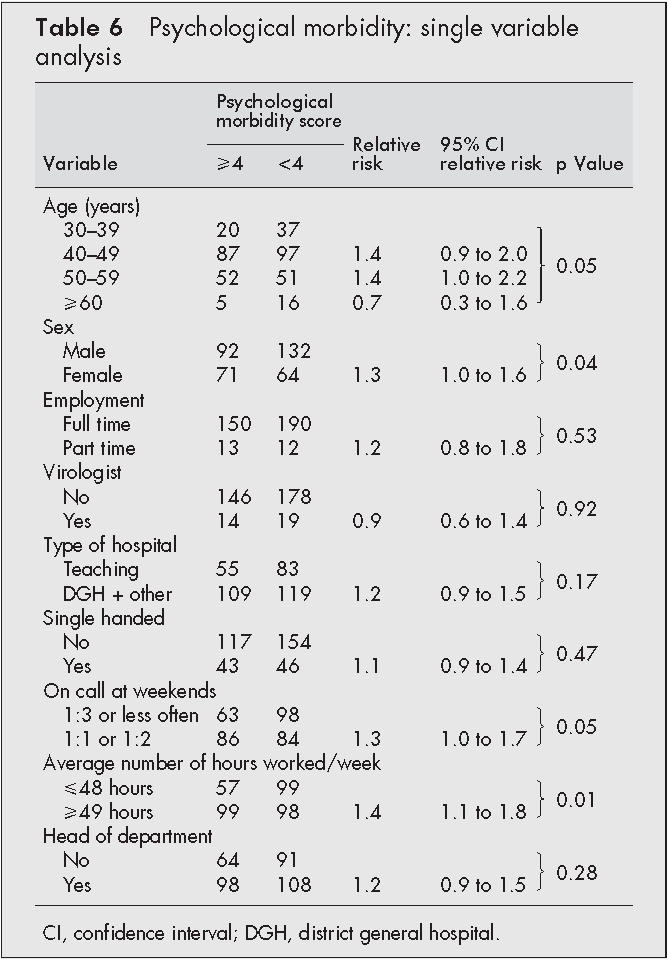
The proportion of microbiologists with a morbidity score of 4 or more was 45% (164 of 367; 95% confidence intervals (CI), 40% to 50%). The greatest contributor to psychological morbidity was “feeling constantly under strain”.
Single variable analysis showed that women and those working long hours were significantly more likely to have higher morbidity scores. Psychological morbidity also increased with age, but dropped considerably in the small numbers of respondents aged 60 years or more. Those with 1 : 1 or 1 : 2 weekend on call commitments were also more likely to have higher morbidity scores (table 6). Those reporting low or very low job satisfaction had higher morbidity scores than those reporting high or very high job satisfaction (80% v 23%; p < 0.00005).
Table 6.
Psychological morbidity: single variable analysis
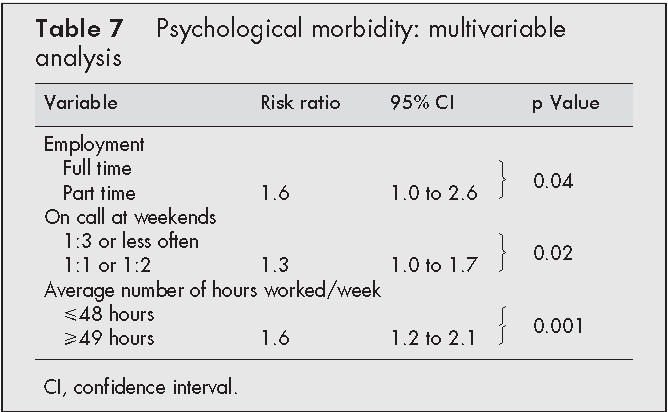
Multivariable analysis showed that working a weekly average of more than 48 hours (adjusted risk ratio, 1.6; 95% CI, 1.2 to 2.1; p = 0.001), and being on call at weekends 1 : 1 or 1 : 2 (adjusted risk ratio, 1.3; 95% CI, 1.0 to 1.7; p = 0.02) were independently associated with higher psychological morbidity (table 7). With adjustment for these factors, there was no evidence of higher psychological morbidity among older consultants or female consultants.
