Abstract
A case of primary amyloid tumour of the breast is reported with a brief review of the literature. The tumour was mammographically suspicious of carcinoma. Fine needle aspiration cytology yielded clumps of amorphous material surrounded by giant cells and lymphocytes. Subsequent histology showed nodular amyloid associated with osseous metaplasia and giant cell reaction. There are 13 cases of amyloid tumour of the breast reported in the literature and in four of these fine needle aspiration had been undertaken.
Keywords: breast, tumour, fine needle aspiration cytology, osseous metaplasia, amyloid
A myloidosis in the breast was first reported by Fernandez and Hernandez in 1973.1 Subsequently, several cases have been documented in the literature, including women with bilateral breast involvement.2–7 Most of the reported cases were elderly women who had mammographically suspicious lesions. By definition, amyloidosis is extracellular deposition of amorphous congophilic protein within tissues.8 To date, 15 different protein structures of amyloid have been identified, with AL and AA being the most common.9 Skin, tongue, the gastrointestinal tract, and the respiratory tract are other sites where primary amyloidosis is commonly reported. As in our case, most of the cytology case reports describe the appreciation of amyloid material in fine needle aspiration preparations only in retrospect.4,6
“By definition, amyloidosis is extracellular deposition of amorphous congophilic protein within tissues”
CASE REPORT
A 86 year old white woman presented to the regional breast screening service with a palpable left breast lump. She was known to have hyperthyroidism and diet controlled diabetes and was on regular treatment. She had a mild degree of osteopenia and had suffered repeated falls in the past. She had a permanent cardiac pacemaker since 1994 for blackouts. In March 2000 she had complete left bundle branch block and since then she was treated with digoxin for atrial fibrillation. Her breast lump was suspicious of malignancy, both clinically and mammographically, with malignant looking microcalcification. Fine needle aspiration cytology was performed, which was negative for malignancy, and reported to show a non-specific inflammatory reaction only. In view of the clinical and mammographic suspicion, excision biopsy of this lesion was performed.
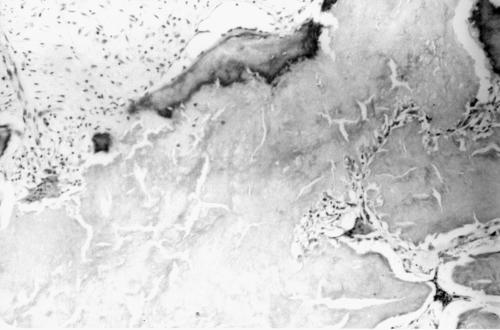
On gross examination, the breast tissue weighed 7.5 gm. Serial slicing of the excised mass showed a 1.6 cm size firm nodule close to the excision margins. All the tissue had been processed. Subsequent histological examination showed a mass composed of hyaline eosinophilic material surrounded by giant cells. There were foci of osseous metaplasia (fig 1). At the periphery, numerous plasma cells containing Russel bodies and lymphocytes were present. The congo red stain was positive in this hyaline material and showed apple green birefringence on polarising microscopy. Apart from this localised mass, amyloid was seen around occasional breast ducts and blood vessels. However, there was no amyloid within the walls of the blood vessels. There was no evidence of malignancy in the specimen submitted.
Figure 1.
Histopathology showing amyloid with osseous metaplasia. Haematoxylin and eosin stained; original magnification, ×100.
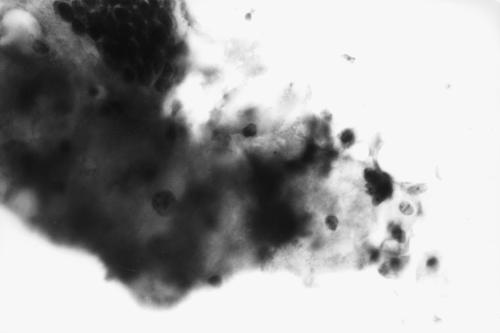
To evaluate the nature of this amyloid further, the sections were pretreated with potassium permanganate and then a congo red stain was carried out.10 The material resisted potassium permanganate treatment and retained its orange brown colour, thus confirming the AL type of amyloid. Considering the nature of amyloid the patient was investigated further. Her chest, spine, and skull radiographs were normal. The serum electrophoresis was also unremarkable. Urinary Bence-Jones proteins were negative. The haematology profile was normal. The cytology preparations were reviewed and showed amorphous homogenous material surrounded by giant cells and lymphocytes (fig 2).
