Abstract
Background: The “International consensus statement on testing and reporting antineutrophil cytoplasmic antibodies (ANCA)” advocates screening by indirect immunofluorescence (IIF), but external quality assessment programmes often demonstrate different IIF patterns for a single serum.
Aim: To determine whether the variation in IIF patterns can be attributed solely to errors in interpretation.
Methods: This study compared the IIF patterns produced by four sera (two with cytoplasmic or C-ANCA; one with perinuclear or P-ANCA with myeloperoxidase (MPO) specificity; and one P-ANCA without MPO specificity) that were tested in 11 different laboratories. The sera were examined according to individual laboratory protocols at dilutions of 1/10 to 1/40 using P1 (n = 4), P2 (n = 2), P3 (n = 2), or in house (n=3) neutrophil preparations and conjugates from manufacturers C1 (n = 3), C2 (n = 1), C3 (n = 2), C4 (n = 1), C5 (n = 2), and C6 (n = 2). The IIF patterns were noted in each laboratory, the testing repeated, and the fluorescent patterns photographed and subsequently discussed at a meeting of the Australian ANCA study group.
Results: All IIF patterns described in individual laboratories were confirmed on retesting and by the ANCA study group. Neutrophil substrates produced commercially or in house varied in their ability to demonstrate cytoplasmic granularity and interlobular accentuation, which distinguish between “C-ANCA” and “C-ANCA (atypical)”. All commercial and in house neutrophil substrates demonstrated neutrophil nuclear extension of P-ANCA fluorescence, which correlates with MPO specificity. However, eight assays (eight of 43) from eight laboratories resulted in IIF patterns different from those usually seen. One of these produced a C-ANCA (atypical) rather than a C-ANCA pattern. The other seven resulted in at least some cytoplasmic fluorescence when the consensus pattern was P-ANCA with (n = 4) or without (n = 3) MPO specificity. These assays used three different commercial and one in house neutrophil substrate, and six different conjugates, with anti-IgG, anti-(Fab)`2, anti-Ig (heavy and light chain), and anti-G, A, and M activity. Four of the seven assays tested on commercial substrates had used the manufacturer's conjugates.
Conclusions: This study indicates that the variation in IIF patterns seen with ANCA positive sera tested in different laboratories does not necessarily result from errors in the interpretation of patterns and cannot be attributed solely to the use of a particular neutrophil substrate or conjugate, or to the use of substrate from one manufacturer and conjugate from another.
Keywords: antineutrophil cytoplasm antibodies, indirect immunofluorescence, vasculitis, Wegener's granulomatosis
Antineutrophil cytoplasmic antibodies (ANCA) are autoantibodies directed against antigens found in the cytoplasmic granules of neutrophils and monocytes.1 These antibodies occur at presentation in most patients with active Wegener's granulomatosis or microscopic polyangiitis1,2 (reviewed in Savige and colleagues3).
The “International consensus statement on testing and reporting antineutrophil cytoplasmic antibodies (ANCA)”4 advocates that all laboratories screen for ANCA by indirect immunofluorescence (IIF), and that any sera with cytoplasmic or perinuclear fluorescence, or nuclear fluorescence that might mask an ANCA, should be tested for both the major ANCA specificities, proteinase 3 (PR3) and myeloperoxidase (MPO) by enzyme linked immunoassay (ELISA). The conditions for IIF and the ELISAs have been described in detail.3–6
“Cytoplasmic antineutrophil cytoplasmic antibodies (C-ANCA) have to be distinguished from C-ANCA (atypical), where the fluorescence is flatter, and there is no accentuation of the interlobular fluorescence or granular staining”
The consensus statement describes two fluorescence patterns that occur in patients with Wegener's granulomatosis and microscopic polyangiitis. Cytoplasmic fluorescence (C-ANCA) is diffuse cytoplasmic staining with coarse granular and central interlobular accentuation. It is seen in most patients with active generalised Wegener's granulomatosis, and is usually the result of PR3 specificity.7 With perinuclear fluorescence (P-ANCA), the nuclear lobes are outlined, and there is some nuclear extension when the specificity is MPO. MPO-ANCA occur in about 60% of patients with microscopic polyangiitis,8 but sometimes patients with microscopic polyangiitis have P-ANCA with PR3 specificity, or C-ANCA with PR3 or MPO specificity.9
C-ANCA have to be distinguished from C-ANCA (atypical), where the fluorescence is “flatter”, and there is no accentuation of the interlobular fluorescence or granular staining. This pattern occurs as often as C-ANCA in a routine testing laboratory, but is not present in the systemic vasculitides.10 It is found mainly in rheumatoid arthritis, inflammatory bowel disease, cystic fibrosis, and in infections.