Table 7.
Psychological morbidity: multivariable analysis
DISCUSSION
The identification of all consultant medical microbiologists and virologists in the UK proved challenging. Reconciliation of our various data sources probably gave the most complete dataset currently available in the UK. The 464 confirmed practising consultants we identified underestimates the total numbers because the questionnaire was not sent to consultants in posts known to have purely managerial or academic content. The 79% response rate to the questionnaire gave confidence in the validity of the results.
The preponderance of male respondents was not surprising, but there was a welcome trend towards sex equality among younger consultants. As expected, most respondents worked in DGHs. Single handed consultants made up approximately a quarter of the total. The possibility that this group may have been more likely to respond cannot be excluded. Single handed practitioners have particularly onerous on call commitments, and are likely to need support to meet the increasing demands of continuing professional development.
Personal workload was generally high. In addition to clinical responsibilities, many consultants were carrying out infection control doctor duties or additional managerial roles, or both. More than half of the respondents (56%) reported working in excess of 48 hours each week on average, with a smaller group (17%) reporting working 60 or more hours each week. Such long working hours may threaten health, and are in breach of the European Working Time Directive.
“More than half of the respondents reported working in excess of 48 hours each week on average, with a smaller group (17%) reporting working 60 or more hours each week”
Despite generally high workload, job satisfaction and morale appear to have held up surprisingly well, but the deterioration in both over the past five years is consistent with other NHS consultant groups, and may explain the substantial numbers of microbiologists now considering, or actively planning, early retirement. With increasing numbers of consultants now planning to retire at 60, or in many cases at age 55, microbiology and virology workforce planning assumptions must be reviewed urgently.
The use of standardised assessment tools that generated numerical scores for stress and psychological morbidity permitted consultant medical microbiologists and virologists to be compared with other groups of UK doctors. The mean stress score among about 350 Scottish consultants in 1995 was 42.8.7 Taking only the 21 questions used in our study, the mean score of the Scottish consultants would have been approximately 44.5, significantly lower than the mean score of 54.5 for microbiologists and virologists in this survey (p < 0.00005). Although direct comparisons are difficult because of small variations in the phrasing and number of questions, in addition to the time interval between the two surveys, the size of the difference suggests that microbiologists are more stressed.
A 1995 survey of psychological morbidity in four groups of NHS consultants11 (gastroenterologists, surgeons, radiologists, and oncologists) revealed that 27% had a morbidity score of 4 or more, significantly lower than the 45% of microbiologists in our survey (risk ratio, 1.7; 95% CI, 1.4 to 1.9; p < 0.00005). Again, although direct comparisons are difficult because of the slight variations in questions used and in the time interval between the surveys, the substantial difference in proportions between the two groups suggests that in microbiologists there is a greater prevalence of psychological morbidity.
Take home messages.
Many consultant microbiologists and virologists work long hours, which is in breach of the European Working Time Directive and is associated with a higher degree of psychological morbidity
The frequency of on call commitments has increased for most consultants and job satisfaction and morale have deteriorated in the past five years
Urgent action should be taken, particularly to support those with the highest workload, although a major expansion of the consultant establishment cannot be achieved rapidly, and will be slowed further if early retirements become more frequent
In most comparisons, stress scores were not significantly different, although female consultants were significantly more likely to have higher stress scores. This association could not be explained by chance or by any of the other variables considered. Female consultants may have greater domestic commitments and may experience more logistic difficulty in meeting both these and their professional commitments.
Greater differences between groups were seen with respect to psychological morbidity. It was not surprising that those working a 1 : 1 or 1 : 2 weekend on call rota had higher psychological morbidity scores than those on call less frequently. About 50% of consultants have such heavy weekend on call commitments, and this group was estimated to be about 30% more likely to suffer from psychological morbidity, other factors being the same. DGH consultants were considerably more likely to be on call 1 : 1 or 1 : 2. In addition, those working an average of 48 hours or more each week had a higher psychological morbidity than those working fewer hours. About 50% of consultants work such long hours, and this group was estimated to be about 60% more likely to suffer from psychological morbidity, other factors being the same.
