Abstract
Aim: To evaluate recent trends in alcohol related deaths in the UK and to consider possible causative factors.
Design: Observational retrospective study of the database of the Office for National Statistics, alcohol consumption data reported by the General Household Survey, and other published data.
Setting: England, 1993–9.
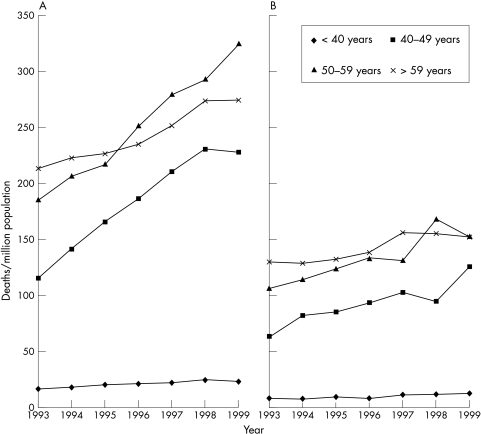
Results: Deaths for each million of the population from alcohol related illness increased by 59% in men and 40% in women over the years 1993 to 1999. One subgroup of alcohol related deaths, ICD 571.3 (alcoholic liver damage unspecified), showed a 243% increase in men aged 40 to 49 years over the same period. Figures for younger men, and women in all age groups, showed less pronounced increases. There has been no associated rise in alcohol intake. There has been an increase in the incidence of hepatitis C virus (HCV) infection in recent years, and alcohol consumption in HCV positive individuals accelerates the progression to cirrhosis. Circumstantial evidence links the rise in HCV infection to the use of illicit drugs in the 1970s and 1980s, among those currently aged 40 to 59 years.
Conclusions: The recent increase in alcohol related deaths cannot be solely explained by a change in drinking habits. It is suggested that this probably results from the rapid progression of alcoholic cirrhosis in people who have acquired HCV infection through intravenous drug use. Alcohol consumption in HCV positive individuals is firmly linked with a poor outcome.
Keywords: alcohol, hepatitis C, cirrhosis, mortality, drug misuse
Alcohol related deaths have shown a sharp increase in recent years in the UK.1 An individual's risk of death from alcohol depends on a variety of factors. Patterns of consumption are probably most influential, but other factors are also important.2 For example, hepatitis C virus (HCV) positive individuals who also consume alcohol have accelerated liver damage, a higher frequency of cirrhosis, and a higher incidence of hepatocellular carcinoma.3 In HCV infected individuals, even drinking an average of 40 g alcohol (4 units) each day can hasten the progression towards liver cirrhosis.4,5 Therefore, we wished to explore the hypothesis that the rise in alcohol related deaths is associated with an increase in the incidence of HCV infection.
METHODS
Numbers of deaths from alcohol related illness for England for the years 1993–9 were obtained from the Office of National Statistics. Trends in these data were considered overall and separately for each ICD9 (International Classification of Diseases, 9th revision) category. Men and women were subdivided into different age groups. Deaths were adjusted to take into account the population of each sex and age group for each year. Trends in ICD9 subcategory 571.3 (alcoholic liver damage unspecified) and alcohol related deaths overall were compared with trends in alcohol consumption1,6 and data on HCV infection.7–14 Data were collated and the trends analysed using Microsoft Excel; p values were determined from the standard error of the regression coefficient.
Data on alcohol consumption were obtained from the General Household Survey.6 We searched the websites of the Office for National Statistics, the National Health Service, and the Public Health Laboratory Services (PHLS) and Medline for statistics on HCV.