Figure 2.
Cytology showing a fragment of hyaline dense amyloid material and giant cells. PAP stain; original magnification, ×400.
DISCUSSION
Amyloidosis of the breast can occur as organ specific nodular amyloidosis or as part of systemic amyloidosis. Organ specific nodular amyloidosis has been reported in skin, trachea, bronchi, and the urogenital tract, with breast being the lowest in frequency. To our knowledge, 13 cases of localised breast amyloidosis have been reported (table 1).1–7,11–15 Of these, our case is only the third to show foci of osteoid metaplasia, the previous ones having been documented by Lynch and Moriarty11 and by Yokoo and Nakazato.12 Two patients had bilateral amyloid deposits.5,11 In one patient, breast amyloidosis was associated with mucosa associated lymphoid tissue lymphoma.14 Localised amyloid deposits have been reported in a range of endocrine neoplasms including medullary carcinoma of the thyroid, bronchial carcinoid, phaeochromocytoma, and insulinoma. None of these was present in our case. Similarly, there was no evidence of chronic illness, such as rheumatoid arthritis.
Table 1.
Amyloid tumour of the breast; case reports to date
| Author (Ref) | Year | No. of cases | Age | Site | Clinical diagnosis | Cells | Amyloid type |
| Fernandez and Hernandez (1) | 1973 | 1 | 62 | RUO | Cancer | P+L+G | – |
| Walker et al (2) | 1982 | 1 | 55 | LUO | – | P+L+G | – |
| McMahon et al (3) | 1984 | 1 | 54 | R | Cancer | P+L | AL (κ) |
| Lew and Seymour (4) | 1985 | 1 | 63 | RUO | Cancer | P+L | AA |
| Silverman et al (6) | 1986 | 2 | 67 | R | Cancer | P+L+G | AL (IgA) |
| 79 | L | Cancer | P+L+G | AL (IgG) | |||
| Cheung et al (5) | 1986 | 1 | 82 | Bi | Cancer | P+L+G | – |
| Santini et al (15) | 1992 | 1 | 75 | L | Cancer | – | – |
| Lynch and Moriaty (11) | 1993 | 1 | 72 | Bi | Cancer | L+G | AL (IgG) (κ) |
| Gupta and Dowle (13) | 1996 | 1 | 43 | L | Cancer | P | AL |
| Luo and Rotterdam (7) | 1997 | 1 | 82 | R | Cancer | L+G | AA |
| Yokoo and Nakazato (12) | 1998 | 1 | 76 | R | Fibroadeoma | P+G | AL |
| Gupta et al (14) | 2000 | 1 | 64 | L | Cancer | P+L+G | P component |
| Deolekar et al | 2002 | 1 | 86 | L | Cancer | P+L+G | AL |
Site: Bi, bilateral; L, left; LUO, left upper quadrant; R, right; RUO, right upper quadrant. Cells: G, giant cells; L, lymphocytes; P, plasma cells.
In breast screening units, fine needle aspiration cytology is now a routine tool to distinguish benign and malignant lesions. The cytological findings in amyloid tumour have been reported in four cases.4,6,11,13 As in our patient, the presence of amyloid in the fine needle aspirate was only noticed retrospectively in all these reports.
“The AL nature of localised amyloidosis is now thought to be derived from localised plasma cells secreting immunoglobulins; that is, immunocyte derived amyloid”
To date, the histochemical nature of amyloid has been determined in nine of 13 cases (table 1). Of these, only two had AA amyloid and the remaining cases, including our own, had AL amyloid. The AA amyloid was associated with a carcinoma in one patient4 and it was thought to be the result of an abnormal immune response in the other.7
Most patients with the AL type of amyloid do not have classic multiple myeloma or an overt B cell neoplasm. Such cases have traditionally been classified as primary amyloidosis because their clinical features derive from the effects of amyloid deposition with no other associated disease.9 The AL nature of localised amyloidosis is now thought to be derived from localised plasma cells secreting immunoglobulins; that is, immunocyte derived amyloid.9 In our patient, there were many plasma cells containing Russel bodies in the vicinity of the amyloid. Considering the clinical details of our patient the localised breast amyloidosis is probably primary.
