Abstract
The causal role of human papillomavirus infections in cervical cancer has been documented beyond reasonable doubt. The association is present in virtually all cervical cancer cases worldwide. It is the right time for medical societies and public health regulators to consider this evidence and to define its preventive and clinical implications. A comprehensive review of key studies and results is presented.
Keywords: human papillomavirus, cervical cancer, causality, review
SUMMARY
During the 1990s, epidemiological studies, supported by molecular technology, provided evidence on the causal role of some human papillomavirus (HPV) infections in the development of cervical cancer. This association has been evaluated under all proposed sets of causality criteria and endorsed by the scientific community and major review institutes. The finding is universally consistent, and to date there are no documented alternative hypotheses for the aetiology of cervical cancer.
HPV has been proposed as the first ever identified, “necessary cause” of a human cancer. In practical terms, the concept of a necessary cause implies that cervical cancer does not and will not develop in the absence of the persistent presence of HPV DNA.
Cervical cancer is still the second most common cancer in women worldwide, although it is a theoretically preventable disease.
In developed parts of the world, and in populations where cytology based programmes are established, it would be beneficial to add HPV testing to the screening protocol. HPV testing was shown by several studies, including one randomised trial, to be of help in solving the ambiguous cases generated by cytology reading.
In populations where cytology programmes are either not in place or are not efficient, HPV testing should now be considered and evaluated as an alternative test for primary screening.
Prevention of exposure to high risk HPV types by vaccination may prove to be the most efficient and logistically feasible preventive intervention for cervical cancer.
At this stage of development, regulatory agencies are requested to evaluate the scientific evidence and weigh its implications in relation to costs, public health investments, and policy. This is a subjective evaluation that could be guided by a careful description of the most relevant studies and findings.
INTRODUCTION
A major discovery in human cancer aetiology has been the recognition that cervical cancer is a rare consequence of an infection by some mucosatropic types of HPV. In public health terms, this finding is equally important as the discovery of the association between cigarette smoking and lung cancer, or between chronic infections with hepatitis B virus (HBV) or hepatitis C virus and the risk of liver cancer. Moreover, as in the HBV disease model, intense efforts are currently going into the development and testing of vaccines that may prevent the relevant HPV infections, and presumably, cervical cancer.
By the year 2000, the epidemiological evidence included a large and consistent body of studies indicating, beyond any reasonable doubt, strong and specific associations relating HPV infections to cervical cancer. The observations have been reported from all countries where investigations have taken place. Studies include prevalence surveys, natural history investigations, case–control studies and, more recently, a randomised intervention trial. Natural history and follow up studies have clearly shown that HPV infection preceded the development of cervical cancer by several years and confirmed that sexual transmission is the predominant mode of HPV acquisition. These studies satisfied, in biological terms, the long known clinical and epidemiological observations that cervical cancer displayed the profile of a sexually transmitted disease (STD). Case–control studies, case series, and prevalence surveys have unequivocally shown that HPV DNA can be detected in adequate specimens of cervical cancer in 90–100% of cases, compared with a prevalence of 5–20% in cervical specimens from women identified as suitable epidemiological controls.
The association has been recognised as causal in nature by several international review parties since the early 1990s, and the claim has been made that this is the first necessary cause of a human cancer ever identified.
The implications of the recognition that, in the absence of viral DNA, cervical cancer does not develop, are of considerable practical importance. On the one hand, the concept of risk groups comes into focus. High risk women can now be sharply redefined as the group of persistent HPV carriers. Operatively, this represents substantial progress from previous versions of the high risk group that identified women by their exposure to a constellation of ill defined factors (low socioeconomic status, high number of sexual partners, smoking, use of oral contraceptives, history of STDs, and any combination of the above). Most of these factors are now viewed either as surrogates of HPV exposure or as relevant cofactors given the presence of HPV DNA. On the other hand, if indeed HPV is a necessary cause of cervical cancer, the implication is that specific preventive practices targeting some putative non-HPV related cervical cancer cases are no longer justified. Finally, technology is now available to screen HPV DNA positive women in the general population. Therefore, the final consideration on the nature of the association between HPV and cervical cancer is of considerable public health relevance. Research at the population level has largely accomplished its task by providing an exhaustive body of evidence. It is now time for public health institutions to evaluate these achievements, consider the costs and benefits involved, and apply this knowledge to their guidelines, recommendations, and policy.
HISTORICAL OVERVIEW
Research in relation to the aetiology of cervical cancer has made substantial progress in the past two decades, both in scientific and operational terms. For decades, the epidemiological profile of women with cervical cancer was recognised as suggestive of a sexually transmitted process, and several infectious agents were proposed over the years including syphilis, gonorrhea, and type 2 herpes simplex virus (HSV-2).
The development of technology to test for the presence of HPV DNA in cellular specimens in the early 1980s and the multidisciplinary collaboration within the field made possible the establishment of a definite aetiological role for HPV in cervical cancer. Evidence is also accumulating for HPV involvement in a considerable proportion of cancers of the vulva, vagina, anal canal, perianal skin, and penis. The association of HPV with cervical cancer has provided the background and the justification for improving screening programmes and for developing HPV vaccines.
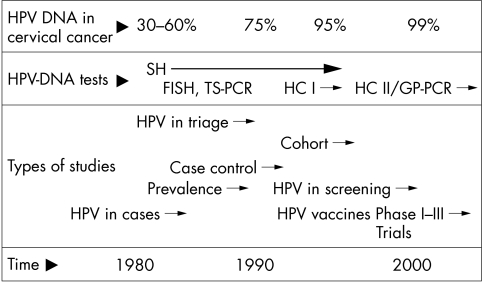
Figure 1 is a schematic view of the time scale of this dynamic process. It includes an indication of the results obtained as technology evolved in sensitivity expressed as the per cent of cervical cancer cases that were found to contain viral DNA. The figure also indicates the types of HPV tests that were predominantly used and an estimate of the periods in which the key types of studies were initiated.
Figure 1.
Evolution of epidemiological research on human papillomavirus (HPV) and cervical cancer in the past two decades. FISH, filter in situ hybridisation; GP-PCR, general primer PCR; HC I–II, hybrid capture first and second generation; PCR, polymerase chain reaction; SH, Southern blot hybridisation; TS-PCR, type specific PCR.
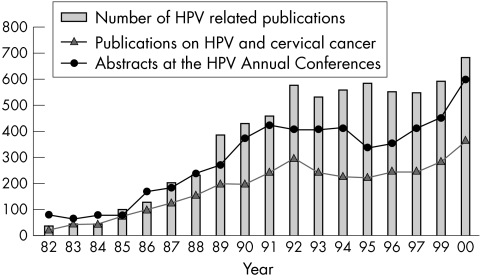
Figure 2 displays the approximate number of scientific papers identified by Medline searches on HPV and on HPV and cervical cancer, and the number of research abstracts presented at the major annual papillomavirus conferences (http://www.ipvsoc.org). The 1980s generated a rapidly increasing number of publications on HPV DNA prevalence in cervical cancer and reports on validation of the available detection methods. The 1990s produced the key results of case–control and cohort studies, and beginning in the late 1990s there was an increasing number of publications on the clinical uses of HPV testing in screening and triage.
Figure 2.
Scientific publications on human papillomavirus (HPV) identified by Medline and the number of research abstracts presented at the annual Papillomavirus International Conferences.
CAUSALITY CRITERIA IN HUMAN CANCER RESEARCH
Epidemiological studies are essential to establish the association between risk factors and cancer and to qualify the nature of the association. Traditionally, these include case series, case–control studies, cohort studies, and intervention studies.
Comparisons of exposure between patients with cervical cancer and their relevant controls were initially established using questionnaires. Most studies conducted before the availability of HPV DNA detection systems identified as key risk factors several variables related to the sexual behaviour of the women and of their sexual partners. The most frequently reported risk factors included the number of sexual partners, an early age at first intercourse, or any previous STD.1
Once the relevant biomarkers were validated, in this case the presence of HPV DNA in exfoliated cervical cells, it became possible to advance over questionnaire based studies and establish biologically sound comparisons between patients and controls. In epidemiological terms, these comparisons would analyse cervical cells from women with cervical cancer and from otherwise comparable women without cervical cancer (case–control studies), or from cohorts of women tested for viral DNA (cohort studies). To characterise the link between HPV and invasive cervical cancer, case–control studies proved to be the key study design and the only ones ethically acceptable in human populations. Typically in such a study and at the time of fieldwork, controls are selected to match the age distribution of the cases and, as much as possible, the general characteristics of the cases (place of residence, socioeconomic status, health plan, etc). To characterise the association, all study participants are requested to comply with a questionnaire to assess their individual exposure to any known or suspected risk factor for the disease. The information is then used to estimate the odds ratios (ORs) of disease related to any given exposure. Multivariate analyses have the ability to compare (through statistical adjustment) strictly equivalent groups of women in relation to any of the exposures of interest. The adjusted differences (ratios) in the prevalence in HPV markers between cases and controls are then obtained after having eliminated the effects of any other differences in exposure. Likewise, comparisons of cases and controls in relation to other variables of interest will provide estimates of the relevance of other factors (oral contraceptives (OCs) or smoking) and identify the variables that merely reflect HPV exposure (surrogate variables).
When the technology to detect HPV DNA in samples of DNA extracted from exfoliated cervical cells became available, it was relatively easy to show that most of the sexual behaviour variables were in fact surrogate measures of HPV exposure, reflecting the predominant pathway of acquisition of HPV. As methods became more sensitive, the parameters that merely expressed the probability of HPV (or any other STD) infection, such as number of sexual partners, became statistically irrelevant.2–5
Causality in public health requires a judgment based on scientific evidence from human and experimental (animal) observations. As such, only the latter may benefit from the most stringent criteria of causality; that is, the repeated induction of the disease by exposure to the relevant agent(s) compared with the “spontaneous” occurrence of the same disease in unexposed and yet comparable groups of animals. All causal associations of human cancers have been recognised based on educated judgment of the results of epidemiological studies at the level already available for HPV and cervical cancer. Final proof can only be confirmed by intervention (preventive) trials, in which a reduction of the disease burden (incidence or mortality) is observed following the introduction of a preventive practice in strictly controlled conditions. These studies typically include as controls populations to whom the existing standard of preventive care is being offered.
Table 1 displays some of the criteria that have been proposed to evaluate the nature of the associations encountered by epidemiological studies. This is particularly relevant when causality is being proposed because, as a consequence, preventive or clinical recommendations are made.
Table 1.
Epidemiological considerations important for causal inference
| Lilienfeld (1959)6 | Sartwell (1960)7 | Hill (1965)8 | Surgeon General (1964)9 and Susser (1973)10 | MacMahon and Pugh (1970)11 | IARC (1995)12 |
| Magnitude of effect | Strength of association | Strength of association | Strength/magnitude of association | Strength/magnitude of association | Strength of association |
| Consistency | Replication | Consistency | Consistency | Consistency | Consistency |
| Specificity | Specificity | Specificity | |||
| Temporality | Temporality | Temporality | Temporality | Temporality | |
| Dose response | Dose response | Biological gradient | Dose response | Dose response | Dose response |
| Biological mechanism | Biological plausibility | Biological mechanisms | Mechanisms | ||
| Biological reasonableness | Biological coherence | Biological coherence | Consonance with existing knowledge | ||
| Experimentation evidence | Experimental (intervention) | Experimental (intervention) | Experimental | ||
| Analogy | |||||
| Exclusion of alternative explanations |
Adapted from Weed 1995.13
In addition to the criteria listed in table 1, some additional contributions might be worth discussing. In 1976, Evans reviewed the history of the causality criteria in infectious disease models and adapted the early postulates of Henle-Koch to both the viral origin of acute diseases and to the relation between viral infections and cancer.14 The human models that inspired most of the latter included two examples: Epstein-Barr virus (EBV) infections and Burkitt's lymphoma, and HSV-2 viral infections and cervical cancer. The technology that was discussed was largely based on antibody detection and the studies involved were seroepidemiological surveys and case–control studies. Antibody measurements were the methods of choice for the assessment of exposure. Evans proposed a unified scheme for causation that included most of the criteria mentioned in table 1.14 In 1976, Rothman15 introduced the concepts of “necessary and sufficient causes”. This model is useful to accommodate the growing evidence of the multifactorial origin of human cancer in many instances. Finally, several authors have defined criteria to evaluate the findings of molecular technology that provided the basis of the studies of HPV and cervical cancer.16,17
Because of its wider acceptance, we will discuss in detail the criteria proposed by Hill, and its version adopted by the International Agency for Research on Cancer (IARC) monograph programme, in addition to the model on necessary and sufficient causes proposed by Rothman in 1995.18
In brief, the criteria proposed by Hill8 as summarised by Rothman19 include the following:
Hill suggested that the following aspects of an association should be considered when attempting to distinguish causal from non-causal associations: (1) strength, (2) consistency, (3) specificity, (4) temporality, (5) biological gradient, (6) plausibility, (7) coherence, (8) experimental evidence, and (9) analogy.
Strength
By “strength of association”, Hill means the magnitude of the ratio of incidence rates. Hill's argument is essentially that strong associations are more likely to be causal than weak associations because if they were the result of confounding or some other bias, the biasing association would have to be even stronger and would therefore presumably be evident. Weak associations, on the other hand, are more likely to be explained by undetected biases. Nevertheless, the fact that an association is weak does not rule out a causal connection.
Consistency
Consistency refers to the repeated observation of an association in different populations under different circumstances.
Specificity
The criterion of specificity requires that a cause should lead to a single effect, not multiple effects. However, causes of a given effect cannot be expected to be without other effects on any logical grounds. In fact, everyday experience teaches us repeatedly that single events may have many effects.
Temporality
Temporality refers to the necessity that the cause should precede the effect in time. The temporality of an association, is a sine qua non: if the “cause” does not precede the effect that is indisputable evidence that the association is not causal.
Biological gradient
Biological gradient refers to the presence of a dose–response curve. If the response is taken as an epidemiological measure of effect, measured as a function of comparative disease incidence, then this condition will ordinarily be met.
Plausibility
Plausibility refers to the biological plausibility of the hypothesis, an important concern but one that may be difficult to judge
Coherence
Taken from the Surgeon General's report on Smoking and Heath (1964)9: “The term coherence implies that a cause and effect interpretation for an association does not conflict with what is known of the natural history and biology of the disease.”
Experimental evidence
Such evidence is seldom available for human populations. In human data, the experimental criterion takes the form of preventive interventions and explores whether there is evidence that a reduction in exposure to the agent is associated with a reduction in risk.
Analogy
The insight derived from analogy seems to be handicapped by the inventive imagination of scientists, who can find analogies everywhere. Nevertheless, the simple analogies that Hill offers—if one drug can cause birth defects, perhaps another can also—could conceivably enhance the credibility that an association is causal.
As is evident, these nine aspects of epidemiological evidence offered by Hill to judge whether an association is causal are saddled with reservations and exceptions; some may be wrong (specificity) or occasionally irrelevant (experimental evidence and perhaps analogy). Hill admitted that: “none of my nine viewpoints can bring indisputable evidence for or against the cause and effect hypothesis and none (except temporality) can be required as a sine qua non”.
The IARC in its monograph programme largely adopted the causality criteria proposed by Hill and established rules to decide on the carcinogenicity of a given exposure, particularly when human data are scarce and must be combined with experimental data. However, the final qualification of the carcinogenicity of any given substance being evaluated is taken by vote of the external (non-IARC) participants.
The monograph programme and its criteria has been reviewed and accepted by most scientists in the field of human carcinogenesis. To date, 77 monographs have been published, of which five involve biological agents such as HPV.12 In its preamble, the monograph programme establishes guidelines to qualify an epidemiological observation as causal, and also defines rules to be followed when human data suggest lack of carcinogenicity potential. These criteria are useful to challenge any aetiological hypothesis when the epidemiological studies are inconsistent or when only weak associations are reported.
Finally, another useful way of examining the nature of an association was provided by a model system that proposed that any given disease would occur as a consequence of human exposure to a “sufficient cause”.18 A sufficient cause is described, in its simplest model, as the concurrence in a given individual of a constellation of factors (called the components of the sufficient cause), following which the disease will develop. Each given disease will have its own sufficient cause or sets of sufficient causes (lung cancer may have a sufficient cause that involves cigarette smoking, but another sufficient cause that does not include smoking, such as intense radon exposure in non-smokers). According to the model, a necessary cause is described as a component of a sufficient cause that is part of all the sufficient causes described. To prevent disease it is not necessary to identify all the components of a sufficient cause, or to remove them all: it is sufficient to remove one component from each sufficient cause, that is to remove, if it exists, the necessary cause.
COMPLIANCE OF THE CAUSALITY CRITERIA IN THE HPV AND CERVICAL CANCER MODEL
In the following sections, we will review several studies that have provided evidence of the association between HPV and cervical cancer, using the criteria outlined in table 1. For purposes of clarity, we shall concentrate the discussion on the criteria that have proved to be of greater value in the evaluation of human carcinogens and on the studies that focused on invasive cervical cancer.
Strength of the association
This criterion is usually discussed by examining the magnitude of the relative risk (RR), or the OR, which is the estimate of the RR in case–control studies. We shall use as the primary example the results of the IARC multicentre case–control study on invasive cervical cancer, as presented at international scientific meetings, and either published or at different stages of preparation for publication. In brief, this project included nine case–control studies in different parts of the world, mostly in high risk countries. HPV DNA testing was done in two central research laboratories using the MYO9/1120 and the general primer (GP) GP5+/6+21,22 polymerase chain reaction (PCR) testing systems. The published results have reported ORs for cervical cancer in the range of 50 to 100 fold for HPV DNA. ORs for specific associations (such as HPV-16 and squamous cell cancer and HPV-18 and cervical adenocarcinomas) range between 100 and 900. These estimates lead to calculations of attributable fractions (AF) for the entire study greater than 95%.23
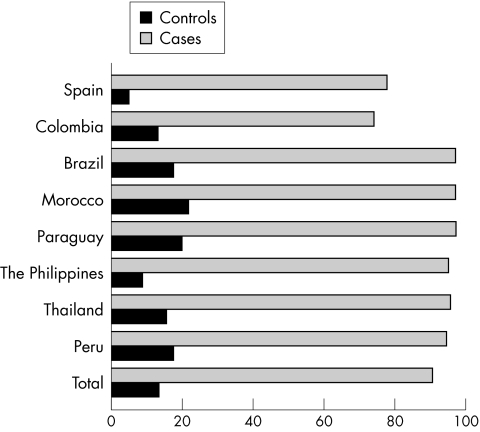
Table 2 shows the size of the multicentre case–control study and the prevalence of HPV DNA in each relevant group. Figure 3 displays the HPV DNA prevalence in eight countries in cervical cancer cases and controls. It is noteworthy that the first two studies conducted in Spain and Colombia (fig 3) used early versions of the MYO9/11 PCR system that identified HPV DNA in approximately 75% of the cases. The rest of the studies were analysed using the GP5+/6+ PCR system and its modifications, which resulted in an almost 20% increase in the HPV DNA detection rate.
Table 2.
Size of the IARC multicentre case–control study and human papillomavirus (HPV) DNA prevalence
| Cervical cancer | ||||||
| Controls | Adeno and mixed | Squamous | ||||
| No. countries | N | HPV DNA (% +ve) | N | HPV DNA (% +ve) | N | HPV DNA (% +ve) |
| 9* | 2491 | 13.4 | – | – | 2365 | 90.7 |
| 6† | 1466 | 15.4 | 141 | 91.9 | 2280 | 96.6 |
*Brazil, Morocco, Paraguay, the Philippines, Thailand, Peru, Mali, Spain, and Colombia.