Only 7% of consultants reported working part time. Working part time was independently associated with higher psychological morbidity. Part time consultants very rarely work long hours and are less frequently on call at weekends; they were estimated to be moderately more at risk of psychological morbidity than full time consultants (table 6). The reason for this association was not clear.
Neither working regularly at two or more sites, nor the type of employer (NHS, PHLS, university, or “other”) was significantly associated with any of the outcome measures (job satisfaction, morale, stress, or psychological morbidity).
The questionnaire responses confirmed anecdotal evidence of rising workload, demanding on call commitments, and declining job satisfaction and morale among consultant medical microbiologists and virologists. Of particular concern were the substantial numbers of single handed practitioners, the numbers of consultants working average weekly hours in excess of the European Working Time Directive, and the numbers in all age groups planning early retirement. These issues will impact cumulatively on workforce planning. However, any major expansion of the consultant body appears unachievable, at least in the short term, owing to the paucity of training posts and possible adverse effects on recruitment resulting from the erosion of academic medical microbiology and virology. In the short term, it will be important for consultant microbiologists and virologists to work as efficiently and effectively as possible, to consider greater use of scientists and nurse practitioners, and to prepare well argued business cases for new consultant appointments to support those in the most hard pressed posts.
Acknowledgments
We thank Dr N Kapur for assistance with questionnaire design, Dr K Scott (Treasurer, Association of Clinical Pathologists) for financial support, Professor R MacSween (President, Royal College of Pathologists), and Professor M Emmerson (President, Association of Medical Microbiologists) for endorsement of the questionnaire, and administrative and technical staff of Gloucester PHL for preparing and distributing the questionnaires, and entering and validating data. Not least, we thank all the consultant medical microbiologists and virologists who took the time to complete and return the questionnaire.
Abbreviations
ACP, Association of Clinical Pathologists
AMM, Association of Medical Microbiologists
CI, confidence interval
DGH, district general hospital
NHS, National Health Service
PHLS, Public Health Laboratory Service
RCPath, the Royal College of Pathologists
REFERENCES
- 1.British Medical Association. Stress and the medical profession. London: British Medical Association, 1992.
- 2.Anon. Burnished or burnt out: the delights and dangers of working in health. Lancet 1994;344:1583–4. [PubMed] [Google Scholar]
- 3.Caplan R. Stress, anxiety and depression in hospital consultants, general practitioners, and senior health managers. BMJ 1994;309:1261–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blenkin H, Deary I, Sadler A, et al. Stress in NHS consultants. BMJ 1995;310:534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Allen I, Hale R, Herzberg J, et al. Stress among consultants in North Thames. London: Policy Studies Institute and University of London, 1999.
- 6.Audit Commission. The pathology services—a management review. London: HMSO, 1991.
- 7.Agius RM, Blenkin H, Deary IJ, et al. Survey of perceived stress and work demands of consultant doctors. Occup Environ Med 1996;53:217–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bank M, Clegg C, Jackson P, et al. The use of the general health questionnaire as an indication of mental health in occupational settings. Journal of Occupational Psychology 1980;53:187–94. [Google Scholar]
- 9.Goldberg D, Williams P. A user's guide to the General Health Questionnaire. Berkshire, UK: NFER-Nelson Publishing Co, 1988.
- 10.Dean AG, Dean JA, Coulumbier D, et al. Epi-Info version 6: a word-processing, database, and statistics program for epidemiology on microcomputers. Atlanta: Centers for Disease Control and Prevention, 1994.
- 11.Ramirez AJ, Graham J, Richards MA, et al. Mental health of hospital consultants: the effects of stress and satisfaction at work. Lancet 1996;347:724–8. [DOI] [PubMed] [Google Scholar]