In summary, localised breast amyloidosis is a rare entity and can have a diverse aetiology. It occurs in elderly women and is clinically and mammographically suspicious of carcinoma. If breast screening is extended to older age groups, this lesion could be diagnosed more frequently.
Take home messages .
We report a case of amyloidosis localised to the breast
This is a rare entity that can have a diverse aetiology
This lesion occurs mostly in elderly women and is clinically and mammographically suspicious of carcinoma
If breast screening is extended to older age groups, it may be diagnosed more frequently
REFERENCES
- 1.Fernandez BB, Hernandez FJ. Amyloid tumour of the breast. Arch Pathol 1973;95:102–5 . [PubMed] [Google Scholar]
- 2.Walker AN, Fechner RE, Callicott JH. Amyloid tumour of the breast. Diagnostic Gynaecology and Obstetrics 1982;4:339–41. [PubMed] [Google Scholar]
- 3.McMahon RFT, Waldron D, Given HF, et al. Localised amyloid tumour of the breast, a case report. International Journal of Medical Science 1984;159:323–4. [DOI] [PubMed] [Google Scholar]
- 4.Lew W, Seymour AE. Primary amyloid tumor of the breast. Acta Cytol 1985;29:7–11. [PubMed] [Google Scholar]
- 5.Cheung PSY, Yan KW, Alagaratnam TT, et al. Bilateral amyloid tumours of the breast. Aust N Z J Surg 1986;56:375–7. [DOI] [PubMed] [Google Scholar]
- 6.Silverman JF, Drabbs DJ, Norris HT et al. Localised primary (AL) amyloid tumour of the breast. Am J Surg Pathol 1986;10:539–45. [DOI] [PubMed] [Google Scholar]
- 7.Luo JH, Rotterdam H. Primary amyloid tumour of the breast: a case report and review of the literature. Mod Pathol 1997;10:735–8. [PubMed] [Google Scholar]
- 8.Virchow R. Weitere Mitteilugen uber das Vorkommen der pflanzlichen Cellulose beim Menschen. Virchows Arch Pathol Anat Physiol Kin Med 1854;6:268. [Google Scholar]
- 9.Cotran Ramzi S, Kumar V, Collins T. Diseases of immunity. In: Robbins pathologic basis of disease, 6th ed. W B Saunders, 1999:188–259.
- 10.Wright JR, Calkins E, Humphrey RL. Potassium permanganate reaction in amyloidosis, a histological method to assist in differentiating forms of this disease. Lab Invest 1977;36:274–81. [PubMed] [Google Scholar]
- 11.Lynch LA, Moriarty AT. Localised primary amyloid tumour associated with osseous metaplasia presenting as bilateral breast masses, cytologic and radiologic features. Diagn Cytopathol 1993;9:570–5. [DOI] [PubMed] [Google Scholar]
- 12.Yokoo H, Nakazato Y. Primary localised amyloid tumour of the breast with osseous metaplasia. Pathol Int 1998;48:545–8. [DOI] [PubMed] [Google Scholar]
- 13.Gupta RK, Dowle CS. Cytodiagnosis of amyloid deposition within the breast. Cytopathology 1996;7:136–40. [DOI] [PubMed] [Google Scholar]
- 14.Gupta D, Shidham V, Zemba-Palco V, et al. Primary bilateral mucosa-associated lymphoid tissue lymphoma of the breast with atypical ductal hyperplasia and localised amyloidosis, a case report and review of the literature. Arch Pathol Lab Med 2000;124:1233–6. [DOI] [PubMed] [Google Scholar]
- 15.Santini D, Pasquinelli G, Alberghini M, et al. Invasive breast carcinoma with granulomatous response and deposition of unusual amyloid. J Clin Pathol 1992;45:885–8. [DOI] [PMC free article] [PubMed] [Google Scholar]