†Brazil, Morocco, Paraguay, the Philippines, Thailand, and Peru.
Figure 3.
Prevalence of human papillomavirus (HPV) DNA in cases and controls in the IARC multicentre case–control study.24–30
Table 3 shows the corresponding estimates of the RR (OR and 95% confidence interval (CI)). Results are presented separately for squamous cell carcinomas and adenocarcinomas of the cervix. Given the case–control design of the study, these very high ORs reflect the risk in relation to existing HPV DNA in cervical cells (HPV DNA point prevalence), not in relation to “ever” being infected with HPV (cumulative lifetime exposure). Furthermore, if HPV shedding was intermittent among controls, their corresponding HPV prevalence would have been underestimated, resulting in an inflation of the ORs observed. It is usually interpreted that the HPV DNA point prevalence at advanced age (over 40 years of age) reflects viral persistency. However, much research is still devoted to defining viral persistency and its prognosis accurately, a crucial definition for the clarification of the uses of HPV testing in screening and patient management.31
Table 3.
Odds ratio for the association of human papillomavirus (HPV) DNA and cervical cancer in the IARC multicentre case–control study: preliminary data23,32,33
| HPV DNA prevalence (%) | ||||
| No. studies | Controls | Cases | OR (95% CI) | |
| Squamous | 9 | 13.4 | 90.7 | 83.3 (54.9 to 105.3) |
| Adeno and mixed | 6 | 15.4 | 91.9 | 68.7 (36.2 to 130.5) |
CI, confidence interval; IARC, Agency for Research on Cancer OR, odds ratio.
Most of the discussion in the text uses HPV DNA as a generic marker that includes any positive result for several HPV types. It is now possible to provide estimates of the RR for at least 10 different HPV types showing that there are no significant differences in the risk of cervical cancer in relation to the HPV types most commonly found in these lesions. The preliminary results of the IARC multicentre case–control were pooled and summarised by Muñoz et al in 2000,32 at the HPV 2000 Papillomavirus Conference (www.hpv2000.com). These analyses indicated that for squamous cell carcinomas, the age and centre adjusted OR was 83.3 (95% CI, 54.9 to 105.3). The prevalence of the four most common HPV types and their ORs among 1545 cases with single infections were: HPV-16, 59% (OR = 182); HPV-18, 12% (OR = 231); HPV-45, 4.8% (OR = 148); and HPV-31, 3.7% (OR = 71.5). Other less common HPV types showing equally high ORs were: HPV-33, OR = 77.6; HPV-35, OR = 34.8; HPV-51, OR = 42.7; HPV-52, OR = 145.7; HPV-58, OR = 78.9; and HPV-59, OR = 347.3.
The most common types among cases were also the most common types among HPV positive control women: HPV-16, 30.3%; HPV-18, 8.2%; HPV-31, 4.8%; and HPV-45, 3.9%. These findings indicate that in addition to HPV-16 and HPV-18, HPV types 31, 33, 35, 45, 51, 52, 58, and 59 should be considered as human carcinogens.
The HPV type distribution in the population and in patients with cervical cancer shows a seemingly modest geographical variability that has not been fully described (J Kornegay, personal communication, 2001).34–36 The description and the implications of such variability for HPV testing and HPV vaccination are to be determined.
The results of the multicentre study are consistent with findings from other countries that have generated recent data on invasive cervical cancer and preinvasive disease in Costa Rica,37 Thailand,38 Norway,39 Denmark,40 and virtually all other countries in which these studies have been conducted.
Multiple HPV types were detected in the multicentric study on average in 7.3% of the cases and 1.9% of the controls, and did not show a significantly increased risk (OR = 54.5; 95% CI, 35.5 to 83.6) over women positive for only one HPV type (OR = 86.6; 95% CI, 68.2 to 110).
The proportion of multiple types in a given specimen varies across studies and particularly in relation to the HPV detection method used. Table 4 provides an indication of the proportion of specimens from cases and from the general population that showed multiple types. The table suggests that populations at high risk of cervical cancer and with high rates of human immunodeficiency virus (HIV) positivity tend to show higher proportions of multiple types than do populations not belonging to these risk groups. Longitudinal studies have suggested that the one time, cross sectional detection of type specific HPV may underestimate the cumulative lifetime diversity of exposure to HPV.31 However, in all studies of invasive carcinoma, the risk linked to multiple HPV types does not vary significantly from the risk linked to single HPV types.
Table 4.
Prevalence of multiple human papillomavirus (HPV) types in patients with cervical cancer and women without cervical cancer
| Ref | Cases | Non-cases | ||
| Ref | % Of all specimens | % Of all the HPV +ve | % Of all specimens | |
| 32 | IARC multicentre | 4–20% | 10% | 1–3% |
| 37 | Rural Costa Rica | 32% | 38% | 4% |
| 35 | Rural Mozambique | – | 41% | 15% |
| 41 | Imprisoned women, Spain | – | 71% | 20% |
| 42 | HIV +ve, USA | – | 42% | – |
| HIV -ve, USA | – | 16% | – | |
IARC, International Agency for Research on Cancer.
The similarity in the prognostic value of detection of any of the 10 high risk HPV types, in addition to any combination of them, clearly indicates that group testing for high risk HPVs would be sufficient in the context of clinical and screening protocols.
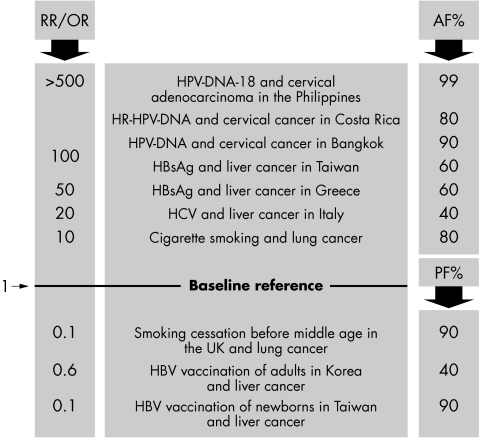
Figure 4 shows, for comparison purposes, some estimates of the strength of associations between environmental factors and human cancer that were recognised as causal in nature by epidemiological studies and subsequently proved in human populations by intervention studies. The figure includes risk (RRs or ORs) as the measurement of the strength of the associations and AFs representing the proportion of disease that is attributable to (caused by) the exposure. Below the reference line the risk column displays its reverse estimate as a less than one (protective) OR or RR and the protective fractions (PF%) in the right hand column show results that have already been achieved in disease reduction after specific exposure reduction interventions.
Figure 4.
Selected examples of the strength of the associations (RR/ OR) between risk factors and human cancer; estimates of the attributable fraction (AF%) and of the protective fraction (PF%). Refs: the Philippines,28 Costa Rica,37 Bangkok,5 Taiwan,43 Greece,44 Italy,45 UK,46 Korea,47 and Taiwan.48
Strength of association. Evaluation.
The association between HPV DNA in cervical specimens and cervical cancer is one of the strongest ever observed for a human cancer. HPV-16 accounts for almost 50% of the types identified in cervical cancer. The cancer risk for any one of at least 10 HPV types or for any combination of HPV types does not differ significantly.
Consistency
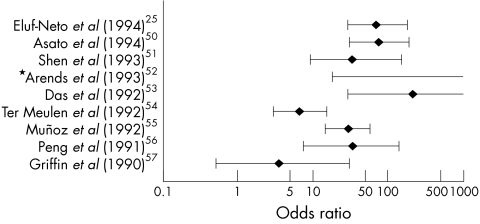
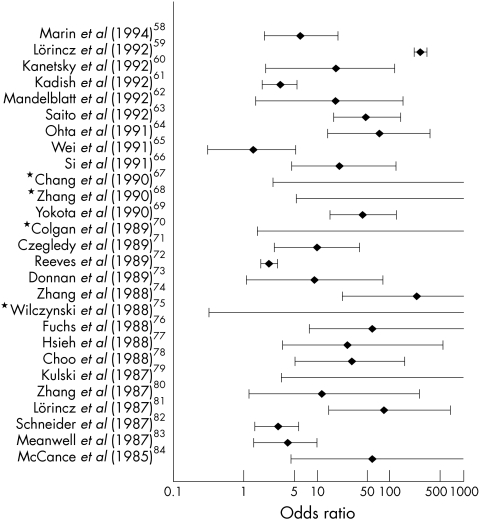
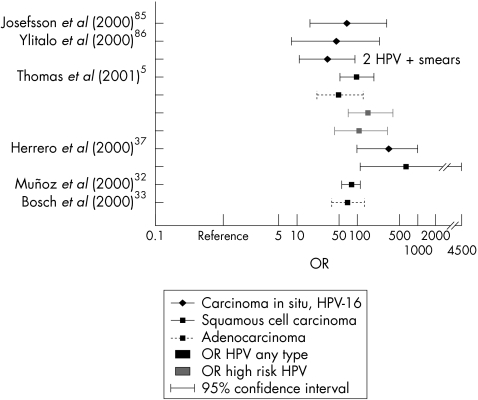
There is a striking consistency between the results of the multicentre case–control study and over 50 other studies conducted in other countries, under different protocols and HPV DNA testing systems. Figures 5, 6, and 7 summarise the results of studies that compared the prevalence of HPV DNA in patients with cervical cancer and controls. Some of the studies used the prevalence of HPV-16 DNA to calculate ORs and some reported results for HPV DNA (all types combined). Some studies focused on invasive cervical cancer, whereas others used preinvasive lesions as the definition of cases. When indicated, separate analyses are presented for squamous cell carcinomas and for adenocarcinomas. Studies that have compared risk factors for cervical intraepithelial neoplasia stage 3 (CIN 3) and invasive cancer have not reported any significant differences in their associations with HPV or with their epidemiological profile.38,49
Figure 5.
Odds ratios (OR) and 95% confidence intervals for associations found in case–control studies using PCR methods between human papillomavirus 16 (HPV-16) (or its nearest surrogate) and invasive cervical cancers. *The OR estimate is ∞ owing to the absence of HPV positive controls. Adapted from IARC monograph 64, 1995.12
Figure 6.
Odds ratios (OR) and 95% confidence intervals for associations found in case–control studies using non-PCR methods between human papillomavirus 16 (HPV-16) (or its nearest surrogate) and invasive cervical cancers. *The OR estimate is ∞ owing to the absence of HPV positive controls. Adapted from IARC monograph 64, 1995.12
Figure 7.
Odds ratios (OR) and 95% confidence intervals for associations found in case–control studies after the year 2000. HPV, human papillomavirus.
Apart from confirming the high ORs shown in figs 5 and 6, fig 7 also demonstrates the consistency of results between squamous cell carcinomas and adenocarcinomas, the consistency of findings between preinvasive disease and invasive cancer, and the consistency of findings between risk estimates for HPV DNA (all types considered) and risk estimates restricted to high risk types.
Consistency. Evaluation.
The association between HPV DNA in cervical specimens and cervical cancer is consistent in a large number of investigations in different countries and populations. There are no published studies with observations challenging the central hypothesis on causality.
Specificity
Specificity, as defined by Hill, tended to be relegated to a secondary level for cancer causality evaluation once it became clear that carcinogenic exposures are usually complex (for example, cigarette smoke) and can induce cancer in different organs and even cancers of different histological profile in the same organ.
In the case of HPV, the complexity of the association is being unveiled. The HPV family includes over 100 HPV types, of which 30–40 are mucosatropic and at least 15 types have been clearly linked to cervical cancer. In addition, some of these types are also related to other cancers of the genital tract (vulvar cancer, vaginal cancer, and cancers of the anal canal, perianal skin, and the penis) and perhaps to cancers of other organs (such as oropharyngeal and skin cancer).
To examine the association of HPV and human cancer in light of the specificity criteria, we shall widen the original scope (one exposure/one disease) to verify whether a more complex model involving multiple HPV types and several cancer sites seems to occur with frequencies suggesting a consistent departure from a random model.
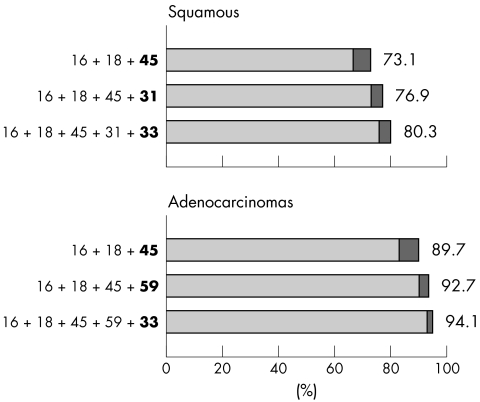
About 15 HPV types are involved in over 95% of the cervical cancer cases. HPV-16 and HPV-18 are the most common types identified and represent 50% and 10%, respectively, of the viral types involved in invasive cancer. Figure 8 shows the cumulative prevalence of five HPV types in cervical carcinomas by histological type in 2400 cases included in the multicentre case–control study. It clearly shows that these five HPV types comprise 80–95% of the viral types identified in carcinomas.
Adenocarcinomas and adenosquamous cell carcinomas are more closely related to HPV-18 and its phylogenetically related family (HPV types 39, 45, and 59) than are squamous cell carcinomas, which in turn are closely linked to HPV-16 and its phylogenetically related family (HPV types 31, 35, and 52).34,87 The reasons for such specificity are unknown.
Cancers of the vulva and vagina are closely related to HPV-16. Approximately 40–50% of vulvar cancer shows HPV DNA, and in several series HPV-16 is by far the predominant type in more than 80% of cases.88–90
Cancer of the tonsil is closely related to HPV-16, whereas other cancers of the oral cavity show inconsistent and lower prevalences of HPV DNA.91–94
Skin cancers related to the epidermodysplasia verruciformis condition are related to a restricted number of dermatotrophic HPV types. These are also recovered from basal cell carcinomas and squamous cell carcinomas of the skin in immunosuppressed and immunocompetent individuals.95
Other associations, reported in a small number of cases, seem to occur with some specificity. For example HPV-16 and cancers of the conjunctiva96 and HPV-16 and cancers of the ungueal bed.
Studies on HPV variants (variation within HPV types at the single nucleotide level) are beginning to unveil risk differences.97–99 The geographical distribution of HPV variants and its relevance for HPV testing and for vaccine development are still uncertain.
HPV has been excluded as a likely cause or even as a risk factor for other human cancers. A large number of investigations (largely unpublished) have not provided support to the hypothesis of the involvement of these viruses in the causation of cancers of the endometrium, ovary, prostate, or other sites (reviewed by Shah and Howley16 and Syrjänen and Syrjänen100).
Figure 8.
Cumulative prevalence of human papillomavirus (HPV) types in cervical cancer. Taken from the IARC multicentre case–control study; preliminary data.23
Specificity. Evaluation.
The association of type specific HPV DNA and cervical cancer is significantly different from random. Systematic patterns of HPV type and cervical cancer histology suggest a fair degree of specificity. Patterns are also observed when the scope of HPV and cancer expands to include the full spectrum of HPV types and the large number of addi-tional cancer sites that have been investigated.
In conclusion, although the specificity criteria can be viewed as of secondary applicability, the global picture indicates that HPV types are not randomly associated with human cancer. A fair degree of specificity is consistently reported, even if the complexities of the type specific viral properties and of the organ/cell susceptibility have not been fully disclosed.
Temporality
Of the criteria outlined by Hill and repeatedly endorsed by the IARC monograph programme and other bodies, the demonstration that exposure has occurred before the diagnosis is considered a “sine qua non” condition for a risk factor and for establishing causality. Five groups of studies have contributed data relevant to the temporality criterion.
Descriptive data
Cross sectional studies have repeatedly reported that subclinical HPV infections are highly prevalent in young individuals, whereas invasive cervical cancer typically develops in the third decade and later (fig 9). The cross sectional prevalence of HPV DNA decreases spontaneously to a background level of 2–8% in most populations in groups that are 40 years old and above. In countries where intensive screening of young women takes place, part of the HPV prevalence reduction could be attributable to aggressive treatment of HPV related cervical lesions. Women who remain chronic HPV carriers are currently described as the true high risk group for cervical cancer. In some populations, a second mode of HPV DNA prevalence has been observed for older women (50 years and above), with uncertain relevance in relation to the risk of cervical cancer.36,37,101 In all settings investigated, the point prevalence of HPV DNA in the young age groups is strongly related to the sexual behaviour patterns that are dominant in each population.102–107
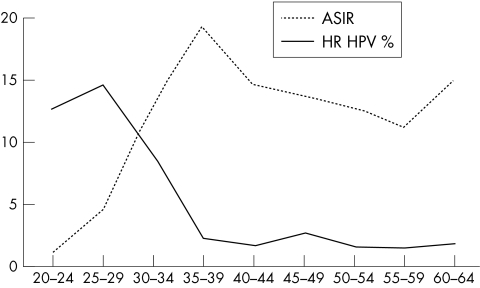
Figure 9.
Age specific prevalence (%) of high rish (HR) human papillomavirus (HPV) DNA in 3700 women entering a screening programme and age specific incidence rate (x105) (ASIR) of cervical cancer in the Netherlands. Adapted from Jacobs et al and Parkin et al.106,108
These population studies provide support for the concept that HPV infections precede the development of cervical cancer by some decades. In fact, from most cancer registries, including the USA based registries, it is well established that the age specific incidence of cervical cancer has a rising trend in the age interval 20–40, and shows a plateau or continues to increase smoothly after that age. Only occasionally do cases of invasive disease occur at earlier ages. Figure 9 shows the age specific, cross sectional prevalence of high risk HPV DNA in a screening programme in the Netherlands, and the corresponding age specific incidence rates of cervical cancer in that country. The distributions shown in fig 9 are highly reproducible in studies in other settings in high and low risk countries.3,24,106,108 However, the age specific incidence rates of invasive cervical cancer are strongly influenced by the local impact of screening programmes in each country.3,24,106,108
Follow up studies
For cervical cancer, compliance with the temporality criteria has been established by numerous cohort studies that monitored women from cytological normalcy to the stage of high grade cervical intraepithelial neoplasia (high grade squamous intraepithelial lesions (HSIL) or CIN 2/3). Monitoring of women to invasive disease is not acceptable on ethical grounds and thus that information is not available.
Repeated sampling of women being followed for viral persistence and cervical abnormalities has shown that the median duration of the infections is around eight months for high risk HPV types, compared with 4.8 months for the low risk HPV types. In two unrelated studies, the time estimates were fairly consistent. In one study in a high risk population in Brazil, the mean duration of HPV detection was 13.5 months for high risk HPV types and 8.2 months for the non-oncogenic types. HPV-16 tended to persist longer than the average for high risk types other than HPV-16.109 The results were remarkably similar in a student population in the USA and in the UK.31,110 The self limiting course of most HPV infections is consistent with the cross sectional profile displayed in fig 9. However, the currently observed time intervals may still suffer from imprecision in the estimates of time at first exposure, from the variability in the endpoint definition, and from censoring as a result of treatment of the early lesions.
