Abstract
This report describes a case of cytomegalovirus (CMV) infection of the nasopharynx. A 47 year old man presented with a nasopharyngeal mass of one month's duration. The patient had a history of pneumonia one month previously. Sinus computed tomography incidentally picked up a nasopharyngeal mass. The initial biopsy showed lymphoid hyperplasia. Repeated nasopharyngoscopy showed a prominent central nasopharyngeal mass without ulceration. Histology of the nasopharyngeal biopsy revealed several enlarged epithelial cells with characteristic CMV cytopathic changes. An immunohistochemical study, using a monoclonal IgG antibody against a CMV antigen, confirmed CMV infection. The patient's nasopharyngeal mass decreased in size gradually on follow up. To the best of our knowledge, this is the first reported case of CMV infection of the nasopharynx in the English literature. This disease entity should be considered in those patients presenting with nasopharyngeal mass, biopsy negative for malignancy, and no underlying immunosuppression or immunodeficiency.
Keywords: cytomegalovirus infection, nasopharynx, Epstein-Barr virus, nasophayngeal carcinoma
Cytomegalovirus (CMV) infection is frequent and severe in children and adults with congenital or acquired immunosuppression or immunodeficiency. Active infection can either be disseminated or localised, where the gastrointestinal tract, central nervous system, respiratory tract, and adrenals are the most commonly infected sites.1
Nasopharyngeal carcinoma (NPC) is common in southern China, Africa, and among Greenland Eskimos.2 The presence of a neck mass, nasal symptoms, and aural symptoms are the main presenting complaints.3 Clinical examination commonly shows a nasopharyngeal mass with or without ulceration.
Localised infection by CMV of the nasopharynx has not been reported. We report one such case presenting as a nasopharyngeal mass, clinically simulating NPC.
CASE REPORT
A 47 year old man presented to our otorhinolaryngology unit with a nasopharyngeal mass. He had a history of pneumonia with cough and nasal discharge four weeks previously. Two courses of antibiotics were given. Sinus computed tomography at that time showed right sided maxillary sinusitis. An incidental nasopharyngeal mass was detected. Epstein-Barr virus (EBV) serology showed mildly raised titres. A nasopharyngeal biopsy revealed lymphoid hyperplasia.
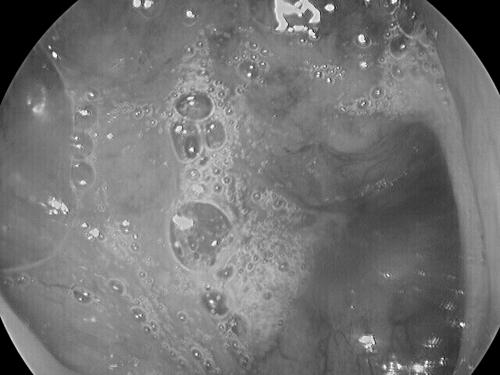
The patient continued to have nasal catarrh. Repeated direct nasopharyngoscopic examination in our unit revealed a prominent central nasopharyngeal mass with abundant secretions (fig 1). There was no ulceration. The EBV serology was rechecked. Immunofluorescence showed a mildly raised IgA antibody titre against EBV viral capsid antigen (VCA) (titre, 10), although the titre of IgA antibody against EBV early intracellular antigen (EA) was normal (titre < 5). Other blood tests, including a complete blood picture with differential white blood cell counts and erythrocyte sedimentation rate, were performed. All the results were within the normal range. The nasopharyngeal mass persisted in subsequent follow up two weeks later. NPC was suspected and thus a nasopharyngeal biopsy was taken.
Figure 1.
Direct nasopharyngoscopy view demonstrating the prominent nasopharyngeal mass with abundant secretion.
