Abstract
Background: Chronic neutrophilic leukaemia (CNL) is a distinct BCR/ABL negative myeloproliferative disorder of elderly patients characterised by sustained neutrophilia and splenomegaly. The bone marrow shows expansion of neutrophilic granulopoiesis, without excess of myeloblasts. To date, only 129 cases of CNL have been reported in the literature.
Aims: To report the findings from a large group of 14 new cases of CNL, consisting of eight women and six men (mean age, 64.7 years).
Methods: A review of the 14 new cases of CNL and the investigation of BCR/ABL translocations in these patients.
Results: Three quarters of the patients died within two years after diagnosis, mostly as a result of severe cerebral haemorrhage. Two younger patients were successfully treated with allogeneic bone marrow transplantation or interferon, which resulted in haematological remission for years.
Conclusion: CNL is a rare myeloproliferative disease mostly taking a fatal clinical course, despite the presence of mature neutrophils as leukaemic cells in the blood. Thus, it is important to recognise CNL to develop appropriate therapeutic strategies for affected patients.
Keywords: chronic neutrophilic leukaemia, bone marrow, case reports, chronic neutrophilic leukaemia
Chronic neutrophilic leukaemia (CNL) is a rare BCR/ABL negative myeloproliferative disorder characterised by persistent neutrophilia and splenomegaly.1–3 CNL generally affects elderly patients of both sexes. Most patients with CNL have a poor prognosis, with a mean survival time of 21 months.4 To date, only 129 cases of CNL have been reported in the literature, including some cases in which the “leukaemic” state in fact represented a neutrophilic reaction, mostly as a result of plasma cell dyscrasia.1,2,5 The term “true” CNL recently introduced by Reilly5 highlights the need for more experience with further CNL cases to improve the diagnostic criteria. Therefore, we present our findings in a large group of 14 new cases of CNL, and discuss clinicopathological aspects of the disease.
REPORT OF THE CASES
In our institute, approximately 10 000 bone marrow biopsies are investigated every year, in many cases together with bone marrow and blood smears. Therefore, from the beginning of computed records in 1989, our archives have included probes of approximately 120 000 haematological patients. Among these records, we found 14 cases of CNL (comparative figure for chronic myeloid leukaemia (CML), 4597 cases). This “Freiburg collective” of patients with CNL consisted of eight women and six men, 10 of whom died (table 1). The mean age of the patients at diagnosis was 64.7 years (range, 37 to 81). The diagnosis of CNL was established on morphological findings and on clinical and laboratory data. All the patients showed chronic neutrophilia, and most of them had splenomegaly. Clinically, in all the cases an underlying leukaemoid reaction had been ruled out, and a myeloproliferative disorder (mostly: “CML?”) was suspected. Morphologically, the bone marrow was strongly hypercellular because of the expansion of neutrophilic granulopoiesis, which was only slightly left shifted and produced mature neutrophils. Both erythropoiesis and megakaryocytes were normocellular and without cytological abnormalities. The iron load of the phagocytic reticulum cells and the reticulin fibre network was normal. In the blood there was moderate leucocytosis (mean white blood cell count, 45.5 × 106/litre), including up to 95% mature neutrophils and band forms, but often also up to 20% myelocytes. In most of the cases the neutrophil alkaline phosphatase (NAP) score was greatly increased, and mild anaemia and thrombocytopenia were present. In no case was plasma cell dyscrasia found. On investigation of fresh blood samples of the patients taken at the time of diagnosis, no BCR/ABL translocation was detected using standard methods, including fluorescence in situ hybridisation. In the course of the disease, 10 of the patients died, with a mean survival time of 14.7 months. Cerebral haemorrhage (in six cases) was the most important cause of death. Two patients died of generalised leukaemic tissue infiltration, one of them showing ileus caused by a granulocytic and myelocytic infiltration of the small bowel. Another two patients died of pneumonia or after blastic transformation of the disease. Patient 1 is well and free of disease 73 months after familiary allogeneic bone marrow transplantation. The youngest patient (patient 9) has been in clinical remission during 41 months of interferon α treatment. The other patients were treated by blood transfusions when necessary or by hydroxyurea.
Table 1.
