Abstract
Aim: To audit the benign surgical biopsies in women screened, assessed, and referred by the Leeds/Wakefield Breast Screening Unit for the year 1999–2000 with a view to determining any association with a preoperative B3 core biopsy categorisation.
Methods: The results of all preoperative diagnostic procedures in all patients who underwent surgical excision for a lesion proving benign in the year 1999–2000 were reviewed. Cases were categorised according to whether the preoperative fine needle aspirate cytology (FNAC) or core biopsy had been equivocal or of uncertain malignant potential (C3/B3), inadequate or unrepresentative (C1/B1), or benign (C2/B2). In those cases with a C3/B3 FNAC or core biopsy result, reasons for the uncertainty were determined by examination of the report and, where necessary, slides. In cases with C1/B1 or C2/B2 investigations and in those without a preoperative procedure, the reasons for surgical referral were determined from the screening records. Case records of all patients with a B3 core biopsy categorisation who subsequently proved to have malignancy were also reviewed.
Results: Thirty six women had benign surgical biopsies in the 1999–2000 screening year. In 13 of the 36 patients, referral for diagnostic biopsy rested on radiological and/or pathological suspicion of radial scar. The core biopsy category was B3 in all but one, which was in the B1 category. In a further 10 patients, referral was based primarily on a pathological B3 categorisation. The reasons for this were as follows: papillary lesion (two), fibroepithelial lesion (two), atypical intraductal epithelial proliferation (two), stromal mucin (two), atypical lobular hyperplasia (one), and an unusual vascular lesion (one). Two cases with a C3 on FNAC also derived from papillary lesions. In the remaining nine patients, the radiological features were sufficiently suspicious to prompt referral in the presence of either inadequate/unrepresentative (C1/B1) or benign (B2) preoperative pathological findings. Two women had no preoperative needle biopsy.
Conclusions: In 22 of 36 benign biopsies, the initial core biopsy categorisation was B3. According to the current system of core biopsy categorisation, a diversity of lesions must be designated as of “uncertain malignant potential” (B3) because the technique provides insufficient tissue for full histological assessment. The use of this category may increase the number of benign biopsies if all such cases are referred for surgery. An increase in the benign biopsy rate may be averted if larger amounts of tissue can be obtained using newer vacuum assisted techniques such as the Mammotome.
Keywords: benign biopsies, B3 category, breast screening, core biopsy
The non-operative diagnosis of breast cancer requires a multidisciplinary approach, and the assessment of screen detected mammographic abnormalities requires particularly close collaboration between radiologists and pathologists. In the early years after the introduction of the National Health Service Breast Screening Programme, pathological input related mainly to the interpretation of fine needle aspiration cytology (FNAC). More recently, there has been an increase in the use of core biopsy, although the extent to which each technique is used varies widely across the country. The increased use of core biopsy has been facilitated by the development of automatic spring loaded guns, and several publications have emphasised how the core biopsy technique can improve the non-operative diagnosis rate and more frequently achieve a definitive diagnosis—benign or malignant.1–3
“The number of core biopsies performed has increased progressively, and since 1999–2000 we have noticed an accompanying increase in the benign biopsy rate”
Recent guidelines for core biopsy interpretation indicate that the “B3” category should be used for lesions of “uncertain malignant potential”,3 although the wide range of lesions that potentially fall into this category is becoming increasingly recognised.2,3 For a screen detected abnormality it is difficult to recommend return to three yearly routine recall following such a categorisation and in many units, including our own, the usual management decision will be referral for diagnostic excision biopsy. The risk of unnecessary biopsies for benign disease in these circumstances will be determined by the criteria for inclusion in the B3 category.
Screening in our unit began in 1991 and the first screening round was completed in 1994. FNAC was used from the outset and although an occasional core biopsy was performed in 1994–5, the technique only became established in 1995–6. The number of core biopsies performed has increased progressively, and since 1999–2000 we have noticed an accompanying increase in the benign biopsy rate, particularly in prevalent screens. Two hundred and forty three FNACs and 92 core biopsies were performed in 1995–6 compared with 232 FNACs and 291 core biopsies in 1999–2000. The trend has continued, with a further decline in FNAC and a total of 332 cores performed in 2000–1. Over this period, the malignant to benign ratio has fluctuated but shown no significant trend up or down and was 4.6 : 1 in the 1999–2000 screening year. Sixteen (0.8/1000 screened) benign biopsies were performed in 1995–6, compared with 36 (1.3/1000 screened) in 1999–2000.
This audit was performed to clarify any relation between the increase in benign biopsies and the use of the B3 core biopsy category. The purpose of this report is to document our findings and to emphasise the diversity of benign lesions that may give rise to a B3 core. We also highlight the difficulties in deciding appropriate management for this group of women.