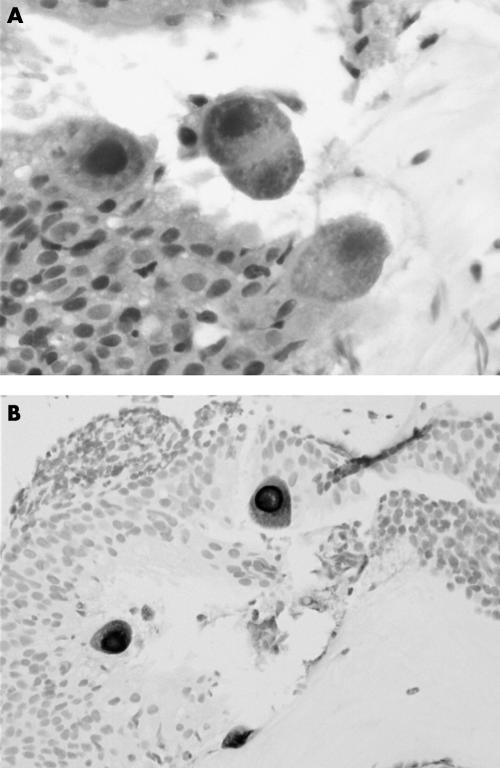
Histological examination of the nasopharyngeal biopsy revealed the features of CMV infection. Large epithelial cells, with both nuclear and cytoplasmic enlargements and characteristics basophilic intranuclear and intracytoplasmic inclusion bodies, were noted (fig 2A). The intracytoplasmic inclusion bodies were numerous and of varied size. Some larger inclusion bodies condensed near the cell membrane. The background showed lymphoid hyperplasia with no inflammation or ulceration. No malignancy was identified. Review of the previous nasopharyngeal biopsy showed lymphoid hyperplasia only. No CMV or other infection could be identified.
Figure 2.
(A) The nasopharyngeal biopsy demonstrating large epithelial cells with both nuclear and cytoplasmic enlargements and characteristic basophilic intranuclear and intracytoplasmic inclusion bodies (haematoxylin and eosin; original magnification, ×400). (B) Immunohistochemistry using a monoclonal antibody against cytomegalovirus antigen highlighting the enlarged epithelial cells (original magnification, ×200).
Immunohistochemical studies, using prediluted monoclonal mouse IgG antibody E-13 against an immediate early, non-structural 72 kDa antigen of CMV (Signet, Dedham, Massachusetts, USA), highlighted the enlarged epithelial cells (fig 2B). In situ hybridisation for EBV encoded RNAs (EBER), using a fluorescein conjugated oligonucleotide probe for EBER (Novocastra, Newcastle, UK), was negative.
The patient was then followed up and observed closely. No treatment was given. His nasal symptoms improved gradually. The nasopharyngeal mass decreased greatly in size on follow up. The IgA anti-EBV VCA titre decreased to 5.
DISCUSSION
The gastrointestinal tract, central nervous system, respiratory tract, adrenals, and rarely gall bladder and pancreas are common sites of CMV infection.1–4 To the best of our knowledge, localised nasopharyngeal CMV infection has never been reported. This is the first reported case of CMV infection of the nasopharynx in the English literature. In a study of 201 infants with respiratory tract infection, CMV was isolated in the nasopharyngeal aspirates from 10.9% of the patients. It was shown that CMV viral load was not related to clinical respiratory symptoms or nasopharyngeal mass. 5
The initial nasopharyngeal biopsy was negative for CMV infection. This might have been caused by the time lag between the two biopsies. Because the initial biopsy was taken at an early stage of the disease, the infected epithelial cells did not yet show the characteristic cytopathic changes. Nevertheless, sampling error is another possible explanation because only some of the epithelial cells in the current biopsy showed CMV cytopathic changes.
Our patient was immunocompetent, with no history of previous CMV infection. Therefore, this episode of CMV infection of the nasopharynx was probably a primary infection. Primary CMV infection in immunocompetent patients is usually latent and asymptomatic, but can be frequent and severe in children and adults with congenital or acquired deficient cellular immunity, underlying malignancy, and immunosuppression as a result of steroid administration or AIDS.1 In any patient with primary CMV infection, underlying immunodeficiency or immunocompromise should be always considered. Although this is the first reported case of CMV infection of the nasopharynx, this indicates the important role of CMV infection in the aetiology of nasopharyngeal masses, especially in immunocompetent patients. CMV infection should always be included in the benign causes of nasopharyngeal mass.
Take home messages.