The Freiburg cases of chronic neutrophilic leukaemia, arranged in chronological order
| Patient | Sex | Age (years) | BCR/ABL-status | WBC (×109/l) | % N | Hb (g/l) | Plt. ×103 | F-Up (months) | SpM | NAP | Outcome |
| 1 | F | 40 | Negative | 22.6 | 84 | 129 | 106 | 73* | + | 298 | BMT, CR |
| 2 | M | 69 | Negative | 34.4 | 68 | 117 | 105 | 14† | (+) | NI | Chloroma |
| 3 | M | 69 | Negative | 11.3 | 72 | 79 | 117 | 9† | (+) | NI | Pneumonia |
| 4 | M | 69 | Negative | 49.2 | 88 | 90 | 84 | 19† | + | 2 | Cerebral haemorrhage |
| 5 | F | 77 | Negative | 89.0 | 95 | 102 | 135 | 15† | (+) | 91 | Chloroma |
| 6 | M | 64 | Negative | 41.7 | 84 | 109 | 281 | 9† | + | 55 | Cerebral haemorrhage |
| 7 | F | 77 | Negative | 93.0 | 74 | 77 | 116 | 8† | + | 293 | Cerebral haemorrhage |
| 8 | F | 81 | Negative | 35.0 | 95 | 108 | 189 | 38† | + | 270 | Cerebral haemorrhage |
| 9 | F | 37 | Negative | 36.2 | 92 | 143 | 273 | 41* | + | 383 | IFN-α |
| 10 | F | 72 | Negative | 38.0 | 90 | 89 | 47 | 23† | (+) | low | Blast crisis |
| 11 | M | 64 | Negative | 109.0 | 87 | 113 | 161 | 10† | + | 364 | Cerebral haemorrhage |
| 12 | F | 52 | Negative | 30.0 | 82 | 140 | 182 | 16* | (+) | 310 | No treatment |
| 13 | M | 72 | Negative | 22.8 | 88 | 93 | 62 | 2† | + | 40 | Cerebral haemorrhage |
| 14 | F | 63 | Negative | 24.6 | 78 | 123 | 210 | 5* | (+) | 46 | No treatment |
In patients 2–8, 10, 11 and 13 the outcome was fatal. Haematological data are those found at the time of diagnosis. *, indicates that the patient is alive and the number indicates the number of months since diagnosis; †, indicates that the patient is dead and the number indicates the number of months after diagnosis.
BMT, bone marrow transplantation; CR, complete remission; F-Up, follow up period; Hb, haemoglobin; IF-α, interferon α; %N, % of neutrophils; NAP, neutrophil alkaline phosphatase score (normal range, 20–120); NI, not investigated; Plt., platelet count; SpM, splenomegaly; WBC, leucocyte count; (+), mild form.
DISCUSSION
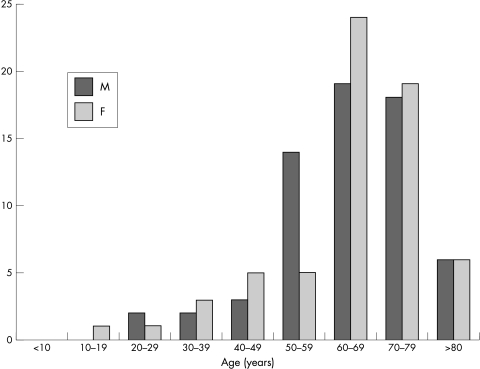
The main diagnostic criteria of CNL are chronic neutrophilia in the blood, expansion of neutrophilic granulopoiesis in the bone marrow, and splenomegaly in the absence of any form of BCR/ABL translocation or leukaemoid reaction.1 These criteria were sufficiently fulfilled in our 14 patients with CNL. The spectrum of fatal complications we saw in our patients was very similar to that described in the literature.2 The haemorrhagic diathesis seen in patients with CNL may be the result of thrombocytopenia and thrombocyte dysfunction,6 or it may be caused by leukaemic infiltration of vascular walls.7 With rare exceptions,8 CNL is a disease of older adults (fig 1). At the time of diagnosis, 88% of the patients with CNL in the literature were older than 50 years. The sex distribution in CNL is nearly equal.
Figure 1.
Distribution of patients with chronic neutrophilic leukaemia in the literature (including the Freiburg cases) according to sex and age.
There is doubt about whether all of the CNL cases in the literature represent true CNL. Some authors1,2,5 have suggested that those cases of CNL that occurred in association with plasma cell dyscrasias like myeloma were in fact neutrophilic reactions. Moreover, it was suggested that cases of CNL showing dysplastic features would be better classified as a myelodysplastic entity. Thus, reviewing the data of all CNL cases in the literature, Reilly5 defined a group of 33 cases of true CNL, including one unpublished case of his own. This group of 33 selected patients with CNL also showed a high mean age (62.5 years) and short survival times (mean survival, 30 months), but had a 2 : 1 male to female ratio. The term true CNL used by Reilly reveals the need for an even more precise definition of CNL as an entity. Thus, the diagnostic criteria of CNL should be applied in a strict manner, especially for the conditions mentioned above.