Follow up studies of women with and without cervical abnormalities have indicated that the continuous presence of HR-HPV is necessary for the development, maintenance, and progression of progressive CIN disease.110–114 A substantial fraction (15–30%) of women with HR-HPV DNA who are cytomorphologically normal at recruitment will develop CIN 2 or CIN 3 within the subsequent four year interval.111,115,116 Conversely, among women found to be HR-HPV DNA negative and cytologically identified as either atypical squamous cells of undetermined significance (ASCUS) or borderline or mild dysplasia, CIN 2/3 is unlikely to develop during a follow up of two years, and their cytology is likely to return to normal.117,118 Women found positive for low risk HPVs rarely become persistent carriers and their probability of progression to CIN 2/3 is extremely low.117,119
As ongoing cohorts expand their follow up time, more precise estimates are being provided on the predictive value of viral persistence as defined by repeated measurements of viral types and variants. One such cohort in Sao Paulo has shown that the incidence of cervical lesions in women who were HPV negative twice was 0.73/1000 women months. The corresponding incidence among women with repeated HPV-16 or HPV-18 positive results was 8.68, a 12 fold increased incidence. The OR for HPV persistence among women who were twice HPV positive for the same oncogenic types was OR = 41.2 (95% CI, 10.7 to 158.3).120 Retrospective assessment of HPV status using archival smears from cases of cervical cancer and controls has provided evidence that HPV DNA preceded the development of invasive disease, and showed its value in signalling false negatives smears.117 An interesting observation from the same group suggests that the clearance of HR-HPV in otherwise established cytological lesions is a marker associated with the regression of CIN lesions.118,121 Finally, the persistence of HPV DNA after treatment for CIN 2/3 is an accurate predictor of relapse, and is at least as sensitive as repeated vaginal cytology.122
These results are useful in defining the clinical role of HPV testing. However, most observations on preinvasive disease have limitations for making inferences on cervical cancer causality. This is because even in controlled settings, observations are not allowed to continue beyond the stage of HSIL/CIN 3 or carcinoma in situ.
Retrospective cohorts
A particularly interesting approach to conducting follow up studies of invasive cancer (as opposed to studies of CIN 3) without ethical and time constraints is provided by so called “nested case–control studies”. These are studies initiated several years in the past that assembled and stored large banks of biological specimens from healthy individuals. Linkage studies can then identify cases of cervical cancer (or any other condition) that have occurred in the interval and the original specimens can then be analysed for the presence of HPV biomarkers. HPV DNA prevalence can then be compared with the corresponding prevalence in specimens of epidemiologically sound controls (individuals from the same cohort who did not develop the condition under otherwise equivalent exposures). These studies have documented the existence of HPV exposure years before the development of the disease, thus reproducing the conditions of a longitudinal study. With this approach, a RR estimate of 16.4 (95% CI, 4.4 to 75.1) was seen for invasive cervical cancer in Sweden using DNA extracted from stored Papanicolaou (Pap) smears123 and a RR of 32 (95% CI, 6.8 to 153) was seen in the Netherlands.117 In a similar study design, an OR of 2.4 (95% CI, 1.6 to 3.7) was obtained using serological markers of HPV exposure.124
Preventive interventions
Since the late 1980s, multiple studies have evaluated HPV testing as an adjunct to cytology in screening programmes. These have considered HPV testing either as a triage test in cases of mild abnormalities125–127 or as a primary screening test.128–130 It is not the purpose of this paper to review this literature and excellent summaries are being regularly produced and updated (see later). In brief, triage studies have shown that HPV testing is more sensitive than repeated cytology in identifying underlying high grade lesions in women with ASCUS.114,119,121,131,132 Studies that reflect primary screening conditions (in the absence of fully randomised trials) have shown that the sensitivity of HPV tests is higher than standard cytology in detecting high grade lesions, whereas the specificity is age dependent. HPV tests show lower specificity than cytology in younger women, accounting for the bulk of transient infections, whereas in older women (ages 30–35 and above) specificities tend to be similar for both tests.107,133,134
In terms of causality assessment, these studies showed that it is possible to predict the concurrent presence of neoplastic disease (usually HSIL, CIN 2–3, or severe dyskaryosis), or the risk of developing it, by means of HPV DNA detection. This property of the HPV test offers an indirect measurement of the strength of the association and of the temporal sequence of the events.
Determinants of HPV infection
Epidemiological studies investigating risk factors for HPV infection clearly and consistently have shown that the key determinants among women are the number of sexual partners, the age at which sexual intercourse was initiated, and the likelihood that each of her sexual partners was an HPV carrier.103,105,135–141 These are lifelong behavioural traits, thus clearly preceding the development of cervical cancer.
The role of men as possible vectors of HPV was measured in the early epidemiological studies by questionnaires that asked about the sexual behaviour of the husbands or sexual partners of patients with cervical cancer and controls. In addition, more recent studies had the ability to measure HPV DNA in exfoliated cells from the penile shaft, the coronal sulcus, and the distal urethra.142–146
These and other studies consistently showed that the risk of cervical cancer for a given woman can be predicted by the sexual behaviour of her husband as much as her own sexual behaviour. In populations where female monogamy is dominant, the population of female sex workers plays an important role in the maintenance and transmission of HPV infections. Moreover, the probability that a woman is an HPV carrier and her risk of developing cervical cancer have been shown to be related to the presence of HPV DNA in the penis or the urethra of her husband or sexual partner.104,147–149 More recently, it has been possible to confirm that male circumcision protected men from being HPV carriers and their wives from developing cervical cancer.150 These observations confirmed, in terms of HPV infections, observations made over a century ago151 and a scientific hypothesis formulated almost 30 years ago that male sexual behaviour is a central determinant of the incidence of cervical cancer.152,153
In conclusion, the natural history studies of HPV infections satisfy in biological terms most of the observations that were historically linked to cervical cancer. In the past two decades, the cervical cancer puzzle has become a coherent description that includes the identification of HPV as the sexually transmitted aetiological agent and the characterisation of the major determinants of HPV acquisition.154
Temporality. Evaluation.
HPV infections precede cervical precancerous lesions and cervical cancer by a substantial number of years. The epidemiology and the dynamics of HPV infection in populations satisfy previous observations that related cervical cancer to a sexually transmitted disease.
Biological gradient
This refers to the presence of a dose–response curve indicating that the magnitude of the exposure is related to the risk of disease. This requirement, largely supported by chemically induced models of carcinogenesis, is difficult to apply in models of viruses and cancer. For HPV DNA, it is difficult to measure viral load in relation to the DNA of the cancer cells in the specimen, although early studies tended to show a correlation between HPV DNA amount and disease status.127 Some recent publications have provided relevant evidence using real time PCR methods. A study that used a nested case–control design found that cases consistently had higher viral loads for HPV-16 than controls, and that high viral loads could be detected up to 13 years before the diagnosis of cervical cancer.155 Women with high viral loads for HPV-16 had a 30 fold greater risk of developing cervical cancer than did HPV negative women. This also applied to women under the age of 25. A related paper using the same population showed that the 20% of the population with the highest viral loads for HPV-16 had a 60 fold higher risk of developing carcinoma in situ when compared with HPV negative women.85 Of importance for clinical and screening purposes, another study confirmed that high viral loads predicted cervical lesions and, more interestingly, that the reduction of viral load or clearance of viral DNA in repeated visits predicted regression of CIN lesions to normalcy.156 These studies suggest that measuring viral load, at least of HPV-16, may distinguish between clinically relevant infections and those that are unlikely to progress. However, in contrast to the above results one large prospective study in Portland USA, using quantitative hybrid capture, did not find viral load to be a determinant of risk of future CIN 3 (A Lorincz et al, unpublished data, 2002). More research is needed to validate these methods and the results need to be extended and confirmed in clinical studies.157
Biological gradient. Evaluation .
The risk of cervical cancer may be related to estimates of viral load. The technology to estimate viral load is being developed and compliance with the biological gradient requirement needs to be further validated.
Biological plausibility and coherence
The mechanisms by which HPV induces cancer in humans and the molecular genetics of the process are being investigated intensively and excellent reviews are readily available.12,16,17,158–161 These investigations provide additional evidence on the causality of the association by describing viral and host interactions leading to cell transformation and malignancy. Of the criteria outlined in table 1, both the “biological plausibility” and understanding of the “mechanisms” are in rapid expansion as a consequence of developments in molecular methods and technology.
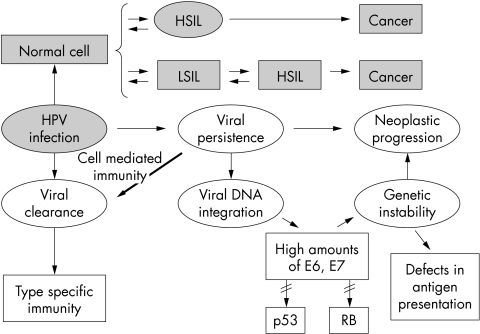
Figure 10 shows in a schematic manner some of the major components of the transition from HPV infection to cervical cancer. Whereas transient infections are largely subclinical, progression is closely related to the persistence of viral DNA. This process goes frequently with viral disruption in the E1/E2 regions and integration into the cellular DNA. E2 disruption releases the viral promoters of E6 and E7 and increases the expression of these transforming genes. The E6 and E7 viral proteins are capable of selectively degrading the p53 and retinoblastoma gene (RB) products, respectively, leading to inactivation of two important cellular negative regulatory proteins.
Figure 10.
Mechanisms of human papillomavirus (HPV) carcinogenesis. HSIL, high grade squamous intraepithelial lesion; LSIL, low grade squamous intraepithelial lesion; RB, retinoblastoma gene.
Some characteristics that provide support for the role of HPV in the induction of cervical cancer were recently outlined.17 Accordingly, the causal nature of this association is indicated by: (1) the regular presence of HPV DNA in the neoplastic cells of tumour biopsy specimens; (2) the demonstration of viral oncogene expression (E6 and E7) in tumour material (but not in stromal cells); (3) the transforming properties of these genes (E6 and E7); (4) the requirement for E6 and E7 expression to maintain the malignant phenotype of cervical carcinoma cell lines; (5) interaction of viral oncoproteins with growth regulating host cell proteins; and (6) epidemiological studies pointing at these HPV infections as the major risk factors for cervical cancer development.
In their review, Shah and Howley16 provided references to some of the key experiments that exemplify most of the requirements indicated by zur Hausen,17 namely: (1) The genomes of HPV-16 and HPV-18 are capable of immortalising human keratinocytes in cell culture, whereas the DNA of the low risk HPV types (6/11) do not.162 (2) In raft cultures, the oncogenes of the high risk HPV types induce morphological changes that closely resemble preinvasive cervical lesions.163,164 (3) In HPV associated lesions, the viral genome is present in every cell and is always transcriptionally active.165 (4) The viral genome is present in the original tumour and in metastases.166 (5) Most of the cell lines established from cervical cancer contain either HPV-16 or HPV-18 genomes.167 (6) The pattern of transcription changes as the lesion increases in severity. All open reading frames (ORFs) are expressed in early lesions but the expression of ORFs E4 and E5 is not found in many invasive cancers.165 (7) The E6 and E7 ORFs contain the transforming ability of HPV. These are always intact and are consistently expressed in cervical cancer cell lines, in cells transformed by HPV, and in HPV associated cancer tissue. They are transcribed at higher levels in high grade lesions than in low grade lesions.165,168 (8) In most cell lines and in many HPV associated cancers, the HPV DNA is integrated into the cellular DNA. HPV-18 is nearly always integrated, whereas HPV-16 can be found episomally or in the integrated form.76,169,170
In reviewing work on the molecular genetics of cervical carcinoma, Lazo indicated different mechanisms of cancer induction. The effects of E6 and E7 on host regulatory proteins can be considered to be HPV related mechanisms. An additional effect could be expected from the consequences of viral integration and the specific impact on the integration sites. The third mechanism, which may or may not be related to HPV, is the accumulation of the cellular genetic damage needed for tumour development. The existence of this mechanism is strongly suggested by the observations of recurrent losses of heterozygosity and by recurrent amplifications in a large fraction of cervical carcinomas.160 The role of non-identified tumour suppressor genes is also suggested by experiments showing that the tumorigenicity of HeLa cells could be suppressed by fusion with normal fibroblasts or keratinocytes, and that the tumorigenicity of SiHa cells was suppressed by the introduction of chromosome 11 via microcell transfer technology.171–173 Similarly, the immortality of Hela and Sitta cells was suppressed by the introduction of chromosomes 3, 4, and 6.174,175
Although a review of the field is far from the purposes of this discussion, it seems quite clear that the biology of cervical cancer in relation to HPV has become a paradigm of viral mediated oncogenesis. The work being regularly published has clearly shown that the viral DNA detected by epidemiological studies is not a passenger infection of the cancerous tissue, but a biologically meaningful association.
Biological plausibility and coherence. Evaluation.
The association of HPV DNA in cervical specimens and cervical cancer is plausible and coherent with previous knowledge. This includes in vitro experiments, animal experiments, and observations in humans. Novel criteria of causality are being proposed and tested as molecular technology develops and is introduced into epidemiological research protocols.
Biological mechanisms of HPV carcinogenesis
In previous decades, our understanding of cancer pathways was rudimentary and often incorrect. In the face of such uncertainty, arguments based on assumptions of molecular biology were not particularly convincing. However, with the large body of work now available it is possible to develop a reasonable understanding of the ways in which cancer may develop and ways in which HPV infection can drive the process. Thus, we can say with some confidence that it is plausible for HPV to cause cervical cancer and, furthermore, we can describe with reasonable clarity the general steps by which HPV may do so. Of course there is a lot of detail still to be revealed, but we are well on our way to a factual basis for understanding carcinogenesis rather than the guesswork and rudimentary models of just two decades ago.
What follows is a description of selected information that may illuminate salient aspects of the natural history of HPV and reasons why a mostly benign infectious process sometimes results in malignancy. It must be understood by readers that the pathways discussed are based on extensive experimentation in biopsied human tissues, in tissue culture, and other kinds of molecular biology systems. However, many details of pathway modifications and aberrant pathway effects are speculative—they have not been shown to occur inside the relevant precancerous and cancerous tissues of living hosts. However, despite the many holes and inconsistencies, the models are still quite compelling and cohesive in facts. In future, we expect to see these molecular models being tested in human subjects.
Essentially all HPV types produce warty lesions but only high risk types promote the development of cervical cancer to any appreciable extent. Such differences between HPV types may seem surprising, given the high DNA and structural similarities. However, a large functional divergence caused by small genetic changes is the norm in many biological systems. Variations in carcinogenic potential among HPVs are principally governed by the E6 and E7 proteins; specifically by the capacities of these proteins to interact with and alter or destroy key cell cycle regulatory molecules.176–178
The progress and outcome of an HPV infection depend on HPV type, anatomical location, and the nature and timing of local cellular and tissue influences.179–183 Virions access basal and parabasal cells in areas of erosion and viral DNA enters the cell nuclei. Establishment is tied to the tissue proliferative activity of epithelial cells and, in the case of extensive tissue repair, the viral infection can become widely disseminated. Persistence in keratinocytes is variable and related to viral type.109,112,184 Finally, integration of viral DNA may occur, resulting in lifetime persistence of certain viral genes in the cell. In the cervix, detectable infection by low risk HPV types is of relatively short duration, whereas infection by most high risk types lasts longer. On occasion, such infections may become persistent and last years or even decades; it is in these cases that the risk of cancer is increased.
The establishment of HPV infection can be modulated by a competent and primed immune system. In vitro experiments have revealed an inverse association between the degree of cervical neoplasia and interleukin 2 production by peripheral blood mononuclear cells in response to HPV-16 E6 and E7 peptides.184,185 Women with CIN 3 or cancer appear to have a decreased ability to mount a T helper cell type 1 (Th1) mediated immune response to HPV E6/E7, compared with women with CIN 1 or HPV infected women without lesions.184,185 It is possible that a Th1 mediated cellular immune response could play a role in host immunological control of HPV infection and that lack of such an appropriate response may predispose to the progression of cervical disease.
If HPV enters immature metaplastic basal stem cells that are actively dividing the infection can become widely dispersed and persistent. In contrast, if infection occurs only in the parabasal transit amplifying cells the infection may become transient or quasi-persistent.179–182 The size, histological grade, and duration of lesions can depend on the number and types of cells that become infected by HPV. In either transient or persistent infection there may be periodic viral genome amplification, depending on the activity of the infected daughter cells, which can lead to variable detection of the lesion by HPV DNA or Pap tests.
There is an important difference in host–virus interactions of carcinogenic HPV types and low risk HPV types—the former have activities that more strongly interfere with a set of host cell cycle control mechanisms. It is therefore useful to consider the effects of carcinogenic HPV types. HPV initially replicates to reach about 25–50 genomes/cell.179–182,186–188 The process by which this occurs is tied to the activities of four multifunctional viral proteins E1, E2, E6, and E7.176–178,189–191 One key activity of E7 is to overcome the pRB tumour suppressor block.176 Binding of E7 to pRB and its related members results in the liberation of E2F transcription factors, which play key roles in promoting host cell and viral DNA synthesis. E7 also binds and activates cyclin complexes, such as p33–cyclin dependent kinase 2,192 which control progression through the cell cycle. E6 protein can overcome the p53 protective control pathways,178 which are important in preventing the genetic damage that may lead to cancer.
HPV genomes attach to host chromatin via the E2 protein and replicate at a steady state, once for each cell division.186–188 It has been speculated that a benefit of this tethered theta mode of replication is that the loss of HPV DNA from cells by non-disjunction is minimised and the presence of low amounts of HPV DNA in cells is less likely to be detected by intracellular interference mechanisms that could trigger apoptosis. As cells differentiate and move to the surface there is a normal differentiation and maturation process that leads to pyknotic condensed cells that slough from the tissue. However, in virally infected tissues there is activation of unscheduled DNA replication in some spinous cells, accompanied by a switch in viral DNA replication to the rolling circle mode, which leads to the production of viral progeny.179–182 This reactivation of DNA synthesis can be detected by the presence of punctate proliferating cell nuclear antigen tissue staining (a protein with a key role in DNA replication) and the presence of HPV virions in a subset of upper layer cells.
HPV E7 proteins of both low and high risk types have an ability to promote unscheduled DNA replication in spinous cells.179–182,193 It is believed that the extent to which E7 stimulates cells, and the tissue location at which such stimulation occurs, is important to malignant progression. Spinous cells respond to E7 by the production of a cyclin kinase inhibitor, p21cip1, translated from sequestered RNA. In basal and parabasal cells existing mRNA for p21cip1 is not available and the protein is typically produced from new transcripts stimulated by p53; however, if p53 is inactivated by E6 the p21cip1 cannot be made. Spinous cells thus have a control advantage lacking in basal cells. Interestingly, high amounts of E7 can bind and block the activity of p21cip1. The relative amounts of E7 and p21cip1 are believed to determine whether cells re-enter S phase and replicate viral DNA or whether cells block viral production. The inspection of tissues reveals a mutually exclusive set of spinous cells with high amounts of either E7 or p21cip1.179–182 Cells in which E7 overcomes the p21cip1 block can become koilocytes and produce viral particles. This balance can explain the patchy expression of the HPV effect in infected tissues.177,194 A key function of the E6 oncoprotein is the destruction of p53, a protein that is activated upon phosphorylation via DNA damage sensing proteins. Activated p53 stops the cell cycle in the G phase as a result of direct stimulation of p21cip1 by this molecule. Alternatively, in the case of major DNA damage or high amounts of viral replication, p53 may activate an apoptotic pathway.195,196 E7 also interferes with alternative non-p53 dependent apoptotic pathways. Thus, in the case of E6 mediated destruction of p53, cells are unable to prevent the accumulation of genetic mutations. Cells have other defensive homeostasis mechanisms, but E6 and E7 have counter functions that can lift the blocks and direct cells to enter S phase. Therefore, it appears that the development of malignancy is a consequence of an aberrant host–virus interaction. A potentially important event in this process is the aberrant regulation of E6/E7 expression.182,187,197,198 In low grade CIN lesions, E6/E7 expression is mainly found in differentiating spinous cells that have withdrawn from the cell cycle. In high grade CIN lesions and cervical carcinomas, strong E6/E7 expression is seen in the proliferating cell compartments.