RESULTS
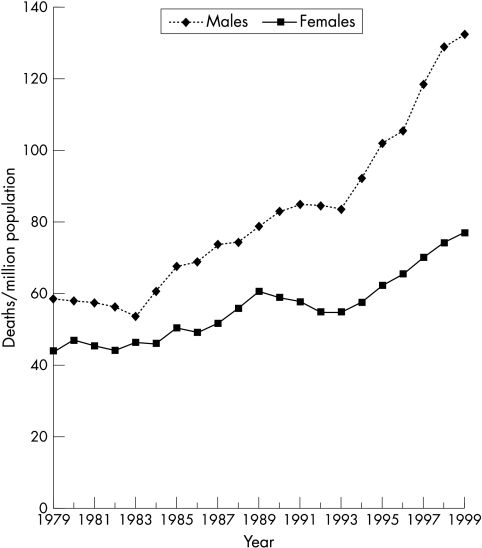
There has been a gradual rise in alcohol related deaths over the past two decades, which has generally been at a steadily progressive rate, with an apparent increase in rate during the years 1993 to 1999 (fig 1). Numbers of deaths for each million of the population from alcohol related illness rose by 58.7% in men and 40.1% in women in England between 1993 and 1999 (table 1; fig 1).
Figure 1.
Death rate from alcohol related diseases in men and women, England and Wales, 1979–1992, England 1993–1999.
Table 1.
Percentage increases in age corrected alcohol related deaths, England 1993–9
| Age (years) and sex | |||||||||||||||
| <40 | 40–49 | 50–59 | >59 | All ages | |||||||||||
| M | F | M | F | M | F | M | F | M | F | ||||||
| All alcohol related deaths | 42.85 | 98.39* | 63.01* | 24.47 | 51.42 | ||||||||||
| 36.98 | 53.17 | 98.38 | 98.84 | 74.54* | 43.78 | 28.68 | 16.87 | 58.68 | 40.14 | ||||||
| All ICD 571.3 deaths | 156.03 | 243.82*** | 188.25 | 147.44 | 189.57 | ||||||||||
| 184.83 | 115.7 | 276.4* | 202.36 | 234.33* | 124.55* | 181.18 | 99.24 | 228.06 | 137.50 | ||||||
| All alcohol related deaths other than ICD 571.3 | 15.86 | 58.95 | 31.1 | 6.89 | 24.13 | ||||||||||
| 7.94 | 33.0 | 57.62 | 61.15 | 37.61 | 19.3 | 6.98 | 5.62 | 26.98 | 19.33 | ||||||
*p<0.05; **p<0.01; ***p<0.001.
F, female; ICD, International Classification of Diseases; M, male.
Fifty two per cent of the increase in deaths in men aged 40 to 59 years resulted from increases in the ICD9 category 571.3; other categories of alcohol related mortality showed smaller increases and none showed a decrease (table 1).
There was an increase in cross channel importation of alcohol from the mid 1990s according to the General Household Survey.6 However, figures for the weekly consumption of alcohol in the UK did not change in men from 1986 to 1996, the two years compared in the survey, being 16.3 and 16.0 units/week, respectively, although they increased by 19% (from 5.3 to 6.3 units) in women.1,6 The proportion drinking more than 21 units (men) or 14 units (women) each week was the same for men in 1986 and 1996 (at 27%), whereas the figures for women were 10% and 14% respectively.1,6 Figures for the weekly consumption of alcohol decreased with age in both men and women in both years.1,6
A search of the literature revealed estimates of around 5 million chronic carriers of HCV in Western Europe.9,13 Recent data for the UK give estimates of between 0.1% and 1% HCV prevalence in the general population, or 300 000 of the UK population.10–12,14 There are few available data on changes in prevalence of HCV infection in the UK overall. PHLS data show an increase in laboratory reports of confirmed HCV, year on year from 1992, with 241 cases in 1992, rising to 5108 in 2000. One study of the Glasgow area of Scotland considered postmortem data from 370 drug related deaths occurring between 1995 and 1998, and found an increase in cases of HCV in this group from two in 1995 to 46 in 1998.