The other category of atypical ANCA is uncommon, and usually caused by a combination of both cytoplasmic and perinuclear fluorescence. These sera have multiple antigenic specificities including PR3, MPO, bactericidal permeability increasing protein, cathepsin G, elastase, lactoferrin, and lysozyme.3,4 Atypical ANCA occur in inflammatory bowel disease, some autoimmune forms of arthritis, and drug induced vasculitides. The consensus statement recommends that sera with C-ANCA (atypical) and atypical ANCA should be tested in ELISAs for both PR3-ANCA and MPO-ANCA.
ANCA testing is widespread in Australia, and external quality assessment programmes have demonstrated an unexplained variation in the IIF patterns for individual test sera. The aim of our study was to determine whether this variation is caused by errors in the interpretation of ANCA patterns.
METHODS
Sera with C-ANCA and PR3 specificity (n = 2) (producing 3+ or 2+ fluorescence), P-ANCA with MPO specificity (3+) (n = 1), and P-ANCA without MPO specificity (3+) (n = 1) were selected by the reference laboratory that coordinates external quality assessment testing for ANCA in Australia. Sera were chosen that were typical of the C-ANCA found in Wegener's granulomatosis and the P-ANCA found in microscopic polyangiitis or inflammatory bowel disease. None of the sera contained antinuclear antibodies when tested on HEp2 cells.
Each serum was distributed to 11 laboratories and tested with the neutrophil substrates, serum dilutions, and conjugate type and dilutions used routinely in that laboratory (table 1). Substrates and conjugates have been coded, and P1 and C1, P2 and C2, etc are from the same manufacturer. All in house neutrophil preparations were made according to the published method.5 Slides were then examined using ultraviolet microscopy, and the IIF patterns described and strength of fluorescence graded from 0 (negative) to 3+ (strong). The process was repeated, the fluorescence patterns were photographed, and the patterns and intensity of staining were subsequently characterised by members of the Australian ANCA study group at a face to face meeting. The “consensus” pattern was the pattern seen in most laboratories.
Table 1.
Immunofluorescence patterns seen with four sera tested in 11 different laboratories
| Laboratory | PMN | Serum dilution | Conjugate dilution | X | Serum A | Serum B | Serum C | Serum D |
| GRI | P1 | 1/40 | C4 IgG (H&L), prediluted | 400 | Cytoplasmic 3+, i2+, g3+ | Cytoplasmic 2+, i+, g− | Perinuclear with nuclear extension 3+, cytoplasmic 2+ | Perinuclear rim only 3+ |
| ARM | P1 | 1/20 | C5 IgG F(ab`)2, 1/100 | 400 | Cytoplasmic 3+, i2+, g3+ | Cytoplasmic 2+, i+, g+ | Perinuclear with nuclear extension 3+, cytoplasmic 2+ | Perinuclear rim only 3+ |
| ALF | P1 | 1/40 | C1 IgG prediluted | 600 | Cytoplasmic 3+, i +, g+ | Not done | Perinuclear with nuclear extension 3+, cytoplasmic 2+ | Perinuclear rim only 2+ |