HPV DNA is frequently integrated into the host genomes in cancers in such a way that the E2 repressor protein is inactive and allows overexpression of E6 and E7.170,199,200 In cases where HPV integration is not detected, other mutations can be shown in the E2 protein or in repressor functions, such as YYI sites,201–203 which appear to allow continuous expression of the E6 and E7 oncoproteins. Yet another way in which E6 and E7 could be overexpressed in proliferating cells is by the generation of chimaeric HPV mRNAs encoding the E6 and E7 proteins that have host sequences at their 3` termini. Such RNAs are frequently more stable and allow more protein to be synthesised.191
In persistent HPV lesions, viral genomes in the basal cells continue to stimulate the cells to ignore the DNA damage that may be accumulating.204,205 Cell stimulation by E6 and E7 of high risk carcinogenic HPV types produces clones with an extended life span that have passed a point called mortality 1 or M1, although the cells are still not immortal.198 An important step in immortalisation is related to telomeres. Normally, telomeres shorten every cell generation and once they reach a critical length the cells die. Telomere length is maintained by telomerase, which in combination with a capping function, can stabilise and even lengthen telomeres, allowing cells to continue dividing. E6 can activate telomerase and additional cell mutation(s) can then stabilise the telomeres and allow cells to pass a second stage called mortality 2 or M2. It is not known how many additional independent mutations are needed to transform immortalised cells fully to malignancy.191 One set of mutations allows the cell to break through the basement membrane by eliciting a set of novel proteases. Another mutation(s) allows cells to move in the dermis.206 Undoubtedly, metastatic cells have accumulated many additional mutations that allow them to create their own microenvironment for survival in foreign parts of the body.
Biological mechanisms of HPV carcinogensis. Evaluation.
The natural history of HPV infection and its relation to cancer development is being described by molecular technology. These investigations indicate that the induction of cancer by HPV is mediated by viral interference with essential regulatory mechanisms of cellular growth, DNA repair, and immunological escape. The alternative hypothesis of HPV being an opportunistic passenger in the tumoral tissue is no longer tenable.
Experimental evidence
Intervention studies in human populations would require the demonstration of a reduction in cervical cancer incidence and mortality following a reduction in the incidence of HPV infection in the underlying population. Prophylactic vaccines are being developed and vaccination trials are in advanced planning phases to evaluate such expected effects.
Review of the animal models for HPV related lesions, including cancer, is out of the scope of this report. In brief however, there are animal models of PV infections that induce warts and carcinoma in the skin, mucosa, and the digestive tract. The bovine PV (BPV) induces fibropapillomas in the skin and carcinoma of the digestive tract in animals exposed to bracken fern in their diets. Cottontail rabbit PV (CRPV) induces papillomas that could evolve into carcinomas either spontaneously or following the application of various promoters. Canine oral PV (COPV) causes oral papillomas that do not undergo malignant transformation. Several of these models are actively being used in the preparation of vaccines (for a review see Saveria Campo207 and Tindle).208 Many other papillomaviruses have been identified in animal models.209
Experimental evidence. Evaluation.
Experimental evidence shows that species specific papillomaviruses induce papillomas and cancers in the susceptible host.
Analogy
Analogy is no longer viewed as an essential criterion for causality assessment. As proposed by Hill, analogy would allow several considerations in the HPV and cervical cancer model that could be mentioned:
If other DNA viruses (such as HBV) can induce cancer in humans, HPV could too.
If animal PVs can induce papillomas and carcinomas in several animal models, HPV could do the same in humans.
If viral products that interfere with p53 and RB in animal models, such as the simian virus 40 large tumour antigen (SV40 tag), induce cancers in animal species, HPV could do so in humans.
Analogy. Evaluation .
The HPV and cervical cancer model is analogous to many other examples of PV induced papillomas and carcinomas and cancers caused by other viruses.
Exclusion of alternative explanations
In the early studies of HPV and cervical cancer, and currently in most studies, a fraction of cases are labelled as HPV negative and investigated under the hypothesis that HPV negative cases are a true biological entity.210,211 The proportion of such cases tends to be higher in studies of preinvasive neoplasia.212,213 As a consequence, there was some uncertainty in the interpretation of the results until the early 1990s.2,214,215 In many studies, HPV negative cases were frequently compared with HPV positive cases in relation to their epidemiological profile. In broad terms, it was clear that “HPV negative” cases retained the same traits as the rest of the cases (similar age, high number of sexual partners, young age at first sexual intercourse, long term use of contraceptives, high parity, etc). These results strongly suggested that the apparently HPV negative cases were also related to an STD pattern; however, none of the known sexually transmitted agents that had occasionally been associated with cervical cancer is able to satisfy the causality criteria outlined in table 1. In the past decade there has not been a hypothesis supported by sound epidemiological or biological data indicating that the aetiology of cervical cancer could be independent of HPV.
Exclusion of alternative explanations. Evaluation .
Alternative (non-HPV related) hypotheses to explain a fraction of cervical cancer are not being proposed. The hypothesis that a fraction of 5–10% of cases may occur in the absence of HPV should be retained for research purposes. Public health recommendations targeting a putative proportion of HPV negative cervical cancer cases are not supported by current results and are not justified.
Overall evaluation .
Systematic review of the causality criteria strongly indicates that the association of HPV and cervical cancer is causal in nature. The association is very strong, consistent, specific, and universal. HPV infection precedes preinvasive disease and the evidence for biological plausibility of the association is persuasive beyond reasonable doubt.
It should be retained as a scientific and research option that the existence of some non-HPV related cervical cancer cases is plausible. The grounds for such a statement rely on the following facts: (1) Epithelial cells are capable of developing into cancer cells and cancer growths in all human tissues regardless of a known, viral or non-viral, cause. Thus, cells in the human cervix might have this capability too. (2) Cell genes that are involved in HPV related carcinogenesis should be able to generate spontaneous or induced mutations leading to cancer in the absence of HPV. Available evidence suggests that this event is rare within the life expectation of the human population. (3) Relatively few cases of cervical cancer in very old women have been investigated. It is likely that the non-HPV related cancers currently occur very rarely and probably cluster in very old women. (4) Non-epithelial cancers do occur in the cervix at a low frequency.
ALTERNATIVE MODELS OF CERVICAL CANCER AETIOLOGY
This section will discuss in some detail the role of factors other than HPV in cervical cancer and evaluate them under Rothman's model of necessary and sufficient causality.
Other risk factors for cervical cancer
Most of the sexual behaviour parameters that were linked to cervical cancer in the past are being re-evaluated in studies that considered the strong influence of the presence of HPV biomarkers. Soon after the introduction of HPV testing into research protocols, it became clear that some of the key risk factors that reflected sexual behaviour, such as the number of sexual partners, merely reflected the probability of HPV exposure. Other factors, such as the estimates of age at first exposure (as indicated by age at first sexual intercourse or at first marriage) are still under evaluation. In addition, several environmental factors that were historically related to cervical cancer are currently being assessed. These include hormonal factors (use of OCs and multiparity) other STDs (HSV-2, Chlamydia trachomatis, and occasionally other STDs), cigarette smoking, and dietary factors. A special consideration should be given to exposure to HIV and to other situations of immunosuppression, which will not be dealt with in detail in this discussion.
Investigation of the role of such factors, once the central role of HPV was recognised, generated an analytical situation with few precedents in cancer epidemiology. This derived from the observation that HPV DNA was almost always present in specimens from cervical cancer. Moreover, in one large study it was shown that the HPV DNA negative cases that were identified were largely false negative cases, in which HPV DNA was initially undetected because of specimen inadequacy, a relative predominance of integrated HPV-18, or technological inadequacy.216 Therefore, it was thought inappropriate to allow in the statistical analyses a comparison group of “HPV negative” cases even if, in analytical terms, this group existed as a small fraction (between 5% and 10% of the cases) in most studies.
It soon became a standard procedure in the reports of case–control studies to include a separate analysis, or to restrict the analyses to HPV positive cases and controls, to assess the contribution of additional factors to the risk of cervical cancer.3,4,40,217 Given that, few studies were large enough to generate a sufficient number of HPV positive controls. In relation to invasive cervical cancer, the leading project was the multicentre case–control study on cervical cancer undertaken by the IARC in 1991. The characteristics of the protocol, testing system, and some of the key results have been described in the country specific publications.3,24–30,218,219 The pooled analyses for each risk factor will support their conclusions on analysis restricted to HPV positive cases and controls. For this discussion, we will summarise the key preliminary findings.
Oral contraceptives
The IARC multicentre study included 1768 cases and 262 controls that were positive for HPV DNA. OC use “ever” was associated with a significant increase in risk (OR = 1.47; 95% CI, 1.02 to 2.12). Use of OCs for less than five years was not related to cervical cancer (OR = 0.77; 95% CI, 0.46 to 1.29). The risk increased for five to nine years of use (OR = 2.72; 1.36 to 5.46) and for more than 10 years (OR = 4.48; 2.24 to 9.36). The conclusion of this analysis indicates that the use of OCs for five or more years is a cofactor that increases up to fourfold the risk of cervical cancer among women who are carriers of HPV DNA. These results provide a consistent summary of the previous publications of the individual studies included in the multicentre project.220
The evidence for an association of cervical cancer with the use of oral or other hormonal contraceptives is not entirely consistent. Several studies that investigated HPV positive women found no associations or only weak associations in subgroup analyses.4,5,217,221,222 These apparently conflicting results may reflect the increased cytological surveillance of women who are taking OCs in developed countries and the use of different case definitions (from ASCUS up to HSIL/CIN 3 as opposed to cervical cancer) in cohort studies.
The IARC monograph programme reviewed the evidence for OCs and concluded that, for the associations with cervical cancer, biases related to sexual behaviour, screening, and other factors could not be ruled out as possible alternative explanations. One of the difficulties encountered in the conduct and analysis of epidemiological studies is the proper assessment, through questionnaires, of the correlates of HPV exposure (sexual behaviour) and screening history. However, OCs were evaluated as human carcinogens (class 1) by the monograph because of the evidence linked to liver cancer.223
Because of the potential public health importance of confirming an interaction between the long term use of OCs and HPV infections in the development of cervical cancer, efforts are now being devoted to confirm the results in different populations.
Parity
In the IARC multicentre study, HPV positive women who reported seven or more full term pregnancies had a fourfold increased risk of cervical cancer compared with similar HPV positive women who were nulliparous (OR, 3.8; 95% CI, 2.7 to 5.5). There was still a twofold increased risk when women reporting seven or more pregnancies were compared with HPV positive women who reported one to two full term pregnancies.224
Similar results were obtained in Costa Rica,225 Thailand,5 and among women with preinvasive disease in the Portland study.4 In Denmark and in the Manchester cohort study, two populations with low parity,217,226 the effects were less visible. In another high parity country—Honduras—the effects of parity were not significant among the HPV positive cases and controls.227
Smoking
Smoking has been related to cervical cancer since the late 1970s, based upon the correlations seen between cervical cancer incidence and the incidence of other tobacco related cancers.228 The 1986 IARC monograph on smoking considered that the evidence available for cervical cancer was insufficient to rule out confounding with sexual behaviour traits, strongly related to both smoking and cervical cancer.229 An extensive review of the relation between smoking and cervical cancer was published in 1998, including eight cohort and 44 case–control studies. The report concluded that the association was largely consistent in studies that adjusted for HPV DNA or restricted analyses to HPV positive women. The magnitude of the risk for current smokers was of the order of one to threefold; the ORs tended to be higher in more advanced preinvasive neoplasia, and in several studies a dose–response relation with the amount of tobacco consumed was seen.230 A recent review of the evidence conducted by the Surgeon General in the USA retained the hypothesis that a causal association between cigarette smoking and cervical cancer was plausible. However, the report indicated that the extent to which cigarette smoking could be considered independent of HPV could not be definitively assessed.231
Restricting the review to studies that evaluated HPV exposed women, the preliminary pooled results of the IARC multicentre study found that “ever smoking” was associated with a twofold, significantly increased risk of cervical cancer, with a significant dose–response (M Plummer et al, unpublished, 2002). These findings are consistent with those found for “current v never smoking” among HPV positive women in the Costa Rica study (OR = 2.3),225 the Portland study (OR = 2.7 for CIN 2–3),4 the Copenhagen study (OR = 1.9),232 and the Manchester study (OR = 2.2).217 These recent studies are providing growing evidence on the carcinogenic effect of cigarette smoking in women with HPV infection. However, the mechanisms by which cigarette smoking may affect cervical cancer (such as a direct effect of the tobacco metabolites, or an indirect effect related to tobacco induced immunosupression or to reduced dietary antioxidants) remain elusive and further studies are warranted.230
The general considerations in relation to any of the cofactors considered and the carcinogenic effects of HPV are threefold. First, in the analyses restricted to HPV positive women, the magnitude of the RR estimates are moderate (range 2 to 6 for extreme categories of exposure) for any of the variables when compared with the risk estimates for HPV (ranges 50 to > 500). Second, the results in the literature concerning these factors remain inconsistent, again in contrast to the striking consistency of the associations found for HPV DNA. Third, the interpretation of the risk estimates for cofactors should consider that, as far as we understand them today, these are conditional effects that apply if, and perhaps only if, HPV DNA is present in the specimen. Therefore, there is no convincing evidence that any of the three factors discussed are truly independent risk factor for cervical cancer. Some authors view these results (in conjunction with the risk analyses of HPV exposure) as indicative of a promoter effect of OC use, smoking, or multiparity from HPV infections to HPV related neoplasia.
Other factors
The role of additional factors is being actively investigated. Age at exposure has been shown to be a strong determinant of the prognosis of a carcinogenic viral infection in relation to cancer development. For example, HBV induced liver cancer is closely related to age at infection, with the strongest risk linked to infections occurring within the perinatal period.233,234 The prognosis of the EBV infection in relation to Burkitt's lymphoma is related to age at first infection and probably to the concurrent exposure to malaria.235 Similarly, most studies have shown that the risk of cervical cancer is related to age at first sexual intercourse. More recent studies that included HPV measurements have shown age at first intercourse to be a surrogate measure of age at first HPV exposure. However, definite evidence that cervical cancer progression is linked to age at first HPV exposure has not been provided. It has been proposed that the developing cervix (at the age of peri-menarche) or the healing cervix (as a consequence of deliveries, cervical trauma, or any other STD infection) are high risk situations for an HPV infection to reach the basal layer and establish a persistent infection.
Some STDs, including HIV,12,42 have repeatedly been found to be associated with cervical cancer. The multicentre study found a twofold increased risk for the presence of antibodies to C trachomatis (OR = 2.1; 95% CI, 1.1 to 4.0).236 Antibodies to HSV-2218,236 and non-specific inflammatory changes237 have also been related to modest increases in risk among HPV positive women. Other environmental risk factors under evaluation are socioeconomic status238 and nutritional factors.239
Limitations of the evidence
One limitation of the available studies and of the summary presented here is the crudeness of information available on variables that may modulate the effect. This makes it difficult to explain in finer detail the geographical variation in cervical cancer incidence and the variability in risk estimates reported in different populations. For example, the inconsistencies in finding associations of cervical cancer with the use of OCs may be explained by factors related to the intensity, duration, or the chemical composition of the exposure. Factors that are largely country specific, such as the variability in time since widespread introduction, availability of combined versus sequential products, oestrogen/progesterone doses, etc, could be important determinants; yet these would only partially account for the associations observed.
A second limitation is that many studies did not consider host factors in relation to HPV. Human major histocompatibility complex (HLA) types and p53 polymorphisms are being actively investigated because of the indication that they may play a role in the natural history of HPV infections.158,240 The putative effect of such individual susceptibility factors is not adjusted for in the risk analyses of the environmental factors. However, at this stage, there is limited information to substantiate an effect of these host factors as independent of HPV.241–244
There is a clear need to pursue research in understanding the factors that determine whether a woman with an HPV infection will clear the infection or become a persistent carrier. Furthermore, studies are still needed to explore whether additional factors play a role in determining neoplastic progression and how best to use them in screening and patient management.
Likely components of sufficient causes of cervical cancer
The purpose of this section is to try to substantiate the components of plausible sufficient causes of cervical cancer according to Rothman's scheme,15 and based upon data from large series of cases examined with reliable HPV DNA testing systems. In the literature on cervical cancer, the independent risk factors that have been repeatedly identified and at least partially confirmed by some of the most recent studies could be simplified to a dichotomous categorisation (table 5).
Table 5.
Risk factors for cervical cancer among human papillomavirus positive women*
| Risk factor | Risk exposure | Ref |
| HPV DNA in cervial exfoliates | Positive for high risk types | Negative |
| Use of oral contraceptives | 5 or more years of use | Never |
| Smoking | Ever | Never |
| Parity | 5 or more pregnancies | None or 1–2 |
*References adapted from the results of the IARC multicentre study.23
Table 6 shows the distribution of approximately 2500 cases of invasive cervical cancer from over 25 countries classified according to their exposure to every possible combination of the four factors considered above. Approximately 1500 of these cases were included in the IARC multicentre study (table 6, study 1). Two of the study sites (Colombia and Spain) have been removed from the series because HPV testing was performed with the early MY09/11 PCR system. The remaining study sites were investigated using the GP5+/6+ PCR, which has higher sensitivity for some HPV types (see also HPV-DNA prevalence by study site in fig 3). Table 6 also includes an equivalent distribution for 800 cases included in the international biological study on cervical cancer (IBSCC), analysed with a sequential combination of both techniques. Study 2 in table 6 presents the distribution of the first testing exercise with the MY09/11system34 and study 3 presents the distribution of the same cases when the second testing round with GP5+/6+ and CPI/II for the HPV negative cases was completed.216
Table 6.
Prevalence of four risk factors in 1490 cases of invasive cervical cancer included in the IARC multicentre case–control study12 and approximately 800 cases included in the IBSCC tested for human papillomavirus (HPV) DNA in 1995 and 1999
| Study 1 Multicentric | Study 2 IBSCC (1995) | Study 3 IBSCC (1999) | ||||
| Presence of risk factor | N | % | N | % | N | % |
| HPV | 341 | 22.9 | 186 | 23.1 | 186 | 23.1 |
| HPV + OC | 54 | 3.6 | 25 | 3.1 | 25 | 3.1 |
| HPV + Smk | 115 | 7.7 | 96 | 11.9 | 978 | 12.0 |
| HPV + Preg | 587 | 39.4 | 302 | 37.5 | 322 | 40.0 |
| HPV + OC + Smk | 20 | 1.3 | 25 | 3.1 | 28 | 3.5 |
| HPV + OC + Preg | 72 | 4.8 | 14 | 1.7 | 16 | 2.0 |
| HPV + Smk + Preg | 223 | 15.0 | 82 | 10.2 | 88 | 10.9 |
| HPV + OC + Smk + Preg | 21 | 1.4 | 7 | 0.9 | 7 | 0.9 |
| OC | 2 | 0.1 | 0 | 0 | 0 | 0 |
| OC + Smk | 0 | 0 | 3 | 0.4 | 0 | 0 |
| OC + Preg | 0 | 0 | 2 | 0.2 | 0 | 0 |
| OC + Smk + Preg | 0 | 0 | 0 | 0 | 0 | 0 |
| Smk | 8 | 0.5 | 1 | 0.1 | 0 | 0 |
| Smk + Preg | 9 | 0.6 | 6 | 0.7 | 0 | 0 |
| Preg | 15 | 1.0 | 21 | 2.61 | 1 | 0.1 |
| None of the four | 23 | 1.5 | 25 | 3.1 | 2 | 0.2 |
| Total number of cases | 1490 | 100 | 806* | 100 | 806* | 100 |
*The total number in the column is not 806 because of missing values in some of the variables. References: study 1, Muñoz et al (2000)32; study 2, Bosch et al (1995)34; study 3, Walboomers et al (1999).216
HPV, HPV DNA positive; OC, duration of use of hormonal contraceptives >6 years; Preg, ≥5 pregnancies (live or still born); Smk, smoker (ever). IARC, International Agency for Research on Cancer; IBSCC, international biological study on cervical cancer.