DISCUSSION
The rise in alcohol related deaths between 1993 and 1999 was largely the result of increases in the ICD9 category 571.3 (alcoholic liver damage unspecified), whereas other causes of alcohol related mortality showed relatively small increases. The descriptor for ICD9 571.3 suggests that the precise nature of the pathology included in this category may not have been verified. We can only presume that there were reasonable grounds for suspecting a large alcohol intake by the deceased, and that any pathology found was consistent with alcoholic liver disease. The progressive rise in deaths each year since 1993 strongly suggests that it is not an artefact. It may be that doctors and pathologists cite alcohol more freely as a cause of death because of changes in social factors. However, even if this were the case, it would be unlikely to cause such a dramatic rise in the numbers of deaths. Several studies have indicated the unreliability of death certification with respect to liver disease.3 However, the rises in both overall alcohol related deaths and deaths confined to category ICD 571.3 suggest that the increase is real.
The most obvious explanation for the recent dramatic increase in alcohol related deaths would be that this reflects a corresponding change in alcohol consumption. A significant fall in alcohol consumption occurred between 1979 and 1982 in the UK, which was associated with a pronounced decrease in deaths from cirrhosis, pancreatitis, and cancer of the oesophagus.15 However, although there was an increase in cross channel importation of alcohol from the mid 1990s, there has not been an appreciable rise in intake that could explain the increased deaths in men. The proportion of women drinking over 14 units increased by 40% between 1986 and 1996. However, the fact that the ICD 571.3 death rates increased more in men than women over this period suggests that a factor other than increased consumption is operating.
Alcohol consumption in HCV positive individuals is firmly linked with a poor outcome.16 About 20% of HCV infected individuals will progress to cirrhosis over an average of approximately 30 years.4 The HCV positive individual who also consumes alcohol has a 31 times higher frequency of liver cirrhosis.17 In addition, it has been estimated that 30% of patients with alcoholic liver disease are infected with HCV.16
HCV infection is a worldwide health issue of increasing importance. There are reports of a current epidemic.18 According to PHLS data, there was a substantial and consistent rise in the number of reported laboratory confirmed cases of HCV in England and Wales over the period that we were investigating here: from 435 in 1993 to 5745 in 1999. This is consistent with our hypothesis. Our data indicate that men (aged 40–49 and 50–59 years) contribute most to the increase in alcohol related deaths over a similar period. An analysis of 9987 HCV positive patients in Scotland in 1999 showed that 69% were male. Similarly, according to the PHLS, 66% of HCV positive patients in England and Wales are male.
PHLS data between 1992 and 1996 suggest that over 80% of HCV transmission is associated with injecting drug use.12
Therefore we looked at data on intravenous drug misuse to see whether there were any trends that correlated with the rise in alcohol related deaths. There is no evidence that those currently aged 40 to 59 years (that is, the cohort contributing most to the increase in alcohol related death in our sample) have a higher lifetime history of illicit drug use than earlier cohorts. But this is the cohort that would have been involved in the epidemic of illicit drug use that took hold in the 1970s and 1980s.19 Importantly, this was before the introduction of needle exchange and other interventions instigated in the late 1980s to reduce the risk of human immunodeficiency virus (HIV) transmission in drug users.20 In England and Wales, 64% of PHLS laboratory reports of HCV infection are in 24–44 year olds. In the USA, the prevalence of HCV infection is threefold higher among persons aged 30 to 49 years of age than in any other age group, and it is anticipated that the number of deaths from HCV infection will increase substantially during the next 10 to 20 years, as this cohort reaches the age at which complications from chronic liver disease typically develop.21,22
Most people who develop HCV infection are unaware that they are infected until a blood test reveals the diagnosis, because both the acute disease and the carrier state are largely asymptomatic.14 A total of 13 272 positive HCV tests was recorded by the PHLS by 31 December 1998, which suggests that fewer than 5% of the 300 000 people officially estimated to be HCV positive in the UK are aware of their infection.12 At least 85% of infected individuals with HCV become chronic carriers, who may remain asymptomatic for years.