METHODS
Women who had been screened between 1 April 1999 and 31 March 2000 by the Leeds/Wakefield Breast Screening Service and who had undergone a surgical biopsy for a lesion that subsequently proved to be benign were identified from their screening records (KC62 instance report). The results of all preoperative investigations in these patients were reviewed. Cases were analysed according to whether the previous FNAC or core had been equivocal (B3/C3), unrepresentative (C1/B1), or benign (C2/B2). All needle biopsies (FNAC or core) were image guided. Stereotactic guidance was used only if the abnormality was not ultrasonically visible. A spring loaded automatic gun was used for the core biopsies. When using stereotactic guidance, 14 gauge cores were obtained, whereas 18 gauge cores were obtained when using ultrasound guidance. The number of cores taken was between two—for the assessment of a mass with ultrasound guidance—and five to eight—for the assessment of calcification using stereotactic guidance. All the patients being investigated for calcification were x rayed to assess whether representative areas of calcification had been sampled. In those patients with equivocal (B3/C3) core biopsy or FNAC results, reasons for the uncertainty were assessed by examination of the reports and, where necessary, slides. In those patients with inadequate (C1/B1) or benign (C2/B2) results and in patients without preoperative investigations, the reasons for surgical referral were determined from the screening records. Case records of all patients with equivocal (B3) core biopsy results who subsequently proved to have malignant disease were also reviewed.
RESULTS
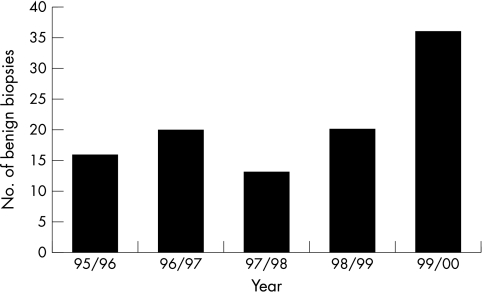
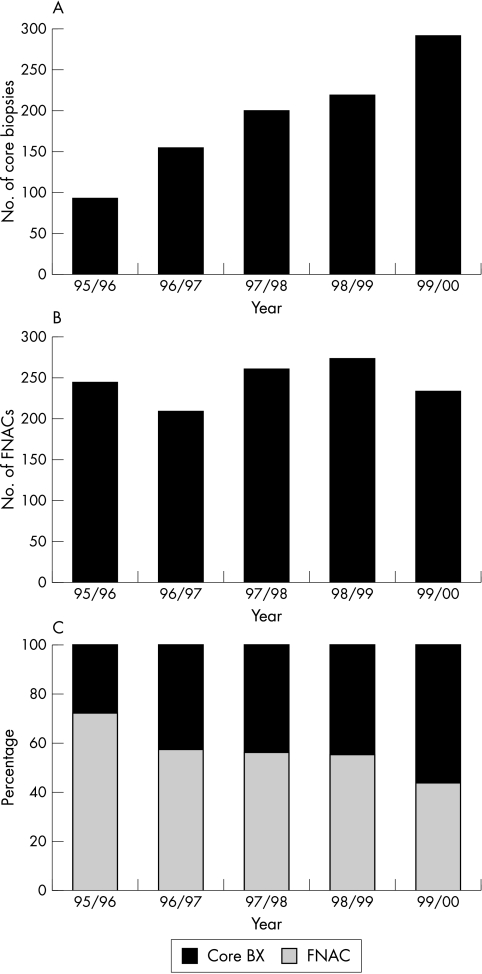
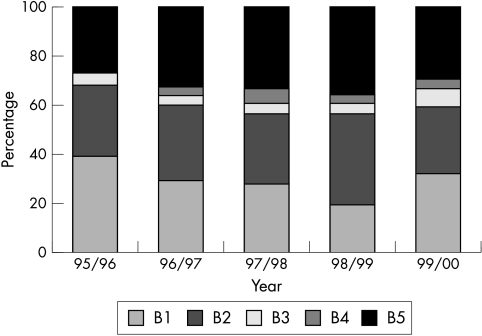
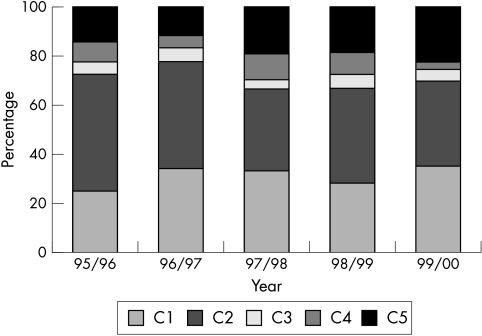
Thirty six women screened between 1 April 1999 and 31 March 2000 underwent surgical excision biopsy for a benign lesion. This was an increase from previous years (fig 1) and parallelled a significant increase in the number of core biopsies performed in the same period, with the number of core biopsies performed exceeding the number of FNACs performed for the first time (fig 2A–C). The year 1999–2000 also saw a relative increase in the proportion of core biopsies categorised as B3 (of uncertain malignant potential) with an accompanying increase in B1s (inadequate/unrepresentative) and a reduction in B2s and B5s (fig 3). With FNAC, a reduction in the proportion of aspirates categorised as C4 was associated with an increase in the proportion of C5s and a small reduction in C2s (fig 4).