Using these distributions as a realistic guide, some theoretically sufficient causal models could be proposed as plausible for cervical cancer (table 7).
Table 7.
Theoretical models of sufficient causes for cervical cancer and environmental risk factors
| Sufficient cause Model 1 | Sufficient cause Model 2 | Sufficient cause Model 3 | Sufficient cause Model 4 |
| HPV DNA in cervical exfoliates | HPV DNA in cervical exfoliates and any other combination of factors | High parity Smoking | None of the four factors |
HPV, human papillomavirus.
Each combination of factors as described could theoretically lead to cervical cancer and, under each model, the occurrence of the disease may be further modulated by the presence or absence of the additional factors. These may determine parameters such as the age of onset, the aggressiveness, or other characteristics of tumour behaviour.
Some of the categories in table 6 are compatible with the hypothesis that a fraction of cases of cervical cancer (4–7%) are independent of HPV and even that some 1–2% are independent of the four environmental risk factors considered in table 6, either alone or in combination. To explain these groups, two alternatives could be considered.
The first alternative is that some cervical cancer cases truly occur unrelated to any of the combinations of the four factors considered. Some previous analyses that have compared the epidemiological profile of HPV positive and apparently HPV negative women with cervical cancer did not find significant differences in their sexual or reproductive behaviour. These types of analyses were reported at the time that HPV DNA detection technology was of limited sensitivity and 30–40% of cervical cancer cases were reported as HPV negative.3 Therefore, the HPV unrelated hypothesis would argue in favour of a role for other STDs. Current results of some major studies found small and still inconsistent effects from previous exposures to C trachomatis236,245,246 and/or HSV-2 infections (J Smith et al, unpublished data, 2002). However, these effects are mostly seen in the presence of HPV DNA.
Conversely, the distributions presented in table 6 may still suffer from misclassification of any of the variables considered, notably of HPV. A particularly relevant exercise was undertaken to verify technical HPV misclassification with the cases included in the IBSCC study (studies 2 and 3 of table 6). After the key results were published reporting an HPV DNA prevalence of 93.0%,34 the apparently HPV negative cases were further investigated. The second level evaluation included: (1) A comparison of the serological and epidemiological profiles of the “HPV DNA negatives” compared with the “HPV DNA positives”. (2) The pathology of the specimen was reviewed. Furthermore, serial cuts from the paraffin wax blocks were used to ensure that the specimen used for HPV DNA testing included neoplastic tissue. (3) A different technology was used for HPV DNA testing using shorter primers in the E7 region and two sets of consensus primers (CPI/II and GP5+/6+). In brief, the results of the study indicated that most of the HPV negative cases were in fact HPV positive, and that the HPV types newly identified were the common types, with an over-representation of HPV-18.216 The distribution of risk factors in study 3 of table 6 thus represents the conclusion of the large IARC effort in HPV and cervical cancer. Based upon the final results of this study and the considerable body of evidence accumulated from other studies at the time, it was proposed that HPV DNA is a necessary cause of cervical cancer and that HPV DNA belongs to (is a component of) all reasonably conceived environmental sufficient causes.
The key consideration from this discussion, however, is that with the current degree of understanding it would be difficult to justify an aetiological model that would not include HPV DNA for most cervical cancer cases occurring worldwide. On these grounds, HPV fulfils the criteria of a necessary cause of cervical cancer.
The second qualifier of the evaluation in Rothman's scheme refers to the sufficient criteria. From natural history studies, it is clear that a large fraction of HPV infections occur as a self limiting subclinical process with little impact on morbidity. The exceptions are the fraction of infected women in whom HPV persistence is established, and in whom the risk of cervical neoplasia increases significantly. Because of the large pool of infections that will not progress to cancer, it is usually accepted that HPV is not a sufficient cause of disease (it is noteworthy that no accepted cause of cancer has ever been considered as sufficient). The implication has been that other factors that modulate the evolution of the relevant HPV infection are intervening. However, specific evidence on the nature of these factors is elusive.
From the data in tables 6 and 7 it is clear that in a fair number of cases HPV is the only environmental factor identified of the four evaluated. This accounts for 23% (341 of 1490) of the cases in the multicentre study and 23% (186 of 806) of the cases in the IBSCC study. It is thus plausible that in perhaps one quarter of cases, the additional factors that modulate the host response to HPV are not the environmental factors usually linked to cervical cancer. It is probable that some of the host response mechanisms to the virus are the determinants of the prognosis of a given infection to either spontaneous resolution or to viral persistence and neoplastic progression.
The identification and natural history of biomarkers related to the immune response and host susceptibility to HPV is a subject under active research. Likewise, the criteria of causality outlined in table 1 may require a revision to integrate criteria for host responses in addition to the canopy of environmental risk factors.
Likely components of sufficient causes of cervical cancer. Evaluation .
HPV is a necessary, non-sufficient cause of cervical cancer. In perhaps a quarter of a large series of cervical cancer cases, HPV was the only environmental risk factor identified. It is likely that the additional factors that combine with HPV to complete a sufficient cause in such cases are of endogenous rather than of environmental nature.
RECOGNITION OF THE CAUSAL LINK BETWEEN HPV DNA AND CERVICAL CANCER
The evidence for a qualification of the association between cervical cancer and HPV DNA as causal and the justification for intervention strategies based upon this conclusion were debated in the late 1980s and early 1990s. At the time, the HPV testing systems suitable for use in large epidemiological studies had limited sensitivity and specificity. The results generated were difficult to interpret and skepticism was overtly expressed in the international literature.2,55,72,214,215,226,247,248 The discussion initiated at the time to decide on the right time to make public health decisions is an ongoing process with occasional spikes.249,250 Some of the landmarks that may be used as examples are the scientific publications coordinated by the IARC that involved a large number of scientists dedicated to HPV research.
In 1989, one IARC scientific publication still retained the hypothesis that HPV DNA could be a passenger and that superinfection of the neoplastic tissue could not be safely ruled out as an alternative explanation.251 In 1992, a follow up publication again reviewed the evidence and concluded that previous incoherent epidemiological results could be explained by measurement errors in HPV detection. The review concluded that bias, chance, or confounding in the epidemiological studies could be safely ruled out and that the association could be considered causal in nature.252 In 1995, a formal IARC monograph was convened to review available evidence for HPV and cervical cancer and concluded that HPV-16 and HPV-18 were carcinogenic to humans and the two types were classed as group 1 carcinogens.12
The conclusion of the 1995 monograph was subsequently endorsed by the scientific community at large, which uses the IARC's reference widely as the standard for causality. Other relevant bodies have undertaken similar exercises and have consistently reached similar conclusions. These include the Centers for Disease Control, the National Cancer Institute (National Institutes of Health), the American Cancer Society (Cervical Cancer Resource Center), the American College of Obstetricians and Gynecologists, the US Department of Health and Human Services, the Program for Appropriate Technology in Health, the World Health Organisation, the European Research Organisation on Genital Infection and Neoplasia, and the Health Technology Assessment of the UK, among others.
In addition to the formal reviews by institutional groups, individual scientists and peer reviewed journals have repeatedly expressed their understanding on the causal nature of the association between HPV and cervical cancer.4,17,37,119,133,141,183,216,217,225,253–273
From evidence to decisions
Decision making in public health is a process that uses scientific evidence in addition to judgment and socioeconomic considerations. The turning point at which public health decisions are taken and enforced as opposed to recommending additional research is often elusive. The role of scientists in influencing such decisions is also debatable (for an extensive review see the special edition of the American Journal of Epidemiology274).
Rothman's textbook describes a rather extreme dichotomy between scientists and public health policy makers:
“Lanes (1985)275 has proposed that causal inference is not part of science at all, but lies strictly in the domain of public policy. According to this view, since all scientific theories could be wrong, policy makers should weigh the consequences of actions under various theories. Scientists should inform policy makers about scientific theories, and leave the choice of a theory and an action to policy makers. Not many public health scientists are inclined toward such a strict separation between science and policy, but as a working philosophy, it has the advantage of not putting scientists in the awkward position of being advocates for a particular theory.276 Indeed, history shows that skepticism is preferable in science.”19
The field of cervical cancer prevention is now in an active phase of evaluation of novel technologies, to increase the efficiency of screening in developed populations and to offer realistic options to populations that do not benefit from cytology based organised programmes. The recognition that HPV is the causal agent of cervical cancer worldwide is a landmark achievement that sets the grounds for qualitative progress. Current efforts in cervical cancer prevention in relation to HPV are focusing first on the evaluation of protocols for HPV testing in the context of established screening programmes, secondly on developing HPV vaccines for the prevention and treatment of HPV infections, and thirdly on the development of HPV treatments.
CONCLUSION
At the current level of knowledge, the causal role of persistent HPV infections in the development of cervical cancer and its precursors has been proved beyond reasonable doubt. A large number of human studies have been conducted following standard criteria that reasonably excluded bias, chance, and confounding in the estimation of the risk. The evidence available at this time is consistent with the established criteria of causality. The association of HPV with cervical cancer has been proposed as the first ever described necessary cause of a human cancer.
At the turning point following a major discovery in the origin of cervical cancer, it is the responsibility of the public health administrators to judge when the scientific evidence is sufficient to take action and promote changes in medical practice.
Selected quotes from Sir Bradford Hill, subsequently endorsed by MacMahon and Pugh,11 Weed ,10 and Rothman,19 may illustrate the current situation in relation to the adoption of HPV testing as a relevant strategy for the prevention and management of cervical neoplasia.
“ Finally, like Hill before them, they (MacMahon and Pugh) believed that `proof' of cause was elusive, and in the face of controversy, the crucial decision was one involving the point at which prudence should reign and action should be taken, rather than waiting for more evidence.”
“The failure of some researchers to recognise the theoretical impossibility of `proving' the causal nature of an association has led to fruitless debates pitting skeptics who await such proof against scientists who are persuaded to make an inference on the basis of existing evidence.”
The responsibility of scientists for making causal judgments was Hill's final emphasis in his discussion of causation:
“All scientific work is incomplete—whether it be observational or experimental. All scientific work is liable to be upset or modified by advancing knowledge. That does not confer upon us a freedom to ignore the knowledge we already have, or to postpone the action that it appears to demand at a given time.”
Acknowledgments
This work has been partially supported by research grant FIS 01/1237 and a non-restricted collaborative research agreement between the Institut Català d'Oncologia (ICO) in Barcelona, Spain and Digene Corporation in Gaithersburg, Maryland, USA.
Advanced versions of this text have been reviewed by a number of researchers in the field of the viral aetiology of cervical cancer. Their comments and contributions are deeply appreciated: LA Brinton, National Cancer Institute, Bethesda, USA; TR Broker, University of Alabama, Birmingham, USA; RD Burk, Albert Einstein College of Medicine, New York, USA; X Castellsagué, Catalan Institute of Oncology, Barcelona, Spain; J Cuzick, Imperial Cancer Research Foundation, London, UK; S de Sanjosé, Catalan Institute of Oncology, Barcelona, Spain; M Del Vecchio, Digene Corporation, Gaithesburg, USA; ELF Franco, McGill University, Montreal, Canada; S Franceschi, International Agency for Research on Cancer, Lyon, France, I Frazer, Center for Immunology and Cancer Research, Brisbane, Australia; R Herrero, Proyecto Epidemiológico Guanacaste, San Jose, Costa Rica; S Krüger Kjaer, Danish Cancer Society, Copenhagen, Denmark; CJN Lacey, Imperial College School of Medicine, London, UK; DR Lowy, National Institutes of Health, Bethesda, USA; V Moreno, Catalan Institute of Oncology, Barcelona, Spain; A Muñoz, John Hopkins School of Hygiene and Public Health, Baltimore, USA; M Plummer, International Agency for Reasearch on Cancer, Lyon, France; WC Reeves, Centers for Disease Control and Prevention, Atlanta, USA; M Schiffman, National Cancer Institute, Bethesda, USA; JT Schiller, National Cancer Institute, Bethesda, USA; H-R Shin, National Cancer Centre Research Institute, Kyonggi, Korea; J Smith, International Agency for Research on Cancer, Lyon, France; PJF Snijders, Vrije Universiteit Medical Center, Amsterdam, The Netherlands; BM Steinberg, Long Island Jewish Hillside Medical Center, New York, USA; MH Stoler, University of Virginia, Charlottesville, USA; D Thomas, Fred Hutchinson Cancer Research Center, Seattle, USA; H Vainio, International Agency for Research on Cancer, Lyon, France; AJ van den Brule, Free University Hospital, Amsterdam, The Netherlands; LL Villa, Ludwig Institute for Cancer Research, Sao Paulo, Brazil; TC Wright, Columbia University, New York, USA. Many other researchers have contributed to understanding cervical cancer aetiology and to this review with their work, presentations at meetings, and coffee break discussions. We are grateful to them and hope this review is of use to anyone involved in the task of cervical cancer prevention. Many thanks to M Diaz and E Guinó for statistical support and to C Rajo and M Gonzalez, for secretarial help.
Abbreviations
AF, attributable fraction
ASCUS, atypical squamous cells of undetermined significance
CI, confidence interval
CIN, cervical intraepithelial neoplasia
EBV, Epstein-Barr virus
GP, general primer
HCV, hepatitis C virus
HIV, human immunodeficiency virus
HPV, human papillomavirus
HSIL, high grade squamous intraepithelial lesion
HSV-2
type 2 herpes simplex virus
IARC, International Agency for Research on Cancer
IBSCC, international biological study on cervical cancer
OC, oral contraceptive
OR, odds ratio
ORF, open reading frame
Pap, Papanicolaou
PF, protective fraction
PCR, polymerase chain reaction
RB, retinoblastoma
RR, relative risk
STD, sexually transmitted disease
Th1, T helper cell type 1
Footnotes
This paper is dedicated to the memory of the late Jan M M Walboomers.
REFERENCES
- 1.Peto R, zur Hausen H, eds. Viral origin of cervical cancer. Bambury report no. 21, New York: Cold Spring Harbor CSH Press, 1986.
- 2.Franco EL. The sexually transmitted disease model for cervical cancer: incoherent epidemiologic findings and the role of misclassification of human papillomavirus infection. Epidemiology 1991;2:98–106. [PubMed] [Google Scholar]
- 3.Bosch FX, Muñoz N, de Sanjosé S, et al. Risk factors for cervical cancer in Colombia and Spain. Int J Cancer 1992;52:750–58. [DOI] [PubMed] [Google Scholar]
- 4.Schiffman MH, Bauer HM, Hoover RN, et al. Epidemiologic evidence showing that human papillomavirus infection causes most cervical intraepithelial neoplasia. J Natl Cancer Inst 1993;85:958–64. [DOI] [PubMed] [Google Scholar]
- 5.Thomas DB, Ray RM, Koetsawang A, et al. Human papillomaviruses and cervical cancer in Bangkok. I. Risk factors for invasive cervical carcinomas with human papillomavirus types 16 and 18 DNA. Am J Epidemiol 2001;153:723–31. [DOI] [PubMed] [Google Scholar]
- 6.Lilienfeld AM. On the methodology of investigations of etiologic factors in chronic disease—some comments. J Chronic Dis 1959;10:41–6. [DOI] [PubMed] [Google Scholar]
- 7.Sartwell PE. On the methodology of investigations of etiologic factors in chronic disease—further comments. J Chronic Dis 1960;11:61–3. [DOI] [PubMed] [Google Scholar]
- 8.Hill AB. The environment and disease: association or causation? Proc R Soc Med 1965;58:295–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Surgeon General's Advisory Committee on Smoking and Health. DHEW publication no. (PHS) 1103. MD, USA: US Public Health Service, 1964.
- 10.Susser M. Causal thinking in the health sciences. New York: Oxford University Press, 1973.
- 11.MacMahon B, Pugh TF. Concepts of causes. In: Epidemiology: principles and methods. Boston: Little, Brown, 1970:17–29.
- 12.IARC. Human papillomaviruses. IARC monographs on the evaluation of carcinogenic risks to humans, Vol. 64. Lyon: IARC, 1995. [PMC free article] [PubMed]
- 13.Weed DL. Causal and preventive inference. In: Greenwald P, Kramer BS, Weed DL, eds. Cancer prevention and control. New York: M Dekker, 1995:285–302.
- 14.Evans AS. Causation and disease: the Henle-Koch postulates revisited. Yale J Biol Med 1976;49:175–95. [PMC free article] [PubMed] [Google Scholar]
- 15.Rothman KJ. Causes. Am J Epidemiol 1976;104:587–92. [DOI] [PubMed] [Google Scholar]
- 16.Shah KV, Howley PM. Papillomaviruses. In: Knipe DM, Howley PM, eds. Fields virology. Philadelphia: Lippincott-Raven, 1996:2077–109.
- 17.zur Hausen H. Papillomavirus causing cancer: evasion from host-cell control in early events in carcinogenesis. J Natl Cancer Inst 2000;92:690–98. [DOI] [PubMed] [Google Scholar]
- 18.Rothman KJ. Reviews and commentary. Causes. Am J Epidemiol 1995;104:90–5. [Google Scholar]
- 19.Rothman KJ. Causal inference in epidemiology. In: Rothman KJ. Modern epidemiology. Boston, Toronto: Little, Brown and Company, 1986:7–23.
- 20.Gravitt PE, Manos MM. Polymerase chain reaction-based methods for the detection of human papillomavirus DNA, Vol. 119. Lyon: IARC Scientific Publications, 1992. [PubMed]
- 21.van den Brule AJC, Meijer CJLM, Bakels V, et al. Rapid human papillomavirus detection in cervical scrapes by combined general primer mediated and type-specific polymerase chain reaction. J Clin Microbiol 1991;28:2739–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.de Roda Husman AM, Walboomers JMM, van den Brule AJC, et al. The use of general primers GP5 and GP6 elongated at their 3` ends with adjacent highly conserved sequences improves human papillomavirus detection by polymerase chain reaction. J Gen Virol 1995;76:1057–62. [DOI] [PubMed] [Google Scholar]
- 23.Bosch FX, Rohan T, Schneider A, et al. Papillomavirus research update: highlights of the Barcelona HPV 2000 international papillomavirus conference. J Clin Pathol 2001;54:163–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Muñoz N, Bosch FX, de Sanjosé SM, et al. The causal link between human papillomavirus and invasive cervical cancer: a population-based case-control study in Colombia and Spain. Int J Cancer 1992;52:743–9. [DOI] [PubMed] [Google Scholar]
- 25.Eluf-Neto J, Booth M, Muñoz N, et al. Human papillomavirus and invasive cervical cancer in Brazil. Br J Cancer 1994;69:114–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chaouki N, Bosch FX, Muñoz N, et al. The viral origin of cervical cancer in Rabat, Morocco. Int J Cancer 1998;75:546–54. [DOI] [PubMed] [Google Scholar]
- 27.Rolón PA, Smith JS, Muñoz N, et al. Human papillomavirus infection and invasive cervical cancer in Paraguay. Int J Cancer 2000;85:486–91. [PubMed] [Google Scholar]
- 28.Ngelangel C, Muñoz N, Bosch FX, et al. Causes of cervical cancer in the Philippines: a case-control study. J Natl Cancer Inst 1998;90:43–9. [DOI] [PubMed] [Google Scholar]
- 29.Chichareon S, Herrero R, Muñoz N, et al. Risk factors for cervical cancer in Thailand: a case control study. J Natl Cancer Inst 1998;90:50–7. [DOI] [PubMed] [Google Scholar]
- 30.Santos C, Munoz N, Klug S, et al. HPV types and cofactors causing cervical cancer in Peru. Br J Cancer 2001;85:966–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Woodman CB, Collins S, Winter H, et al. Natural history of cervical human papillomavirus infection in young women: a longitudinal cohort study. Lancet 2001;357:1831–6. [DOI] [PubMed] [Google Scholar]
- 32.Muñoz N, Bosch FX, Chichareon S, et al. A multinational case-control study on the risk of cervical cancer linked to 25 HPV types: which are the high-risk types? In: Castellsagué X, Bosch FX, de Sanjosé S, et al, eds. 18th International Papillomavirus Conference—program and abstracts book. Barcelona: Thau SL, 2000:125 (available on line: http:/www.hpv2000.com).
