Abstract
Dermatobia hominis causes furuncular myiasis and is endemic to South America. This report describes a case in a young woman who had recently visited Belize, highlighting the importance of clinical history (including travel history) and close liaison between pathologist and surgeon.
Keywords: Dermatobia hominis, furuncular myiasis
A 39 year old American woman was referred by her general practitioner to the day case surgery unit at St Mary’s Hospital, London for excision of a scalp “sebaceous cyst” that had been present for two months. This had been increasing in size, bleeding intermittently, and was associated with cervical lymphadenopathy. On examination a 3 cm firm, non-mobile cyst with central punctum was present.
On excision, movement was noted within the cyst cavity, and further dissection revealed the presence of a live larva, which crawled across the surgical trolley after removal. The cyst was removed in its entirety, and the wound debrided and cleaned with strict aseptic technique, with closure in the usual manner. Both theatre staff and patient were understandably alarmed by the nature of the cyst contents, and after the patient had been calmed, it was established that she had visited Belize four months previously, where she was bitten on the scalp.
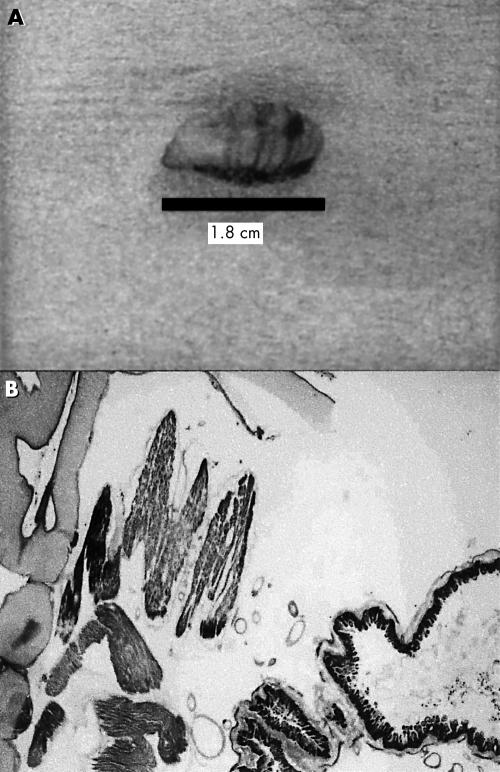
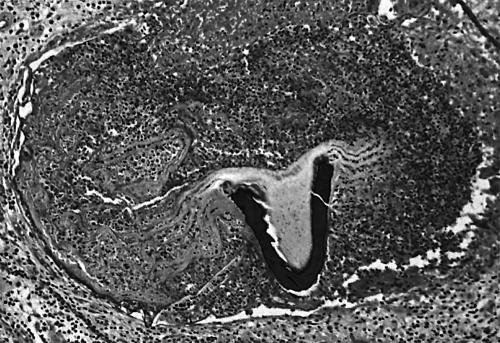
The histopathology department received two specimens: a skin ellipse with part of a cyst wall attached to the inferior surface, and a larva/maggot measuring 1.8 cm in length. The maggot was yellow, with multiple concentric black rings composed of spines around its outer surface (fig 1A). The larva possessed an outer cuticle, surrounding striated muscle and respiratory tubules (fig 1B). Histology of the skin showed a moderate chronic dermatitis, with an extensive abscess cavity present deep within the dermis, comprising multiple eosinophils, neutrophils, and multinucleate giant cells centred on part of the organism (fig 2). The macroscopic and microscopic features seen were consistent with those of Dermatobia hominis.
Figure 1.
(A) Macroscopic appearance of larva received. (B) Microscopic transverse section through larva showing respiratory tubules, striated muscle, and outer cuticle (haematoxylin and eosin stained).
Figure 2.
Intradermal abscess centred on organism (haematoxylin and eosin stained).
“On excision, movement was noted within the cyst cavity, and further dissection revealed the presence of a live larva, which crawled across the surgical trolley after removal”
Dermatobia hominis (also known as the botfly) is endemic to Central and South America and causes skin furuncular myiasis at the site of egg penetration. (Myiasis is defined as invasion of tissues by stages of Diptera flies.) Eggs are hatched on to a mosquito vector and injected into the human host as the mosquito feeds. After hatching the larvae rapidly burrow into the skin and develop for 50 to 60 days, when the adult larva drops to the ground and pupates. This mode of transmission is in contrast to that of the other fly genera, which involves direct contact with eggs and larvae.
Dermatobia hominis is characterised by rows of dark, backward pointing spines, and a pair of mouth hooks, with an external cuticle that encloses internal organs and striated muscle. It causes a papule with central punctum, through which the larva may occasionally be noted. Lesions are painful, with associated inflammation and regional adenitis. Because other genera produce similar clinical pathology it is best to preserve the larva and request formal identification by dissecting microscopy (either from the Hospital for Tropical Diseases or the Natural History Museum), rather than embed the specimen histologically.
Histopathology shows a cavity containing the larva extending from the epidermis to the mid/lower dermis. There are lymphocytes, neutrophils, and eosinophils around the larva and collagen degradation (secondary to larval enzymatic destruction). The cavity may be epithelialised, and rupture may be associated with a foreign body reaction. The only effective treatment is complete surgical excision.
A review of the literature revealed several reports of D hominis from Europe, Scandinavia, Australia, and the Americas, reflecting the widening experience of infectious disease as foreign travel increases. In a review of 13 cases in Munich, Germany, all cases of D hominis infection were related to travel to the Central American tropics.1 The most frequent differential diagnoses are infected sebaceous cyst, or a furuncle with associated lymphadenopathy. Almost all cases are present on limbs, although two papers detailed D hominis infection of the eye: both of which caused palpebral swelling,2,3 and one report described a woman with a long standing breast mass, excision biopsy of which revealed granulomatous inflammation centred around a fly larva.4
This case highlights the importance of the clinical history (including travel history), meticulous surgical technique to effect complete removal of the fly larva, and essential communication between surgeon and the pathologist to achieve prompt diagnosis.
Take home messages.
We report a case of Dermatobia hominis infection causing furuncular myiasis in a young woman who had recently visited Belize
This case highlights the importance of clinical history (including travel history) and close liaison between pathologist and surgeon
REFERENCES
- 1.Jelinek T, Nothdurft HD, Rieder N, et al. Cutaneous myiasis: review of 13 cases in travellers returning from tropical countries.Int J Dermatol 1995;34:624–6. [DOI] [PubMed] [Google Scholar]
- 2.Bangsgaard R, Holst B, Krogh E, et al. Palpebral myiasis in a Danish traveller caused by the human bot-fly (Dermatobia hominis).Acta Ophthalmol Scand 2000;78:487–9. [DOI] [PubMed] [Google Scholar]
- 3.Goodman RL, Montalvo MA, Reed JB, et al. Photo essay: anterior orbital myiasis caused by human bot-fly (Dermatobia hominis).Arch Ophthalmol 2000;118:1002–3. [PubMed] [Google Scholar]
- 4.Kahn DG. Myiasis secondary to Dermatobia hominis (human botfly) presenting as a long-standing breast mass.Arch Pathol Lab Med 1999;123:829–31. [DOI] [PubMed] [Google Scholar]