The histopathology of alcoholic liver disease and chronic HCV are very similar and show considerable overlap, with fatty change and lobular inflammation being common to both.23 Clinicians and pathologists could fail to recognise HCV infection as a cause of rapid progression of alcoholic liver disease unless the virus is specifically tested for. It is also of relevance that a large proportion of drug misusers (those at particular risk of HCV infection) are also problem drinkers.24 Before the rise of HIV, alcohol related deaths were the main cause of mortality in drug misusers.25 We do not know how many alcohol related deaths have already been caused by HCV but have been overlooked. We conclude that the rising mortality figures for alcohol related diseases are best explained by rapidly progressive fatal liver disease in drinkers with HCV infection. Postmortem surveys are needed to confirm our interpretation of the data. These would help to establish the rate of seropositivity for HCV in people who have apparently died from alcoholic liver disease and confirm the impact of HCV infection on national mortality figures for alcohol induced liver disease. There is already sufficient indication of this problem to recommend routine testing of all patients with clinical evidence of alcoholic liver disease. McCusker has shown that people who know they are HCV positive and are aware of the effect of HCV on the progression of liver disease are prepared to reduce their consumption of alcohol.26 Unfortunately, Best et al found that in a sample of 106 injecting opiate addicts attending a methadone maintenance clinic in London, 86% were seropositive for HCV but substantial numbers of these thought that they were seronegative.27 Therefore, testing patients for HCV status, and counselling them about the effect of alcohol on its progression can give them the opportunity to modify their drinking habits so as to increase the chances of successful treatment and longer survival.
Take home messages.
Deaths for each million of the population from alcohol related illness increased by 59% in men and 40% in women over the years 1993 to 1999, although there has been no associated rise in alcohol intake in men
This increase probably results from the rapid progression of alcoholic cirrhosis in people who have acquired hepatitis C (HCV) infection through intravenous drug use
Testing patients for HCV status and advising them about the effect of alcohol on its progression would give them the opportunity to modify their drinking habits so as to increase the chances of successful treatment and longer survival
Figure 2.
Death rate from alcohol related diseases by age and sex, England, 1993–1999. (A) Men, (B) women.
Acknowledgments
We thank Professor P Elliott for his advice and encouragement and A Baker and G Meredith of the Office of National Statistics for help in providing data.
Abbreviations
ICD, International Classification of Diseases
HCV, hepatitis C virus
PHLS, Public Health Laboratory Services
REFERENCES
- 1.Department of Health. Statistics on alcohol: 1976 onwards. Statistics Bulletin 1999/24. London: Department of Health, 1999.
- 2.Edwards G, Anderson P, Babor TF, et al. Alcohol policy and the public good. London: Oxford University Press, 1995.
- 3.Deuffic S, Poynard T, Valleron A-J. Correlation between hepatitis C virus prevalence and hepatocellular carcinoma mortality in Europe. J Viral Hepat 1999;6:411–13. [DOI] [PubMed] [Google Scholar]
- 4.Degos F. Hepatitis C and alcohol. J Hepatol 1999;31(suppl 1):113–18. [DOI] [PubMed] [Google Scholar]
- 5.Nevins CL, Malaty H, Velez ME, et al. Interaction of alcohol and hepatitis C virus infection on severity of liver disease. Dig Dis Sci 1999;44:1236–42. [DOI] [PubMed] [Google Scholar]
- 6.Department of Health. General Household Survey. London: Department of Health, 1998, 2000.