- 33.Bosch FX, Muñoz N, Chichareon S, et al. HPV and cervical adenocarcinoma: an IARC based multicentric case-control study. In: Castellsagué X, Bosch FX, de Sanjosé S, et al, eds. 18th International Papillomavirus Conference—program and abstracts book. Barcelona: Thau SL, 2000:131 (available on line: http:/www.hpv2000.com).
- 34.Bosch FX, Manos MM, Muñoz N, et al. Prevalence of human papillomavirus cervical cancer: a worldwide perspective. J Natl Cancer Inst 1995;87:796–802. [DOI] [PubMed] [Google Scholar]
- 35.Castellsagué X, Menéndez C, Loscertales M-P, et al. Human papillomavirus genotypes in rural Mozambique. Lancet 2001;358:1429–30. [DOI] [PubMed] [Google Scholar]
- 36.Herrero R, Muñoz N, Lazcano E, et al. HPV International prevalence surveys in general populations. In: Castellsagué X, Bosch FX, de Sanjosé S, et al, eds. 18th International Papillomavirus Conference—program and abstracts book. Barcelona: Thau SL, 2000:126 (available on line: http:/www.hpv2000.com).
- 37.Herrero R, Hildesheim A, Bratti C, et al. Population-based study of human papillomavirus infection and cervical neoplasia in rural Costa Rica. J Natl Cancer Inst 2000;92:464–74. [DOI] [PubMed] [Google Scholar]
- 38.Thomas DB, Quin Q, Kuypers J, et al. Human papillomaviruses and cervical cancer in Bangkok. II. Risk factors for in situ and invasive squamous cell cervical carcinomas. Am J Epidemiol 2001;153:732–8. [DOI] [PubMed] [Google Scholar]
- 39.Olsen AO, Gjoen K, Sauer T, et al. Human papillomavirus in cervical intraepithelial neoplasia grade II-III: a population-based case-control study. Int J Cancer 1995;61:312–15. [DOI] [PubMed] [Google Scholar]
- 40.Kjaer SK, Van den Brule AJC, Boch JE, et al. Human papillomavirus—the most significant risk determinant of cervical intraepithelial neoplasia. Int J Cancer 1996;65:601–6. [DOI] [PubMed] [Google Scholar]
- 41.de Sanjose S, Valls I, Cañadas MP, et al. Infección por los virus del papiloma humano y de la inmunodeficiencia humana como factores de riesgo para el cáncer de cuello uterino en mujeres reclusas. Med Clin (Barc) 2000;115:81–4. [DOI] [PubMed] [Google Scholar]
- 42.Palefsky JM, Minkoff H, Kalish LA, et al. Cervicovaginal human papillomavirus infection in human immunodeficiency virus-1 (HIV)-positive and high-risk HIV-negative women. J Natl Cancer Inst 1999;91:226–36. [DOI] [PubMed] [Google Scholar]
- 43.Beasley RP, Lin CH, Hwang L-Y, et al. Hepatocellular carcinoma and hepatitis B virus. A prospective study of 22 707 men in Taiwan. Lancet 1981;21:1129–31. [DOI] [PubMed] [Google Scholar]
- 44.Kuper HE, Tzonou A, Kaklamari E, et al.Hepatitis B and viruses in the etiology of hepatocellular carcinoma; a study in Greece using third-generation assays: Cancer Causes Control 2000;11:171–5. [DOI] [PubMed] [Google Scholar]
- 45.Donato F, Tagger A, Chiesa R, et al. Hepatitis B and C virus infection, alcohol drinking, and hepatocellular carcinoma: a case-control in study Italy. Hepatology 1997;26:579–84. [DOI] [PubMed] [Google Scholar]
- 46.Peto R, Darby S, Deo H, et al. Smoking, smoking cessation, and lung cancer in the UK since 1950: combination of national statistics with two case-control studies. BMJ 2000;321:323–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lee M-S, Kim D-H, Kim H, et al. Hepatitis B vaccination and reduced risk of primary liver cancer among male adults: a cohort study in Korea. Int J Epidemiol 1998;27:316–19. [DOI] [PubMed] [Google Scholar]
- 48.Chang M-H, Chen CH-J, Lai M-S, et al. Universal hepatitis B vaccination in Taiwan and the incidence of hepatocellular carcinoma in children. N Engl J Med 1997;336:1855–907. [DOI] [PubMed] [Google Scholar]
- 49.Moreno V, Muñoz N, Bosch FX, et al. Risk factors for progression of cervical intraepithelial neoplasm grade III to invasive cervical cancer. Cancer Epidemiol Biomarkers Prev 1995;4:459–67. [PubMed] [Google Scholar]
- 50.Asato T, Nakajima Y, Nagamine M, et al. Correlation between the progression of cervical dysplasia and the prevalence of human papillomavirus. J Infect Dis 1994;169:940–1. [DOI] [PubMed] [Google Scholar]
- 51.Shen C-Y, Ho M-S, Chang S-F, et al. High rate of concurrent genital infections with human cytomegalovirus and human papillomaviruses in cervical cancer patients. J Infect Dis 1993;168:449–52. [DOI] [PubMed] [Google Scholar]
- 52.Arends MJ, Donaldson YK, Duval E, et al. Human papillomavirus type 18 associates with more advanced cervical neoplasia than human papillomavirus type 16. Hum Pathol 1993;24:432–7. [DOI] [PubMed] [Google Scholar]
- 53.Das BC, Sharma JK, Gopalkrishna V, et al. A high frequency of human papillomavirus DNA sequences in cervical carcinomas of Indian women as revealed by Southern blot hybridization and polymerase chain reaction. J Med Virol 1992;36:239–45. [DOI] [PubMed] [Google Scholar]
- 54.Ter Meulen J, Eberhardt HC, Luande J, et al. Human papillomavirus (HPV) infection, HIV infection and cervical cancer in Tanzania, East Africa. Int J Cancer 1992;51:515–21. [DOI] [PubMed] [Google Scholar]
- 55.Muñoz N, Bosch FX. HPV and cervical neoplasia: review of case-control and cohort studies. In: Muñoz N, Bosch FX, Shah KV, et al, eds. The epidemiology of cervical cancer and human papillomavirus. Lyon: IARC Scientific Publications No. 119, 1992:251–6. [PubMed]
- 56.Peng HQ, Liu Sl, Mann V, et al. Human papillomavirus types 16 and 33, herpes simplex virus type 2 and other risk factors for cervical cancer in Sichuan Province, China. Int J Cancer 1991;47:711–16. [DOI] [PubMed] [Google Scholar]
- 57.Griffin NR, Bevan IS, Lewis FA, et al. Demonstration of multiple HPV types in normal cervix and in cervical squamous cell carcinoma using the polymerase chain reaction on paraffin wax embedded material. J Clin Pathol 1990;43:52–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Marin J, Ursic Vrscaj M, Erzen M. Detection of human papillomaviruses (HPV-16,18) in cervical smears by in situ hybridization. Israel J Med Sci 1994;30:448–50. [PubMed] [Google Scholar]
- 59.Lörincz AT, Reid R, Jenson AB, et al. Human papillomavirus infection of the cervix: relative risk associations of 15 common anogenital types. Obstet Gynecol 1992;79:328–37. [DOI] [PubMed] [Google Scholar]
- 60.Kanetsky PA, Mandelblatt J, Richart R, et al. Risk factors for cervical cancer in a black, elderly population: preliminary findings. Ethn Dis 1992;2:337–42. [PubMed] [Google Scholar]
- 61.Kadish AS, Hagan RJ, Ritter DB, et al. Biologic characteristics of specific human papillomavirus types predicted from morphology of cervical lesions. Hum Pathol 1992;23:1262–9. [DOI] [PubMed] [Google Scholar]
- 62.Mandelblatt J, Richart R, Thomas L, et al. Is human papillomavirus associated with cervical neoplasia in elderly? Gynecol Oncol 1992;46:6–12. [DOI] [PubMed] [Google Scholar]
- 63.Saito J, Fukuda T, Nakatani H, et al. Detection of human papillomavirus DNA in the normal cervices of Japanese women by the dot-blot (Vira PapTM) method. Asia-Oceania J Obstet Gynaecol 1992;18:283–7. [PubMed] [Google Scholar]
- 64.Ohta M, Casanova H, Mizuno K, et al. Epidemiologic background and changes in patients infected with human papilloma virus. Nippon Sanka Fujinka Gakkai Zasshi 1991;43:479–84. [PubMed] [Google Scholar]
- 65.Wei Z, Yazhou S, Shunqian J, et al. The association between cervical carcinoma and human papilloma virus (HPV) in Xiangyuan county. Chin Med Sci J 1991;6:74–7. [PubMed] [Google Scholar]
- 66.Si JY, Lee K, Han R, et al. A research for the relationship between human papillomavirus and human uterine cervical carcinoma. I. The identification of viral genome and subgenomic consequences in biopsies of Chinese patients. J Cancer Res Clin Oncol 1991;117:454–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chang F, Syrjänen S, Shen Q, et al. Detection of human papillomavirus (HPV) in genital warts and carcinomas by DNA in situ hybridization in Chinese patients. Cytopathology 1990;1:97–103. [DOI] [PubMed] [Google Scholar]
- 68.Zhang GA. A study on the relationship between human papilloma virus (HPV) and cervical cancer. Chinese Journal of Epidemiology 1990;11:31–3. [PubMed] [Google Scholar]
- 69.Yokota H, Yoshikawa H, Shiromizu K, et al. Detection of human papillomavirus types 6/11, 16 and 18 in exfoliated cells from the uterine cervices of japanese women with and without lesions. Jpn J Cancer Res 1990;81:896–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Colgan TJ, Percy ME, Suri M, et al. Human papillomavirus infection of morphologically normal cervical epithelium adjacent to squamous dysplasia and invasive carcinoma. Hum Pathol 1989;20:316–19. [DOI] [PubMed] [Google Scholar]
- 71.Czeglédy J, Gergely L, Hernádi Z, et al. Detection of human papillomavirus deoxyribonucleic acid in the female genital tract. Med Microbiol Immunol (Berl) 1989;178:309–14. [DOI] [PubMed] [Google Scholar]
- 72.Reeves WC, Brinton LA, Garcia M, et al. Human papillomavirus infection and cervical cancer in Latin America. N Engl J Med. 1989;320:1437–41. [DOI] [PubMed] [Google Scholar]
- 73.Donnan SPB, Wong FWS, Ho SC, et al. Reproductive and sexual risk factors and human papilloma virus infection in cervical cancer among Hong Kong. Chinese International Journal of Epidemiology 1989;18:32–6. [DOI] [PubMed] [Google Scholar]
- 74.Zhang WH, Coppleson M, Rose BR, et al. Papillomavirus and cervical cancer; a clinical and laboratory study. J Med Virol 1988;26:163–74. [DOI] [PubMed] [Google Scholar]
- 75.Wilczynski SP, Walker J, Liao S-Y, et al. Adenocarcinoma of the cervix associated with human papillomavirus. Cancer 1988;62:1331–6. [DOI] [PubMed] [Google Scholar]
- 76.Fuchs PG, Girardi F. Pfister human papillomavirus DNA in normal, metaplastic, preneoplastic and epithelia of the cervix uteri. Int J Cancer 1988;41:41–5. [DOI] [PubMed] [Google Scholar]
- 77.Hsieh CY, Lee S-C, Huang S-C. Presence and expression of human papillomavirus types 16 and 18 DNA sequences in cervical carcinomas. Asia-Oceania J Obstet Gynaecol 1988;14:87–95. [DOI] [PubMed] [Google Scholar]
- 78.Choo K-B, Shen H-D, Leung W-Y, et al. A distinct difference in the prevalence of papillomavirus infection in cytologically normal and neoplastic cells of the uterine cervix. Chinese Med J (Taipei) 1988;42:1–6. [PubMed] [Google Scholar]
- 79.Kulski JK, Howard MJ, Pixley. ECDNA sequences of human papillomavirus types 11, 16 or 18 in invasive cervical carcinoma of Western Australian women. Immunol Cell Biol 1987;65:77–84. [DOI] [PubMed] [Google Scholar]
- 80.Zhang WH, Wu AR, Li JX, et al. Relation between human papillomavirus (HPV) and cancer of uterine cervix. Chinese Journal of Oncology 1987;9:433–5. [PubMed] [Google Scholar]
- 81.Lörincz AT, Temple GF, Kurman RJ, et al. Oncogenic association of specific human papillomavirus types with cervical neoplasia. J Natl Cancer Inst 1987;79:671–7. [PubMed] [Google Scholar]
- 82.Schneider A , de Villiers E-M, Schneider V. Multifocal squamous neoplasia of the female genital tract: significance of human papillomavirus infection of the vagina after hysterectomy. Obstet Gynecol 1987;70:294–8. [PubMed] [Google Scholar]
- 83.Meanwell CA, Cox MF, Blackledge G, et al. HPV 16 DNA in normal and malignant cervical epithelium: implications for the aetiology and behaviour of cervical neoplasia. Lancet 1987;1:703–7. [DOI] [PubMed] [Google Scholar]
- 84.McCance DJ, Campion MJ, Clarkson PK, et al. Prevalence of human papillomavirus type 16 DNA sequences in cervical intraepithelial neoplasia and invasive carcinoma of the cervix. Br J Obstet Gynaecol 1985;92:1101–5. [DOI] [PubMed] [Google Scholar]
- 85.Josefsson AM, Agnetha M, Magnusson PKE, et al. Viral load of human papilloma virus 16 as a determinant for development of cervical carcinoma in situ: a nested case-control study. Lancet 2000;355:2189–93. [DOI] [PubMed] [Google Scholar]
- 86.Ylitalo N, Josefsson A, Melbye M, et al. A prospective study showing long-term infection with human papillomavirus 16 before the development of cervical carcinoma in situ. Cancer Res 2000;60:6027–32. [PubMed] [Google Scholar]
- 87.Lacey JV, Frisch M, Brinton LA, et al. Association between smoking and adenocarcinomas and squamous cell carcinomas of the uterine cervix (United States). Cancer Causes Control 2001;12:153–61. [DOI] [PubMed] [Google Scholar]
- 88.van Beurden M, ten Kate FWJ, Smits HL, et al. Multifocal vulvar intraepithelial neoplasia grade III and multicentric lower genital tract neoplasia is associated with transcriptionally active human papillomavirus. Cancer 1995;75:2879–84. [DOI] [PubMed] [Google Scholar]
- 89.van Beurden M, ten Kate FWJ, Tjong-A-Hunt SP, et al. Human papillomavirus DNA in multicentric vulvar intraepithelial neoplasia. Int J Gynecol Pathol 1998;17:12–16. [DOI] [PubMed] [Google Scholar]
- 90.Pinto AP, Signorello LB, Crum CP, et al. Squamous cell carcinoma of the vulva in brazil: prognostic importance of host and viral variables. Gynecol Oncol 1999;14:61–7. [DOI] [PubMed] [Google Scholar]
- 91.Brandsman JL, Abramson AL. Association of papillomavirus with cancers of the head and neck. Arch Otolaryngol Head Neck Surg 1989;115:621–5. [DOI] [PubMed] [Google Scholar]
- 92.Snijders PJF, Cromme FV, van der Brule AJC, et al. Prevalence and expression of human papillomavirus in tonsillar carcinomas, indicating a possible viral etiology. Int J Cancer 1992;51:845–50. [DOI] [PubMed] [Google Scholar]
- 93.Cruz IBF, Snijders PJF, Steenbergen RDM, et al. Age-dependence of human papillomavirus DNA presence in oral squamous cell carcinomas. Eur J Cancer Oral Oncol 1996;32B:55–62. [DOI] [PubMed] [Google Scholar]
- 94.Frisch M, Biggar RJ. Aetiological parallel between tonsillar and anogenital squamous-cell carcinomas: Lancet 1999;354:1442–5. [DOI] [PubMed] [Google Scholar]
- 95.Harwood CA, Surentheran T, McGregor JM, et al. Human papillomavirus infection and non-melanoma skin cancer in immunosuppressed and immunocompetent individuals. J Med Virol 2000;61:289–97. [DOI] [PubMed] [Google Scholar]
- 96.Newton RA. review of the aetiology of squamous cell carcinoma of the conjunctiva. Br J Cancer 1996;74:1511–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Xi LF, Koutsky LA, Galloway DA, et al. Genomic variation of human papillomavirus type 16 and risk for high grade cervical intraepithelial neoplasia. J Natl Cancer Inst 1997;89:796–802. [DOI] [PubMed] [Google Scholar]
- 98.Villa LL, Sichero L, Rahal P, et al. Molecular variants of human papillomavirus types 16 and 18 preferentially associated with cervical neoplasia. J Gen Virol 2000;81:2959–68. [DOI] [PubMed] [Google Scholar]
- 99.Hildesheim A, Schiffman M, Bromley C, et al. Human papillomavirus type 16 variants and risk of cervical cancer. J Natl Cancer Inst 2001;93:315–18. [DOI] [PubMed] [Google Scholar]
- 100.Syrjänen K, Syrjänen S. HPV infections in other sites and lesions. In: Infections in human pathology. UK: Wiley 1999:445–56.
- 101.Lazcano-Ponce E, Herrero R, Muñoz N, et al. Epidemiology of HPV infection among Mexican women with normal cervical cytology. Int J Cancer 2001;91:1–9. [DOI] [PubMed] [Google Scholar]
- 102.Melkert PW, Hopman E, van den Brule AJ, et al. Prevalence of HPV in cytomorphologically normal cervical smears, as determined by the polymerase chain reaction, is age-dependent. Int J Cancer 1993;53:919–23. [DOI] [PubMed] [Google Scholar]
- 103.Bauer HM, Hildesheim A, Schiffman MH, et al. Determinants of genital human papillomavirus infection in low-risk women in Portland, Oregon. Sex Transm Dis 1993;20:274–8. [DOI] [PubMed] [Google Scholar]
- 104.Bosch FX, Muñoz N, de Sanjosé S, et al. Importance of human papillomavirus endemicity in the incidence of cervical cancer: an extension of the hypothesis on sexual behavior. Cancer Epidemiol Biomarkers Prev 1994;3:375–9. [PubMed] [Google Scholar]
- 105.Kjaer SK, Van der Brule AJC, Boch JE, et al. Determinants for genital human papillomavirus (HPV) infection in 1000 randomly chosen young Danish women with normal Pap smear: are there different risk profiles for oncogenic and nononcogenic HPV types? Cancer Epidemiol Biomarkers Prev 1997;6:799–805. [PubMed] [Google Scholar]
- 106.Jacobs MV, Walboomers JMM, Snijders PJF, et al. Distribution of 37 mucosotropic HPV types in women with cytologically normal cervical smears: the age-related patterns for high-risk and low-risk types. Int J Cancer 2000;87:221–7. [PubMed] [Google Scholar]
- 107.Schneider A, Hoyer H, Lotz B, et al. Screening for high-grade cervical intra-epithelial neoplasia and cancer by testing for high-risk HPV, routine cytology or colposcopy. Int J Cancer 2000;89:529–34. [PubMed] [Google Scholar]
- 108.Parkin DM, Whelan SL, Ferlay J, et al. Cancer incidence in five continents. Lyon: IARC Scientific Publications, Vol. VII, No 143, 1997.