| STG | P1 | 1/40 | C1 IgG prediluted | 250 | Cytoplasmic 2+, i2+, g2+* | Cytoplasmic 2+, i2+, g+ | Perinuclear with nuclear extension 3+ | Perinuclear rim only 3+ |
| SOC | P2 | 1/20 | C2 IgG, IgA, IgM, prediluted | 400 | Cytoplasmic 2+, i+, g+ | Cytoplasmic 2+, flat atypical, i−, g− | Perinuclear with ? nuclear extension 3+ | Perinuclear rim only 2+ |
| RMH | P2 | 1/40 | C6 Ig F(ab`)2, 1/200 | 400 | Cytoplasmic 2+, i2+, g+ | Cytoplasmic 2+, i+, g− | Perinuclear with nuclear extension 3+, ? cytoplasmic extension 1+ | Perinuclear rim only 3+ |
| IMM | P3 | 1/20 | C3 IgG (H&L) prediluted | 400 | Small cytoplasm, cytoplasmic 2+, i2+, g+ |
Cytoplasmic 2+, small cytoplasm, i+, g− | Perinuclear with nuclear extension 3+ | ? Perinuclear rim only 3+; almost cytoplasmic |
| FMC | P3 | 1/40 | C3 IgG (H&L) prediluted | 600 | Small cytoplasm, cytoplasmic 2+, i2+, g+ | Cytoplasmic 2+, small cytoplasm, i+, g− | Perinuclear with nuclear extension 3+ | ? Perinuclear rim only 3+, ?cytoplasmic extension |
| RBH | In house | 1/10 | C6 Ig (H&L), F(ab`)2 1/200 | 400 | Cytoplasmic 3+, i+, g+ | Cytoplasmic 2+, no outer margin, i +, g− | Perinuclear with nuclear extension 3+ | Perinuclear rim only 3+ |
| STV | In house | 1/40 | C5 IgG F(ab`)2, 1/1000 | 400 | Cytoplasmic 3+, i2+, g+ | Cytoplasmic 2+, i+, g+ | Perinuclear with nuclear extension 3+ | Cytoplasmic 3+ (i 2+, g 2+) |
| RPA | In house | 1/20 | C1 IgG prediluted | 400 | Cytoplasmic 3+, i +, g− | Cytoplasmic 2+, i+, g+ | Perinuclear with nuclear extension 3+ | Perinuclear rim only 3+ |
Neutrophil preparations and substrates from the same manufacturer have the same suffix; fluorescence is described as 0 to 3+; i0–3+, interlobular or central accentuation of cytoplasmic fluorescence; g0–3+, granularity of cytoplasmic fluorescence.
ANA, antinuclear antibody; C1–C6, conjugate preparations; H&L, antiserum against both heavy and light chains; P1–P3, neutrophil preparations; PMN, neutrophil preparations; X, magnification at which neutrophils were examined.
RESULTS
All test sera were positive for ANCA by IIF in each of the 11 laboratories. All fluorescence patterns were consistent between the first and second testing in each laboratory, and with the description at the meeting of the Australian ANCA study group. Thus, variations in IIF patterns cannot be attributed solely to errors in interpretation.
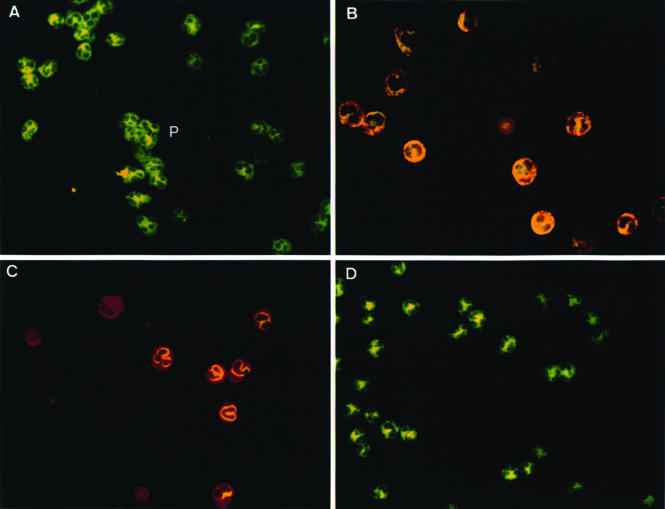
The observed IIF patterns were inconsistent with the consensus patterns in eight assays, each from a different laboratory (eight of 43) (table 1; fig 1). One of these produced a C-ANCA (atypical) rather than a C-ANCA pattern. The other seven resulted in at least some cytoplasmic fluorescence when the consensus pattern was P-ANCA with (n = 4) or without (n = 3) MPO specificity. The intensity of fluorescence for all sera varied by 1+ at most between assays and laboratories.
Figure 1.