This is the first reported case of cytomegalovirus infection of the nasopharynx
This disease entity should be considered in those patients presenting with nasopharyngeal mass, biopsy negative for malignancy, and no underlying immunosuppression or immunodeficiency
Nasopharyngeal carcinoma should be included in the list of differential diagnoses and investigated accordingly
“In any patient with primary cytomegalovirus infection, underlying immunodeficiency or immunocompromise should be always considered”
NPC should always be included in the list of differential diagnoses when nasopharyngeal mass is the presenting symptom in patients from endemic regions. NPC is common among the Chinese population, especially in southern China. In Hong Kong, it was the seventh most common cause of cancer mortality in 1999.6 One third of patients with NPC present with nasal symptoms as the main complaint, including postnasal dripping, nasal obstruction, and blood stained discharge. EBV is causally associated with NPC. EBV serology is a useful diagnostic tool, but the result should be interpreted with care. The two most useful and commonly used serological markers, IgA anti-EBV VCA and IgA anti-EBV EA, have different profiles of sensitivity and specificity.7
Many other conditions present as a nasopharyngeal mass. Adenoids are benign growths commonly found in children and adolescents. A large mass of adenoids is sometimes present in the adult patient. Occasionally, other diseases may present with a mass in the nasopharynx, such as tuberculosis, lymphoma, midline lethal granuloma, and sinonasal undifferentiated carcinoma. Nasopharyngeal angiofibroma is an uncommon, benign tumour found predominantly in adolescent boys, although it sometimes occurs in adults. Other extremely rare conditions, including primary nasopharyngeal amyloidosis, internal carotid artery aneurysm, sinonasal neuroendocrine tumour, giant pituitary adenoma, salivary gland tumour, fibrous tumour, giant cell tumour, rhabdomyosarcoma, and melanoma involving the nasopharynx, have been reported.8
In conclusion, we present the first case of nasopharyngeal CMV infection. This disease entity should be considered in those patients presenting with nasopharyngeal mass, biopsy negative for malignancy, and no underlying immunosuppression or immunodeficiency. NPC should be included in the list of differential diagnoses and investigated accordingly.
Abbreviations
CMV, cytomegalovirus
EA, Epstein-Barr virus early intracellular antigen
EBER, Epstein-Barr virus encoded RNA
EBV, Epstein-Barr virus
NPC, nasopharyngeal carcinoma
VCA, Epstein-Barr virus viral capsid antigen
REFERENCES
- 1.Hodinka RL, Friedman HM. Human cytomegalovirus. In: Murray PR, Baron EJ, Pfaller MA, et al, ed. Manual of clinical microbiology. Washington DC: AMS Press 1995:884–94.
- 2.Huang DP. Epidemiology of nasopharyngeal carcinoma. Ear Nose Throat J 1990;69:222–5. [PubMed] [Google Scholar]
- 3.S kinner DW, van Hasselt CA, Tsao SY. Nasopharyngeal carcinoma: a study of the modes of presentation. Ann Otol Rhinol Laryngol 1991;100:541–51. [DOI] [PubMed] [Google Scholar]
- 4.Bigio EH, Haure AK. Disseminated cytomegalovirus infection presenting with acalculous cholecystitis and acute pancreatitis. Arch Pathol Lab Med 1989;113:1287–9. [PubMed] [Google Scholar]
- 5.Wejse C, Birkebaek NH, Nielsen LP, et al. Respiratory tract infections in cytomegalovirus-excreting and nonexcreting infants. Pediatr Infect Dis J 2001;20:256–9. [DOI] [PubMed] [Google Scholar]
- 6.Hong Kong Hospital Authority. Hospital authority statistical report 1999/2000. Hong Kong: Hong Kong Hospital Authority.
- 7.Ho JHC, Lau WH, Kwan HC, et al. Epstein-Barr virus-specific IgA and IgG serum antibodies in nasopharyngeal carcinoma. Br J Cancer 1976;34:655–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Woo JKS. Clinical diagnosis. In: van Hasselt CA, Gibb AG, eds. Nasopharyngeal carcinoma. Hong Kong: the Chinese University Press 1999:111–26.