- 109.Franco EL, Villa LL, Sobrinho JP, et al. Epidemiology of acquisition and clearance of cervical human papillomavirus infection in women from a high-risk area for cervical cancer. J Infect Dis 1999;180:1415–23. [DOI] [PubMed] [Google Scholar]
- 110.Ho GYF, Biermal R, Beardsley L, et al. Natural history of cervicovaginal papillomavirus infection in young women. N Engl J Med 1998;338:423–28. [DOI] [PubMed] [Google Scholar]
- 111.Koutsky LA, Holmes KK, Critchlow CW, et al. A cohort study of the risk of cervical intraepithelial neoplasia grade 2 or 3 in relation to papillomavirus infection. N Engl J Med 1992;327:1272–8. [DOI] [PubMed] [Google Scholar]
- 112.Ho GYF, Burk RD, Klein S, et al. Persistent genital human papillomavirus infection as a risk factor for persistent cervical dysplasia. J Natl Cancer Inst 1995;87:1365–71. [DOI] [PubMed] [Google Scholar]
- 113.Remmink AJ, Walboomers JM, Helmerhorst TJ, et al. The presence of persistent high-risk HPV genotypes in dysplastic cervical lesions is associated with progressive disease: natural history up to 36 months. Int J Cancer 1995;61:306–11. [DOI] [PubMed] [Google Scholar]
- 114.Nobbenhuis MAE, Walboomers JMM, Helmerhorst TJM, et al. Relation of human papillomavirus status to cervical lesions and consequences for cervical-cancer screening: a prospective study. Lancet 1999;354:20–5. [DOI] [PubMed] [Google Scholar]
- 115.Rozendaal L, Walboomers JM, van der Linden JC, et al. PCR-based high-risk HPV test in cervical cancer screening gives objective risk assessment of women with cytomorphologically normal cervical smears. Int J Cancer 1996;68:766–9. [DOI] [PubMed] [Google Scholar]
- 116.Rozendaal L, Westerga J, van der Linden JC, et al. PCR based high risk HPV testing is superior to neural network based screening for predicting incident CIN III in women with normal cytology and borderline changes. J Clin Pathol 2000;53:606–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Zielinski GD, Snijders PJF, Rozendaal L, et al. HPV presence precedes abnormal cytology in women developing cervical cancer and signals false negative smears. Br J Cancer 2001;85:398–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Nobbenhuis MAE, Helmerhorst THJM, van den Brule AJC, et al. Cytological regression and clearance of high-risk human papillomavirus in women with abnormal cervical smear. Lancet 2001;358:1782–3. [DOI] [PubMed] [Google Scholar]
- 119.Manos MM, Kinney WK, Hurley LB, et al. Identifying women with cervical neoplasia: using human papillomavirus DNA testing for equivocal Papanicolaou results. JAMA 1999;281:1605–10. [DOI] [PubMed] [Google Scholar]
- 120.Schlecht NF, Kulaga S, Robitaille J, et al. Persistent human papillomavirus infection as a predictor of cervical intraepithelial neoplasia. JAMA 2001;286:3106–14. [DOI] [PubMed] [Google Scholar]
- 121.Zielinski GD, Snijders PJF, Rozendaal L, et al. High-risk HPV testing in women with borderline and mild dyskaryosis: long-term follow-up data and clinical relevance. J Clin Pathol 2001;193:1–8. [DOI] [PubMed] [Google Scholar]
- 122.Nobbenhuis MA, Meijer CJ, van den Brule AJ, et al. Addition of high-risk HPV testing improves the current guidelines on follow-up after treatment for cervical intraepithelial neoplasia. Br J Cancer 2001;84:796–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Wallin K-L, Wiklund F, Angström T, et al. Type-specific persistence of human papillomavirus DNA before the development of invasive cervical cancer. N Engl J Med 1999;341:1633–8. [DOI] [PubMed] [Google Scholar]
- 124.Dillner J, Lehtinen M, Bjorge T, et al. Prospective seroepidemiologic study of human papillomavirus infection as a risk factor for invasive cervical cancer. J Natl Cancer Inst 1997;89:1293–9. [DOI] [PubMed] [Google Scholar]
- 125.Campion MJ, McCance DJ, Cuzick J, et al. Progressive potential of mild cervical atypia; prospective cytological, colposcopic, and virological study. Lancet 1986;2:237–40. [DOI] [PubMed] [Google Scholar]
- 126.Cuzick J, Terry G, Ho L, et al. Human papillomavirus type 16 DNA in cervical smears as predictor of high-grade cervical cancer. Lancet 1992;339:959–60. [DOI] [PubMed] [Google Scholar]
- 127.Cuzick J, Terry G, Ho L, et al. Type-specific human papillomavirus DNA in abnormal smears as a predictor of high-grade cervical intraepithelial neoplasia. Br J Cancer 1994;69:167–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Cuzick J, Szarewski A, Terry G, et al. Human papillomavirus testing in primary cervical screening. Lancet 1995;345:1533–6. [DOI] [PubMed] [Google Scholar]
- 129.Cuzick J, Sasieni P, Davies P, et al. A systematic review of the role of human papillomavirus (HPV) testing within a cervical screening programme: summary and conclusions. Br J Cancer 2000;83:561–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Ratnam S, Franco EL, Ferenczy A. Human papillomavirus testing for primary screening of cervical cancer precursors. Cancer Epidemiol Biomarkers Prev 2000;9:945–51. [PubMed] [Google Scholar]
- 131.Solomon D, Schiffman M, Tarone R. Comparison of three management strategies for patients with atypical squamous cells of undetermined significance: baseline results from a randomized trial. J Natl Cancer Inst 2001;93:293–9. [DOI] [PubMed] [Google Scholar]
- 132.Clavel C, Masure M, Bory JP, et al. Hybrid capture II-based human papillomavirus detection, a sensitive test to detect in routine high-grade cervical lesions: a preliminary study on 1518 women. Br J Cancer 1999;80:1306–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Schiffman MH, Herrero R, Hildesheim A, et al. HPV DNA testing in cervical cancer screening. JAMA 2000;283:87–93. [DOI] [PubMed] [Google Scholar]
- 134.Wright TC, Jr, Denny L, Kuhn L, et al. HPV DNA testing of self-collected vaginal samples compared with cytologic screening to detect cervical cancer. JAMA 2000;283:81–6. [DOI] [PubMed] [Google Scholar]
- 135.Hildesheim A, Gravitt P, Schiffman MH, et al. Determinants of genital human papillomavirus infection in low-risk women in Washington, DC. Sex Transm Dis 1993;20:279–84. [DOI] [PubMed] [Google Scholar]
- 136.Wheeler CM, Parmenter CA, Hunt WC, et al. Determinants of genital human papillomavirus infection among cytologically normal women attending the University of New Mexico student health center. Sex Transm Dis 1993;20:286–9. [DOI] [PubMed] [Google Scholar]
- 137.Franco EL, Villa LL, Ruiz A, et al. Transmission of cervical human papillomavirus infection by sexual activity: differences between low- and high-risk oncogenic types. J Infect Dis 1995;172:756–63. [DOI] [PubMed] [Google Scholar]
- 138.Muñoz N, Kato I, Bosch FX, et al. Risk factors for HPV DNA detection in middle-aged women. Sex Transm Dis 1996;23:504–10. [DOI] [PubMed] [Google Scholar]
- 139.Sillins I, Kallings I, Dillner J. Correlates of the spread of human papillomavirus infection. Cancer Epidemiol Biomarkers Prev 2000;9:953–9. [PubMed] [Google Scholar]
- 140.Rousseau MC, Franco EL, Villa LL, et al. A cumulative case-control study of risk factor profiles for oncogenic and non-oncogenic cervical human papillomavirus infections. Cancer Epidemiol Biomarkers Prev 2000;9:469–76. [PubMed] [Google Scholar]
- 141.Kjaer SK, Chackerian B, Van den Brule AJC, et al. High-risk human papillomavirus is sexually transmitted: evidence from a follow-up study of virgins starting sexual activity (intercourse). Cancer Epidemiol Biomarkers Prev 2001;10:101–6. [PubMed] [Google Scholar]
- 142.Barrasso R, de Brux J, Croissant O, et al. High prevalence of papillomavirus-associated penile intraepithelial neoplasia in sexual partners of women with cervical intraepithelial neoplasia. N Engl J Med 1987;317:916–23. [DOI] [PubMed] [Google Scholar]
- 143.Kjaer SK, de Villiers EM, Dahl C, et al. Case-control study of risk factors for cervical neoplasia in Denmark. I: Role of the “male factor” in women with one lifetime sexual partner. Int J Cancer 1991;48:39–44. [DOI] [PubMed] [Google Scholar]
- 144.Bergman A, Nalick R. Prevalence of human papillomavirus infection in men: comparison of the partners of infected and uninfected women. J Reprod Med 1992;37:710–12. [PubMed] [Google Scholar]
- 145.Bosch FX, Castellsagué X, Muñoz N, et al. Male sexual behavior and human papillomavirus DNA: key risk factors for cervical cancer in Spain. J Natl Cancer Inst 1996;88:1060–7. [DOI] [PubMed] [Google Scholar]
- 146.Castellsagué X, Ghaffari A, Daniel RW, et al. Prevalence of penile human papillomavirus DNA in husbands of women with and without cervical neoplasia: a study in Spain and Colombia. J Infect Dis 1997;176:353–61. [DOI] [PubMed] [Google Scholar]
- 147.de Sanjosé S, Palacio V, Tafur L, et al. Prostitution, HIV, and cervical neoplasia: a survey in Spain and Colombia. Cancer Epidemiol Biomarkers Prev 1993;2:531–5. [PubMed] [Google Scholar]
- 148.Thomas DB, Ray RM, Kuypers J, et al. Human papillomaviruses and cervical cancer in Bangkok. III. The role of husbands and commercial sex workers. Am J Epidemiol 2001;153:740–8. [DOI] [PubMed] [Google Scholar]
- 149.Juarez-Figueroa LA, Wheeler CM, Uribe-Salas FJ, et al. Human papillomavirus: a highly prevalent sexually transmitted disease agent among female sex workers from Mexico City. Sex Transm Dis 2001;28:125–30. [DOI] [PubMed] [Google Scholar]
- 150.Castellsagué X, Bosch FX, Muñoz N, et al. Male circumcision, penile human papillomavirus (HPV) infection and cervical cancer. N Engl J Med [In press.] [DOI] [PubMed]
- 151.Rigoni-Stern. Fatti statistici relativi alle malattie cancerose. Giorn Prog Patol Terap 1842;2:507–17. [Google Scholar]
- 152.Beral V. Cancer of the cervix: a sexually transmitted infection? Lancet 1974;i:1037–40. [DOI] [PubMed]
- 153.Skegg DC, Corwin PA, Paul C, et al. Importance of the male factor in cancer of the cervix. Lancet 1982;2:581–3. [DOI] [PubMed] [Google Scholar]
- 154.Schiffman MH. New epidemiology of human papillomavirus infection and cervical neoplasia. J Natl Cancer Inst 1995;87:20. [DOI] [PubMed] [Google Scholar]
- 155.Ylitalo N, Sorensen P, Josefsson AM, et al. Consistent high viral load of human papillomavirus 16 and risk of cervical carcinoma in situ: a nested case-control study. Lancet 2000;355:2194–8. [DOI] [PubMed] [Google Scholar]
- 156.van Duin M, Snijders PJF, Schrijnemakers HFJ, et al. Human papillomavirus 16 load in normal and abnormal cervical scrapes: an indicator of CIN II/III and viral clearance. Int J Cancer [In press.] [DOI] [PubMed]
- 157.Cubie H, Seagar A, McGoogan E, et al. Rapid real time PCR to distinguish between high risk human papillomavirus types 16 and 18. Mol Pathol 2001;54:24–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Stern P, Duggan-Keen M. MHC expression in the natural history of cervical cancer In: Stern PL, Stanley MA, eds. Human papillomaviruses and cervical cancer. Biology and immunology. New York: Oxford University Press, 1994:162–76.
- 159.Tommasino M. Papillomaviruses in human cancer: the role of E6 and E7 oncoproteins. Austin, Texas: Landes Bioscience, 1997.
- 160.Lazo PA. The molecular genetics of cervical carcinoma. Br J Cancer 1999;80:2008–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.McGlennen RC. Human papillomavirus oncogenesis. Clin Lab Med 2000;20:383–404. [PubMed] [Google Scholar]
- 162.Woodworth CD, Doniger J, DiPaolo JA. Immortalization of human foreskin keratinocytes by various human papillomavirus DNAs corresponds to their association with cervical carcinoma. J Virol 1989;63:159–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Meyers C, Laimins LA. In vitro systems for the study and propagation of human papillomaviruses. Curr Top Microbiol Immunol 1994;186:199–215. [DOI] [PubMed] [Google Scholar]
- 164.Steenbergen RDM, Walboomers JMM, Meijer CJLM, et al. Transition of human papillomavirus type 16 and 18 transfected human foreskin keratinocytes towards immortality: activation of telomerase and allele losses at 3p, 10p, 11q and/or 18q. Oncogene 1996;13:1249–57. [PubMed] [Google Scholar]
- 165.Stoler MH, Rhodes CR, Whitbeck A, et al. Human papillomavirus type 16 and 18 gene expression in cervical neoplasias. Hum Pathol 1992;23:117–28 . [DOI] [PubMed] [Google Scholar]
- 166.Lancaster WD, Castellano C, Santos C, et al. Human papillomavirus deoxyribonucleic acid in cervical carcinoma from primary and metastatic sites. Am J Obstet Gynecol 1986;154:115–19. [DOI] [PubMed] [Google Scholar]
- 167.Schwarz E, Freese UK, Gissmann L, et al. Structure and transcription of human papillomavirus sequences in cervical carcinoma cells. Nature 1985;314:111–14. [DOI] [PubMed] [Google Scholar]
- 168.Durst M, Glitz D, Schneider A, et al. Human papillomavirus type 16 (HPV 16) gene expression and DNA replication in cervical neoplasia: analysis by in situ hybridization. Virology 1992;189:132–40. [DOI] [PubMed] [Google Scholar]
- 169.Durst M, Kleinheinz A, Hotz M, et al. The physical state of human papillomavirus type 16 DNA in benign and malignant genital tumours. J Gen Virol 1985;66:1515–22. [DOI] [PubMed] [Google Scholar]
- 170.Cullen AP, Reid R, Campion M, et al. Analysis of the physical state of different human papillomavirus DNAs in intraepithelial and invasive cervical neoplasm. J Virol 1991;65:606–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Stanbridge EJ. Suppression of malignancy in human cells. Nature 1976;260:17–20. [DOI] [PubMed] [Google Scholar]
- 172.Saxon PJ, Srivatsan ES, Stanbridge EJ. Introduction of human chromosome 11 via microcell transfer controls tumorigenic expression of HeLa cells. EMBO J 1986;5:3461–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Koi M, Morita H, Yamada H, et al. Normal human chromosome 11 suppresses tumorigenicity of human cervical tumor cell line SiHa. Mol Carcinog 1989;2:12–21. [DOI] [PubMed] [Google Scholar]
- 174.Backsch C, Wagenbach N, Nonn M, et al. Microcell-mediated transfer of chromosome 4 into HeLa cells suppresses telomerase activity. Genes Chromosomes Cancer 2001;31:196–8. [DOI] [PubMed] [Google Scholar]
- 175.Steenbergen RDM, Kramer D, Meijer CJLM, et al. Telomerase suppression by chromosome 6 in a human papillomavirus type 16-immortalized keratinocyte cell line and in a cervical cancer cell line. J Natl Cancer Inst 2001;93:865–72. [DOI] [PubMed] [Google Scholar]
- 176.Dyson N, Howley PM, Munger K, et al. The human papilloma virus-16 E7 oncoprotein is able to bind to the retinoblastoma gene product. Science 1989;243:934–6. [DOI] [PubMed] [Google Scholar]
- 177.Lörincz AT. Human papillomaviruses. In: Lennette EH, Smith TF, eds. Laboratory diagnosis of viral infections. New York: Marcel Dekker, 1999:635–63.