Indirect immunofluorescence showing: (A) Serum C producing perinuclear antineutrophil cytoplasmic antibodies (P-ANCA) with nuclear extension (laboratory STV from table 1 (P); (B) Serum C producing perinuclear fluorescence with nuclear extension (3+) and cytoplasmic staining (2+) (laboratory GRI); (C) Serum D producing P-ANCA with perinuclear rim pattern only (not specific for myeloperoxidase) (laboratory GRI). (D) Serum D producing cytoplasmic fluorescence (C-ANCA) (laboratory STV).
Neutrophil substrates varied in their ability to demonstrate the consensus IIF patterns. In general, C-ANCA was demonstrated well but substrates differed in their ability to distinguish between a C-ANCA and C-ANCA (atypical). P1 neutrophils demonstrated C-ANCA in all four laboratories and the cytoplasmic granularity and central accentuation were more prominent and more consistent than with other neutrophil preparations. P2 neutrophils were satisfactory where there was strong cytoplasmic fluorescence, but the central accentuation and granularity of weaker cytoplasmic staining were not easily demonstrated, resulting in a C-ANCA being interpreted as a C-ANCA (atypical). Both the P3 and in house neutrophils were too small for cytoplasmic fluorescence to be demonstrated clearly.
All three commercial and three in house neutrophil substrates consistently demonstrated nuclear extension of perinuclear fluorescence with sera containing P-ANCA with MPO specificity. However seven assays of sera containing P-ANCA demonstrated (mostly) additional cytoplasmic fluorescence with each of the three different commercial substrates and one in house assay. In one case only cytoplasmic fluorescence was present.
Of the eight assays that resulted in IIF patterns that differed from the consensus, seven used commercial neutrophil substrates and one an in house substrate. Conjugates included anti-IgG, anti-F(ab`)2, anti-IgG (heavy and light chains), and anti-IgG, A, and M. All six conjugates produced an abnormal IIF pattern on at least one occasion. Of the seven assays tested on commercial substrates, four had been performed using the manufacturer's conjugates, and three had not.
DISCUSSION
The 11 laboratories participating in our study used different patient serum dilutions, neutrophil substrates, conjugates, and microscope magnifications to examine the test sera. All four sera were considered positive for ANCA by IIF in all the laboratories, most patterns were correctly identified as C-ANCA or P-ANCA, and the fluorescence intensities were generally consistent between assays and laboratories. All descriptions of IIF patterns were confirmed on retesting in individual laboratories and on review by the Australian ANCA study group. The participating laboratories comprised the ANCA study group, members of which have a particular interest and expertise in ANCA testing. This may have biased our findings away from those obtained in inexperienced laboratories, where variations in IIF patterns may result from observer error. However, our study demonstrates that variations in ANCA IIF patterns do not necessarily result from the misinterpretation of patterns, but may result from other, probably technical, factors.
In our study, neutrophil substrates from different manufacturers varied in their ability to demonstrate interlobular fluorescence and cytoplasmic granularity, and thus to differentiate between a C-ANCA and C-ANCA (atypical) pattern. However, most laboratories distinguished successfully between these patterns. Although all three commercial and three in house neutrophil substrates demonstrated the nuclear extension of P-ANCA that correlates with MPO specificity, there were, in general, more problems testing sera containing P-ANCA.
Eight assays from eight different laboratories resulted in IIF descriptions that differed from the consensus patterns. These were mostly caused by additional cytoplasmic fluorescence and were found in sera with P-ANCA with or without MPO specificity. However, this preliminary study suggests that the development of cytoplasmic fluorescence in sera containing P-ANCA cannot be attributed solely to the use of a particular neutrophil substrate or conjugate, or to the combination of substrate from one manufacturer and conjugate from another. The explanation for the development of cytoplasmic fluorescence is unclear but may relate to the use of alcohol in neutrophil fixation because this permeabilises the membranes and allows the normally cytoplasmic MPO to diffuse around the nucleus to produce the perinuclear pattern. Cytoplasmic fluorescence may also result from delays in examining the substrate, which allows the perinuclear MPO to diffuse back into the cytoplasm. Finally, cytoplasmic fluorescence may result from the use of polyspecific antiserum that detects additional IgA or IgM ANCA.
“The explanation for the development of cytoplasmic fluorescence is unclear but may relate to the use of alcohol in neutrophil fixation because this permeabilises the membranes”
Take home messages.