“To date, because of the rarity of the disease, no therapeutic standard has been determined in chronic neutrophilic leukaemia”
In the differential diagnosis of CNL, patients with CML usually show a higher degree of leucocytosis (white blood cell count, ∼ 170 × 106/litre), with more immature granulopoietic forms, a decreased NAP score, and basophilia.1 In the bone marrow, granulopoiesis is far more left shifted, and micromegakaryocytes are present. The most important criterion of CML is the presence of a BCR/ABL translocation. There is a rare form of CML (neutrophilic chronic myeloid leukaemia)9 that shares some of the morphological features of CNL, but is characterised by an uncommon type of BCR/ABL translocation (BCR e19/ABL a2). Like CNL, leukaemoid reactions are BCR/ABL negative and show identical morphological changes, including raised NAP scores, making a distinction difficult or even impossible. Because CNL is a clonal disorder,10 clonality studies of the neutrophils in the future may help to distinguish between cells of leukaemic or reactive origin.
To date, because of the rarity of the disease, no therapeutic standard has been determined in CNL.2 Chemotherapeutic agents, such as hydroxyurea, may temporarily control leucocytosis and splenomegaly, and the use of interferon α may induce long standing clinical remission.4 So far, allogeneic bone marrow transplantation represents the only treatment modality with curative potential.2,6
Take home messages.
Chronic neutrophilic leukaemia (CNL) is a rare myeloproliferative disease, mainly found in elderly patients
This disease has a mostly fatal outcome—three quarters of our patients died within two years of diagnosis, mainly as a result of severe cerebral haemorrhage
Two younger patients were successfully treated with allogeneic bone marrow transplantation or interferon, which resulted in haematological remission for years
Thus, it is important to recognise CNL and to develop appropriate therapeutic strategies for affected patients
We conclude that it is important to recognise CNL as a rare, but distinct, disease entity different from CML, and in particular to distinguish CNL from leukaemoid reactions, because patients with CNL generally have a poor prognosis. To gain a better understanding of the nature of true CNL the reporting of new cases must be encouraged.
Abbreviations
CML, chronic myeloid leukaemia
CNL, chronic neutrophilic leukaemia
NAP, neutrophil alkaline phosphatase
REFERENCES
- 1.Imbert M, Vardiman JW, Bain B, et al. Chronic myeloproliferative diseases. In: Jaffe ES, Harris NL, Stein H, Vardiman JW, eds. World Health Organisation classification of tumours. Pathology and genetics of tumours of haematopoietic and lymphoid tissues. Lyon: IARC Press, 2001:20–8.
- 2.Elliott MA, Dewald GW, Tefferi A, et al. Chronic neutrophilic leukemia (CNL): a clinical, pathologic and cytogenetic study. Leukemia 2001;15:35–40. [DOI] [PubMed] [Google Scholar]
- 3.You W, Weisbrot IM. Chronic neutrophilic leukemia. Report of two cases and review of the literature. Am J Clin Pathol 1979;72:233–42. [DOI] [PubMed] [Google Scholar]
- 4.Meyer S, Feremans W, Cantiniaux B, et al. Successful alpha-2b-interferon therapy for chronic neutrophilic leukaemia. Am J Hematol 1993;43:307–9. [DOI] [PubMed] [Google Scholar]
- 5.Reilly JT. Chronic neutrophilic leukaemia: a distinct clinical entity? Br J Haematol 2002;116:10–18. [DOI] [PubMed] [Google Scholar]
- 6.Hossfeld DK, Lokhorst HW, Garbrecht M. Neutrophilic leukemia accompanied by hemorrhagic diathesis: report of two cases. Blut 1987;54:109–13. [DOI] [PubMed] [Google Scholar]
- 7.Noguchi T, Ikeda K, Yamamoto K, et al. Severe bleeding tendency caused by leukemic infiltration and destruction of vascular walls in chronic neutrophilic leukemia. Int J Hematol 2001;74:437–41. [DOI] [PubMed] [Google Scholar]
- 8.Hasle H, Olesen G, Kerndrup G, et al. Chronic neutrophil leukaemia in adolescence and in young adulthood. Br J Haematol 1996;94:628–30. [DOI] [PubMed] [Google Scholar]
- 9.Pane F, Frigeri F, Sindona M, et al. Neutrophilic-chronic myeloid leukemia: a distinct disease with a specific molecular marker (BCR/ABL with C3/A2 junction). Blood 1996;88:2410–14. [PubMed] [Google Scholar]
- 10.Froberg MK, Brunning RD, Dorion P, et al. Demonstration of clonality in neutrophils using FISH in a case of chronic neutrophilic leukemia. Leukemia 1998;12:623–6. [DOI] [PubMed] [Google Scholar]