- 178.Werness BA, Levine AJ, Howley PM. Association of human papillomavirus types 16 and 18 E6 proteins with p53. Science 1990;248:76–9. [DOI] [PubMed] [Google Scholar]
- 179.Cheng S, Schmidt-Grimminger D-C, Murant T, et al. Differentiation-dependent up-regulation of the human papillomavirus E7 gene reactivates cellular DNA replication in suprabasal differentiated keratinocytes. Genes Dev 1995;9:2335–49. [DOI] [PubMed] [Google Scholar]
- 180.Jian Y, Schmidt-Grimminger D-C, Chien W-M, et al. Post-transcriptional induction of p21cip1 protein by human papillomavirus E7 inhibits unscheduled DNA synthesis reactivated in differentiated keratinocytes. Oncogene 1998;17:2027–38. [DOI] [PubMed] [Google Scholar]
- 181.Schmidt-Grimminger D-C, Wu X, Jian Y, et al. Post-transcriptional induction of p21cip1 protein in condylomata and dysplasias is inversely related to human papillomavirus activities. Am J Pathol 1998;152:1015–24. [PMC free article] [PubMed] [Google Scholar]
- 182.Steenbergen RDM, Parker JN, Isern S, et al. Viral E6-E7 transcription in the basal layer of organotypic cultures without apparent p21cip1 protein precedes immortalization of HPV 16 and HPV 18 transfected human keratinocytes. J Virol 1998;72:749–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Stoler MH. Human papillomaviruses and cervical neoplasia: a model for carcinogenesis. Int J Gynecol Pathol 2000;19:16–28. [DOI] [PubMed] [Google Scholar]
- 184.Hildesheim A, Schiffman MH, Tsukui T, et al. Immune activation in cervical neoplasia: cross-sectional association between plasma soluble interleukin 2 receptor levels and disease. Cancer Epidemiol Biomarkers Prev 1997;6:807–13. [PubMed] [Google Scholar]
- 185.Tsukui T, Hildesheim A, Schiffman MH et al. Interleukin 2 production in vitro by peripheral lymphocytes in response to human papillomavirus-derived peptides: correlation with cervical pathology. Cancer Res 1996;56:3697–74. [PubMed] [Google Scholar]
- 186.Chow LT, Broker TR. Papillomavirus DNA replication. Intervirology 1994;37:150–8. [DOI] [PubMed] [Google Scholar]
- 187.Dollard SC, Wilson JL, Demeter LM, et al. Production of human papillomavirus and modulation of the infectious program in epithelial raft cultures. Genes Dev 1992;6:1131–42. [DOI] [PubMed] [Google Scholar]
- 188.Flores ER, Lambert PF. Evidence for a switch in the mode of human papillomavirus type 16 DNA replication during the viral life cycle. J Virol 1997;71:7167–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Munger K, Scheffner M, Huibregtse JM, et al. Interactions of HPV E6 and E7 oncoproteins with tumour suppressor gene products. In: Levine AJ, ed. Tumour suppressor genes, the cell cycle and cancer. New York: Cold Spring Harbor Laboratory Press, 1992:197–217. [PubMed]
- 190.Turek LP, Smith EM. The genetic program of genital human papillomaviruses in infection and cancer. Obstet Gynecol Clin North Am 1996;23:735–58. [DOI] [PubMed] [Google Scholar]
- 191.zur Hausen H. Roots and perspectives of contemporary papillomavirus research. J Cancer Res Clin Oncol 1996;122:3–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Tommasino M, Adamczewski JP, Carlotti F, et al. HPV16 E7 protein associates with the protein kinase p33CDK2 and cyclin A. Oncogene 1993;8:195–202. [PubMed] [Google Scholar]
- 193.Demeter LM, Stoler MH, Broker TR, et al. Induction of proliferating cell nuclear antigen in differentiated keratinocytes of human papillomavirus-infected lesions. Hum Pathol 1994;25:343–8. [DOI] [PubMed] [Google Scholar]
- 194.Stoler MH, Wolinsky SM, Whitbeck A, et al. Differentiation-linked human papillomavirus types 6 and 11 transcription in genital condylomata revealed by in situ hybridization with message-specific RNA probes. Virology 1989;172:331–40. [DOI] [PubMed] [Google Scholar]
- 195.Arends MJ, Wyllie AH, Bird CC. Human papillomavirus type 18 is associated with less apoptosis in fibroblast tumours than human papillomavirus type 16. Br J Cancer 1995;72:646–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Jones DL, Munger K. Analysis of the p53-mediated G1 growth arrest pathway in cells expressing the human papillomavirus type 16 E7 oncoprotein. J Virol 1997;71:2905–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.McCance DJ, Kopan R, Fuchs E, et al. Human papillomavirus type 16 alters human epithelial cell differentiation in vitro. Proc Natl Acad Sci U S A 1988;85:7169–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.McDougall JK, Klingelhutz AJ. Telomerase and the HPV oncogenes: more than a terminal relationship. Papillomavirus Report 1999;10:81–4. [Google Scholar]
- 199.Jeon S, Allen-Hoffmann BL, Lambert PF. Integration of human papillomavirus type 16 into the human genome correlates with a selective growth advantage of cells. J Virol 1995;69:2989–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.zur Hausen H. Papillomavirus infections—a major cause of human cancers. Biochim Biophys Acta 1996;1288:F55–78. [DOI] [PubMed] [Google Scholar]
- 201.Bauknecht T, See RH, Shi Y. A novel C/EBP beta-YY1 complex controls the cell-type-specific activity of the human papillomavirus type 18 upstream regulatory region. J Virol 1996;70:7695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Dong X-P, Stubenrauch F, Beyer-Finkler E, et al. Prevalence of deletions of YY1-binding sites in episomal HPV 16 DNA from cervical cancers. Int J Cancer 1994;58:803–8. [DOI] [PubMed] [Google Scholar]
- 203.May M, Dong X-P, Beyer-Finkler E, Stubenrauch F, et al. The E6/E7 promoter of extrachromosomal HPV16 DNA in cervical cancers escapes from cellular repression by mutation of target sequences for YY1. EMBO J 1994;13:1460–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Kessis TD, Slebos RJ, Nelson WG, et al. Human papillomavirus 16 E6 expression disrupts the p53-mediated cellular response to DNA damage. Proc Natl Acad Sci U S A 1993;90:3988–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Scheffner M, Munger K, Byrne JC, et al. The state of the p53 and retinoblastoma genes in human cervical carcinoma cell lines. Proc Natl Acad Sci U S A 1991;88:5523–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Liotta LA, Kohn EC The microenvironment of the tumour-host interface. Nature 2001;411:375–9. [DOI] [PubMed] [Google Scholar]
- 207.Saveria Campo M. Towards vaccines against papillomavirus. In: Stern PL, Stanley MA, eds. Human papillomaviruses and cervical cancer. Biology and immunology. New York: Oxford University Press, 1994:177–82.
- 208.Tindle RW. Vaccines for human papillomavirus infection and anogenital disease. Texas: RG Landes Company, 1999.
- 209.de Villiers EM. Taxonomic classification of papillomavirus. Papillomavirus Report 2001;12:57–63. [Google Scholar]
- 210.Riou G, Favre M, Jeannel D, et al. Association between poor prognosis in early-stage invasive cervical carcinomas and non-detection of HPV DNA. Lancet 1990;335:1171–4. [DOI] [PubMed] [Google Scholar]
- 211.Viladiu P, Bosch FX, Castellsague X, et al. Human papillomavirus DNA and antibodies to human papillomaviruses 16 E2, L2, and E7 peptides as predictors of survival in patients with squamous cell cervical cancer. J Clin Oncol 1997;15:610–19. [DOI] [PubMed] [Google Scholar]
- 212.Tabrizi SN, Fairley ChK, Chen Sh, et al. Epidemiological characteristics of women with high grade CIN who do and do not have human papillomavirus. Br J Obstet Gynaecol 1999;106:252–7. [DOI] [PubMed] [Google Scholar]
- 213.Burger MPM, Hollema H, Pieters WJLM, et al. Epidemiological evidence of cervical intraepithelial neoplasia without the presence of human papillomavirus. Br J Cancer 1996;73:831–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Muñoz N, Bosch FX, Kaldor JM. Does human papillomavirus cause cervical cancer? The state of the epidemiological evidence. Br J Cancer 1988;57:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Schiffman MH, Schatzkin A. Test reliability is critically important to molecular epidemiology: an example from studies of human papillomavirus infection and cervical neoplasia. Cancer Res 1994;54(suppl 7):1944s–7s. [PubMed] [Google Scholar]
- 216.Walboomers JM, Jacobs MV, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol 1999;189:12–9. [DOI] [PubMed] [Google Scholar]
- 217.Deacon JM, Evans CD, Yule R, et al. Sexual behaviour and smoking as determinants of cervical HPV infection and of CIN 3 among those infected: a case-control study nested within the Manchester cohort. Br J Cancer 2000;88:1565–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.de Sanjose S, Muñoz N, Bosch FX, et al. Sexually transmitted agents and cervical neoplasia in Colombia and Spain. Int J Cancer 1994;56:358–63. [DOI] [PubMed] [Google Scholar]
- 219.Bayo S, Bosch FX, de Sanjosé S, et al. Risk factors of invasive cervical cancer in Mali. Int J Cancer [In press.] [DOI] [PubMed]
- 220.Moreno V, Bosch FX, Muñoz N, et al. Oral contraceptives and cervical cancer: pooled analysis of the IARC multicentric case-control study. Lancet [In press.]
- 221.Kjaer SK, van den Brule AJC, Svare EI, et al. Different risk factor patterns for high-grade and low-grade intraepithelial lesions on the cervix among HPV-positive and HPV-negative young women. Int J Cancer 1998;76:613–9. [DOI] [PubMed] [Google Scholar]
- 222.Lacey JV, Brinton LA, Abbas FM, et al. Oral contraceptives as risk factors for cervical adenocarcinomas and squamous cell carcinomas. Cancer Epidemiol Biomarkers Prev 1999;8:1079–85. [PubMed] [Google Scholar]
- 223.IARC. Hormonal contraception and post-menopausal hormonal therapy. IARC monographs on the evaluation of carcinogenic risks to humans, Vol. 72. Lyon: IARC, 1999.
- 224.Muñoz N, Franceschi S, Bosch FX, et al. The influence of reproductive and menstrual factors on cervical cancer in HPV-positive women. Lancet [In press.]
- 225.Hildesheim A, Herrero R, Castle PE, et al. HPV co-factors related to the development of cervical cancer: results from a population-based study in Costa Rica. Br J Cancer 2001;84:1219–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Kjaer SK, de Villiers EM, Haugaard BJ, et al. Human papillomavirus, herpes simplex virus and cervical cancer incidence in Greenland and Denmark. A population-based cross-sectional study. Int J Cancer 1988;41:518–24. [DOI] [PubMed] [Google Scholar]
- 227.Ferrera A, Velema JP, Figueroa M, et al. Co-factors related to the causal relationship between human papillomavirus and invasive cervical cancer in Honduras. Int J Epidemiol 2000;29:817–25. [DOI] [PubMed] [Google Scholar]
- 228.Winkelstein W, Jr. Smoking and cancer of the uterine cervix: hypothesis. Am J Epidemiol 1977;106:257–9. [DOI] [PubMed] [Google Scholar]
- 229.IARC. Tobacco smoking. Lyon: IARC monographs on the evaluation of carcinogenic risks to humans, Vol. 38. Lyon: IARC, 1986.
- 230.Szarewski A, Cuzick J. Smoking and cervical neoplasia: a review of the evidence. J Epidemiology and Biostatistics 1998;3:229–56. [Google Scholar]
- 231.Surgeon General's Advisory Committee on Women and Smoking. Public Health Service, 2001. (Available online:http://www.cdc.gov/tobacco.)
- 232.Kjaer SK. Risk factors for cervical neoplasia in Denmark. APMIS 1998;80:1–41. [PubMed] [Google Scholar]
- 233.Beasley RP, Trepo C, Stevens CE, et al. The E antigen and vertical transmission of hepatitis B surface antigen. Am J Epidemiol 1977;105:94–8. [DOI] [PubMed] [Google Scholar]
- 234.Coursaget P, Yvonnet B, Chotard J, et al. Age and sex-related study of hepatitis B virus chronic carrier state in infants from an endemic area (Senegal). J Med Virol 1987;22:1–5. [DOI] [PubMed] [Google Scholar]
- 235.Evans AS, Niederman JC. Epstein-Barr virus. In: Evans AS ed. Viral infections of humans, 3rd ed. New York: Plenum, 1989:265–92.
- 236.Smith JS, Muñoz N, Herrero R, et al. Evidence for Chlamydia trachomatis as an HPV cofactor in the etiology of invasive cervical cancer in Brazil and the Philippines. J Infect Dis 2002;185:324–31. [DOI] [PubMed] [Google Scholar]
- 237.Castle PE, Hillier SL, Rabe LK, et al. An association of cervical inflammation with high-grade cervical neoplasia in women infected with oncogenic human papillomavirus (HPV). Cancer Epidemiol Biomarkers Prev 2001;10:1021–7. [PubMed] [Google Scholar]
- 238.de Sanjose S, Bosch FX, Muñoz N, et al. Social differences in sexual behaviour and cervical cancer. In: Kogevinas M, Pearce N, Susser M, et al, eds. Social inequalities and cancer. Lyon: IARC Scientific Publications, 1997. (No. 138):309–17. [PubMed]
- 239.Potischman L, Brinton LA. Nutrition and cervical neoplasia. Cancer Causes Control 1996;7:113–26. [DOI] [PubMed] [Google Scholar]
- 240.Storey A, Thomas M, Kalita A, et al. Role of p53 polymorphism in the development of human papillomavirus-associated cancer. Nature 1998;393:229–34. [DOI] [PubMed] [Google Scholar]
- 241.Makni H, Franco E, Kaiano J, et al. p53 polymorphism in codon 72 and risk of HPV-induced cervical cancer: effect of interlaboratory variation. Int J Cancer 2000;87:528–33. [PubMed] [Google Scholar]
- 242.Madeleine MM, Shera K, Schwartz SM, et al. The p53 Arg72Pro polymorphism, human papillomavirus, and invasive squamous cell cervical cancer. Cancer Epidemiol Biomarkers Prev 2000;9:225–7. [PubMed] [Google Scholar]
- 243.Rezza G, Giuliani M, Garbuglia AR, et al. Lack of association between p53 codon-72 polymorphism and squamous intraepithelial lesions in women with, or at risk for, human immunodeficiency virus and/or human papillomavirus infections. Cancer Epidemiol Biomarkers Prev 2001;10:565–6. [PubMed] [Google Scholar]
- 244.Zehbe I, Voglino G, Wilander E, et al. p53 codon 72 polymorphisms and various human papillomavirus 16 E6 genotypes are risk factors for cervical cancer development. Cancer Res 2001;61:608–11. [PubMed] [Google Scholar]
- 245.Koskela P, Antilla T, Biorge T, et al. Chlamydia trachomatis infection as a risk factor for invasive cervical cancer. Int J Cancer 2000;85:35–9. [DOI] [PubMed] [Google Scholar]
- 246.van den Brule AJC, Kjaer SK, Munk C, et al. Development of HPV induced cervical intraepithelial neoplasias: infection with Chlamdya trachomatis as a possible cofactor. In: Castellsagué X, Bosch FX, de Sanjosé S, et al, eds. 18th International Papillomavirus Conference—program and abstracts book. Barcelona: Thau SL, 2000:130 (available on line: http:/www.hpv2000.com).
- 247.Villa LL, Franco EL. Epidemiologic correlates of cervical neoplasia and risk of human papillomavirus infection in asymptomatic women in Brazil. J Natl Cancer Inst 1989;81:332–40. [DOI] [PubMed] [Google Scholar]
- 248.Guerrero E, Daniel RW, Bosch FX, et al. Comparison of ViraPap, Southern hybridization, and polymerase chain reaction methods for human papillomavirus identification in an epidemiological investigation of cervical cancer. J Clin Microbiol 1992;33:2229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.zur Hausen H. Cervical carcinoma and human papillomavirus: on the road to preventing a major human cancer. J Natl Cancer Inst 2001;93:252–3. [DOI] [PubMed] [Google Scholar]
- 250.Bosch FX, Muñoz N, de Sanjosé S, et al. Re: cervical carcinoma and human papillomavirus: on the road to preventing a major human cancer. J Natl Cancer Inst 2001;93:1349–50. [DOI] [PubMed] [Google Scholar]
- 251.IARC. Human papillomavirus and cervical cancer. Muñoz N, Bosch FX, Jensen OM, eds. Lyon: IARC Scientific Publications, Vol. 94, 1989. [PubMed]
- 252.IARC. The epidemiology of cervical cancer and human papillomavirus. Muñoz N, Bosch FX, Shah KV, et al, eds. Lyon: IARC Scientific Publications, Vol. 119, 1992.
- 253.Meijer CJLM, Brule AJC van den, Snijders PJF, et al. Detection of human papilloma virus in cervical scrapes by the polymerase chain reaction in relation to cytology: possible implications for cervical cancer screening. In: Muñoz N, Bosch FX, Shah KV, Meheus A, eds. The epidemiology of cervical cancer and human papillomavirus. Lyon: IARC, 1992:271–81. [PubMed]
- 254.Cuzick J, Beverley E, Ho L, et al. HPV testing in primary screening of older women. Br J Cancer 1999;81:554–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Coutlée F, Gravitt P, Richardson H, et al. Nonisotopic detection and typing of human papillomavirus DNA in genital samples by the line blot assay. J Clin Microbiol 1999;37:1852–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Sellors JW, Mahony JB, Kaczorowski J, et al. Prevalence and predictors of human papillomavirus infection in women in Ontario, Canada. Can Med Assoc J 2000;163:503–8. [PMC free article] [PubMed] [Google Scholar]
- 257.Meijer CJLM, Walboomers JMM. Cervical cytology after 2000: where to go? J Clin Pathol 2000;53:41–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.The Atypical Squamous Cell of Undetermined Significance/Low-grade Squamous Intraepithelial Lesions Triage Study (ALTS) Group. Human papillomavirus testing for triage of women with cytologic evidence of low-grade squamous intraepithelial lesions: baseline data from a randomized trial. J Natl Cancer Inst 2000;92:397–402. [DOI] [PubMed] [Google Scholar]
- 259.Follen M, Richards-Kortum R. Emerging technologies and cervical cancer. J Natl Cancer Inst 2000;92:363–65. [DOI] [PubMed] [Google Scholar]
- 260.Sasieni PD. Human papillomavirus screening and cervical cancer prevention. J Am Med Wom Assoc 2000;55:216–19. [PubMed] [Google Scholar]
- 261.Stevenson , Hudson LC, Burns JE, et al. Inverse relationship between the expression of the human papillomavirus type 16 transcription factor E2 and virus DNA copy number during the progression of cervical intraepithelial neoplasia. J Gen Virol 2000;81:1825–32. [DOI] [PubMed] [Google Scholar]
- 262.Carter JJ, Koutsky LA, Hughes JP, et al. Comparison of human papillomavirus types 16, 18 and 6 capsid antibody responses following incident infection. J Infect Dis 2000;181:1911–19. [DOI] [PubMed] [Google Scholar]
- 263.Franco EL, Duarte-Franco E, Ferenczy A. Cervical cancer: epidemiology, prevention and the role of human papillomavirus infection. Can Med Assoc J 2001;164:1017–25. [PMC free article] [PubMed] [Google Scholar]
- 264.Lehtinen M, Luukkaala T, Wallin K-L, et al. Human papillomavirus infection, risk for subsequent development of cervical neoplasia and associated population attributable fraction. J Clin Virol 2001;22:117–24. [DOI] [PubMed] [Google Scholar]
- 265.Anttila T, Saiku P, Koskela P, et al. Serotypes of Chlamydia trachomatis and risk for development of cervical squamous cell carcinoma. JAMA 2001;285:47–51. [DOI] [PubMed] [Google Scholar]
- 266.Andersson S, Rylander E, Larsson B, et al. The role of human papillomavirus in cervical adenocarcinoma carcinogenesis. Eur J Cancer 2001;37:246–50. [DOI] [PubMed] [Google Scholar]
- 267.Clavel C, Masure M, Bory J-P, et al. Human papillomavirus testing in primary screening for the detection of high-grade cervical lesions: a study of 7932 women. Br J Cancer 2001;84:1616–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Goldie SJ, Kuhn L, Denny L, et al. Policy analysis of cervical cancer screening strategies in low-resource settings. Clinical benefits and cost-effectiveness. JAMA 2001;285:3107–15. [DOI] [PubMed] [Google Scholar]
- 269.Schwartz SM, Daling JR, Shera KA, et al. Human papillomavirus and prognosis of invasive cervical cancer: a population-based study. J Clin Oncol 2001;19:1906–15. [DOI] [PubMed] [Google Scholar]
- 270.Liaw K-L, Hildesheim A, Burk RD, et al. A prospective study of human papillomavirus (HPV) type 16 DNA detection by polymerase chain reaction and its association with acquisition and persistence of other HPV types. J Infect Dis 2001;183:8–15. [DOI] [PubMed] [Google Scholar]
- 271.Gravitt PE, Lacey JV, jr, Brinton LA, et al. Evaluation of self-collected cervicovaginal cell samples for human papillomavirus testing by polymerase chain reaction. Cancer Epidemiol Biomarkers Prev 2001;10:95–100. [PubMed] [Google Scholar]
- 272.Harro CD, Pang Y-YS, Roden RBS, et al. Safety and immunogenicity trial in adult volunteers of a human papillomavirus 16 L1 virus-like particle vaccine. J Natl Cancer Inst 2001;93:284–92. [DOI] [PubMed] [Google Scholar]
- 273.Peyton CL, Gravitt PE, Hunt WC, et al. Determinants of genital human papillomavirus detection in a US population. J Infect Dis 2001;183:1554–64. [DOI] [PubMed] [Google Scholar]
- 274.Multiple authors. From epidemiology to policy: a symposium on the translation of epidemiologic evidence into public health policy. Am J Epidemiol (Special Issue) 2001;154. [PubMed]
- 275.Lanes S. Causal inference is not a matter of science. Am J Epidemiol 1985;122:550. [Google Scholar]
- 276.Rothman KJ, Poole C. Science and policy making. Am J Public Health 1985;75:340–1. [DOI] [PMC free article] [PubMed] [Google Scholar]