All four sera were positive for antineutrophil cytoplasm antibody (ANCA) by indirect immunofluorescence (IIF) in all the laboratories, most patterns were correctly identified as cytoplasmic or perinuclear ANCA, and the fluorescence intensities were generally consistent between assays and laboratories
The variations that did occur were mostly caused by additional cytoplasmic fluorescence and were found in sera with perinuclear ANCA, with or without myeloperoxidase specificity
Variations in ANCA IIF patterns do not necessarily result from the misinterpretation of patterns, but may result from other, probably technical, factors
Such variations cannot be attributed solely to the use of a particular neutrophil substrate or conjugate, or to the use of substrate from one manufacturer and conjugate from another
The international consensus statement emphasises that IIF is a screening test for ANCA,4 and that assays for both PR3-ANCA and MPO-ANCA should be performed on all IIF positive sera. However, some laboratories test for ANCA by IIF alone, and about 10% of patients with systemic vasculitides are positive only by IIF. In our study, the interlaboratory variation in the character of fluorescence patterns and intensity was surprisingly small considering the differences in substrates, conjugates, and ultraviolet microscopy techniques. Our results indicate that the variation in interpretation of ANCA fluorescence patterns seen with individual sera cannot be attributed solely to errors in observer interpretation.
Abbreviations
ANCA, antineutrophil cytoplasmic antibodies
C-ANCA, cytoplasmic antineutrophil cytoplasmic antibodies
ELISA, enzyme linked immunoassay
IIF, indirect immunofluorescence
MPO, myeloperoxidase
P-ANCA, perinuclear antineutrophil cytoplasmic antibodies
PR3, proteinase 3
This work represents a collaboration of the Australian ANCA study group.
The manufacturers of the P3 substrate have dealt with the issue of small neutrophil cytoplasmic volume.
REFERENCES
- 1.van der Woude FJ, Rasmussen N, Lobatto S, et al. Autoantibodies against neutrophils and monocytes: tool for diagnosis and marker of disease activity in Wegener's granulomatosis. Lancet 1985;i:425–9. [DOI] [PubMed] [Google Scholar]
- 2.Savage CO, Winearls CG, Jones S, et al. Prospective study of radioimmunoassay for antibodies against neutrophil cytoplasm in diagnosis of systemic vasculitis. Lancet 1987;i:1389–93. [DOI] [PubMed] [Google Scholar]
- 3.Savige JA, Davies DJ, Wiik A, et al. Antineutrophil cytoplasmic antibodies (ANCA) and associated diseases. Kidney Int 2000;57:846–62. [DOI] [PubMed] [Google Scholar]
- 4.Savige JA, Gillis D, Benson E, et al. International consensus statement on testing and reporting of antineutrophil cytoplasmic antibodies (ANCA). Am J Clin Pathol 1999;111:507–13. [DOI] [PubMed] [Google Scholar]
- 5.Wiik A. Delineation of a standard procedure for indirect immunofluorescence detection of ANCA. APMIS 1989;6:12–13. [PubMed] [Google Scholar]
- 6.Wiik A, Rasmussen N, Wieslander J. Methods to detect autoantibodies to neutrophilic granulocytes. In: van Venrooij WJ, Maini RN, eds. Manual of biological markers of disease. The Netherlands: Kluwer Academic Publishers, 1993:1–14.
- 7.Niles JL, McCluskey RT, Ahmad MF, et al. Wegener's granulomatosis autoantigen is a novel neutrophil serine proteinase. Blood 1989;74:1888–93. [PubMed] [Google Scholar]
- 8.Falk RJ, Jennette JC. Antineutrophil cytoplasmic autoantibodies with specificity for myeloperoxidase in patients with systemic vasculitis and idiopathic necrotising and crescentic glomerulonephiritis. N Engl J Med 1988;318:1651–7. [DOI] [PubMed] [Google Scholar]
- 9.Segelmark M, Baslund B, Wieslander J. Some patients with antimyeloperoxidase antibodies have a cANCA pattern. Clin Exp Immunol 1994;96:458–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wong RCW, Silvestrini RA, Savige JA, et al. Diagnostic value of classical and atypical cytoplasmic antibodies (ANCA) immunofluorescence patterns. J Clin Pathol 1999;52:124–8. [DOI] [PMC free article] [PubMed] [Google Scholar]