- 7.Infectious diseases. Hepatitis C. (http://www.show.scor.nhs.uk/scieh/)
- 8.Seymour A, Black M, Oliver JS. Drug related deaths in the Strathclyde region of Scotland, 1995–1998. Forensic Sci Int 2001;122:52–9. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organisation. Hepatitis C: global prevalence. Wkly Epidemiol Rec 1997;46:341–4. [PubMed] [Google Scholar]
- 10.Surveillance of known hepatitis C antibody positive cases in Scotland: results to December 31, 1997. Scottish Centre for Infection and Environmental Health Weekly Report 1999;33:190–6. [Google Scholar]
- 11.Ramsey ME, Balogun MA, Collins M, et al. Laboratory surveillance of hepatitis virus infection in England and Wales: 1992 to 1996. Comm Dis Public Health 1998;1:89–94. [PubMed] [Google Scholar]
- 12.Lord Hunt, 2000. Hepatitis C. Parliamentary debates (Hansard). House of Lords Official Report: 1027–31.
- 13.EASL International Consensus Conference on Hepatitis C. J Hepatol 1999;30:956–61. [PubMed] [Google Scholar]
- 14.Ward C, Tudor-Williams G, Cotzias T, et al. Prevalence of hepatitis C among pregnant women attending an inner London obstetric department: uptake and acceptability of named antenatal testing. Gut 2000;47:277–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kendell RE. The beneficial consequences of the United Kingdom's declining per capita consumption of alcohol in 1979–82. Alcohol Alcohol 1984;19:271–6. [PubMed] [Google Scholar]
- 16.Schiff ER. The alcoholic patient with hepatitis C virus infection. Am J Med 1999;107:95s–9s. [DOI] [PubMed] [Google Scholar]
- 17.Harris DR, Gonin R, Alter HJ, et al. The relationship of acute transfusion-associated hepatitis to the development of cirrhosis in the presence of alcohol abuse. Ann Int Med 2001;134:120–4. [DOI] [PubMed] [Google Scholar]
- 18.Singh S, Miller R, Madge S, Patch D. The impact of hepatitis C in general practice. Br J Gen Pract 2000;50:532–6. [PMC free article] [PubMed] [Google Scholar]
- 19.Home Office. Home Office Statistical Bulletin. Issue 8/99. Drug seizure and offender statistics, United Kingdom, 1997. London: Home Office, 1997.
- 20.Judd A, Hickman M, Renton A, et al. Hepatitis C virus infection among injecting drug users: has harm reduction worked? Addiction Research 1999;7:1–6. [Google Scholar]
- 21.Williams I. Epidemiology of hepatitis C in the United States. Am J Med 1999;107:2s–9s. [DOI] [PubMed] [Google Scholar]
- 22.Alter MJ, Kruszon-Moran D, Nainan OV, et al. The prevalence of hepatitis C virus infection in the United States, 1988 through 1994. N Engl J Med 1999;341:556–62. [DOI] [PubMed] [Google Scholar]
- 23.Uchimura Y, Sata M, Kage M, et al. A histopathological study of alcoholics with chronic HCV infection: comparison with chronic hepatitis C and alcoholic liver disease. Liver 1995;15:300–6. [DOI] [PubMed] [Google Scholar]
- 24.Gossop M, Marsden J, Stewart D, et al. Patterns of drinking and drinking outcomes among drug misusers: 1-year follow-up results. J Subst Abuse Treat 2000;19:45–50. [DOI] [PubMed] [Google Scholar]
- 25.Lowinson J, Marion I, Joseph H, et al. Methadone maintenance. In: Lowinson J, Ruiz P, Millman R, et al, eds. Substance abuse: a comprehensive textbook, 2nd ed. Baltimore: Williams and Wilkins, 1992:560–1.
- 26.McCusker M. Influence of hepatitis C status on alcohol consumption in opiate users in treatment. Addiction 2001;96:1007–14. [DOI] [PubMed] [Google Scholar]
- 27.Best D, Noble A, Finch E, et al. Accuracy of perceptions of hepatitis B and C status: cross sectional investigation of opiate addicts in treatment. BMJ 1999;319:290–1. [DOI] [PMC free article] [PubMed] [Google Scholar]