Figure 1.
Numbers of benign biopsies performed from 1995–6 to 1999–2000.
Figure 2.
(A) Numbers of core biopsies performed from 1995–6 to 1999–2000. (B) Numbers of fine needle aspirate cytology (FNAC) procedures performed from 1995–6 to 1999–2000. (C) Relative percentages of core biopsies and FNACs from 1995–6 to 1999–2000.
Figure 3.
Relative percentage categorisation of core biopsies from 1995–6 to 1999–2000.
Figure 4.
Relative percentage categorisation of fine needle aspirate cytology samples from 1995–6 to 1999–2000.
Twenty two of the 36 patients referred for surgical excision had a B3 biopsy categorisation. In 12 patients the pathological features suggested radial scar. Ten patients had a B3 categorisation for reasons other than radial scar, with a diversity of lesions represented. One case suggested radial scar mammographically but only achieved a B1 categorisation preoperatively. Nine further patients had inadequate/unrepresentative or benign biopsy findings but suspicious changes on mammography. Two patients had a preoperative C3 on FNAC and two had neither FNAC nor core biopsy preoperatively.
Patients with equivocal histology or cytology (B3/C3)
Twenty two of the 36 patients with benign pathology at surgical excision had had an equivocal (B3) core biopsy result (tables 1, 2). In 12 (more than half) of these, the biopsy had suggested radial scar. In two the biopsy had suggested a papillary lesion. In two, the biopsy indicated fibroadenoma, but other more important pathology (phyllodes tumour in one case, radial scar in another) could not be excluded because of the limited amount of material available for assessment. In two, there was an intraductal epithelial proliferation difficult to classify and in two there were pools of stromal mucin requiring the exclusion of mucocele-like lesion or mucinous carcinoma. In one patient, the core contained atypical lobular hyperplasia and the possibility that this represented the edge of a more significant lesion could not be excluded. Mammographically, there was a discreet and persistent area of asymmetry, which was reported as radiologically indeterminate. The final case was a vascular lesion requiring exclusion of angiosarcoma.
Table 1.
Summary of reasons for B3 and C3 categorisation with final histological diagnosis
| Reasons | Final histology |
| B3 category (22) | |
| Suggestive of radial scar (12) | Radial scar (11) benign breast change (1) |
| Papillary lesion (2) | Papilloma (2) |
| Fibroepithelial lesion (2) | Fibroadenoma (2) |
| Intraductal epithelial proliferation (2) | Benign breast change (2 with 1 including pseudoangiomatous hyperplasia) |
| Stromal mucin (2) | Benign breast change (2) |
| Atypical lobular hyperplasia (ALH) (1) | ALH in benign breast change (1) |
| Vascular lesion (1) | Haemangioma (1) |
| C3 category (2) | |
| Focal dyscohesion and pleomorphism (2) | Intraduct papilloma (2), one with atypical ductal hyperplasia |
Table 2.
Final diagnoses in 22 patients with equivocal (B3/C3) histology or cytology and subsequent benign pathology, together with radiological findings
| Reason for B3 categorisation | Radiology | Final diagnosis |
| Suggestive of radial scar | Stromal deformity (RS) | Radial scar |
| Suggestive of radial scar | Stromal deformity (RU) | Radial scar |
| Suggestive of radial scar | Asymmetry and stromal deformity (RU) | Radial scar |
| Suggestive of radial scar | Asymmetry + stromal deformity + Ca2+ (RS) | Benign breast change |
| Suggestive of radial scar | Stromal deformity (RU) | Radial scar |
| Suggestive of radial scar | Stromal deformity + Ca2+ (RS) | Radial scar |
| Suggestive of radial scar | Stromal deformity (RS) | Radial scar |
| Suggestive of radial scar | Stromal deformity (RU) | Radial scar |
| Suggestive of radial scar | Stromal deformity (RU) | Radial scar |
| Suggestive of radial scar | Asymmetry + stromal deformity (RS) | Radial scar |
| Suggestive of radial scar | Stromal deformity (RS) | Radial scar |
| Suggestive of radial scar | Mass (RM) | Radial scar |
| Papillary lesion | Mass; 13 mm complex cyst on US (RB) | Papilloma |
| Papillary lesion | 20 mm mass (RS) | Papilloma |
| Fibroepithelial lesion | 16 mm new mass (RU) | Fibroadenoma |
| Fibroepithelial lesion | Asymmetry; 13 mm mass on US (RU) | Fibroadenoma |
| Intraductal epithelial proliferation (nature uncertain) | Asymmetry + Ca2+ (RU) | Benign breast change |
| Intraductal epithelial proliferation (nature uncertain) | Asymmetry (RU) | Benign breast change |
| Stromal mucin | Ca2+ (RU) | Benign breast change |
| Stromal mucin | Ca2+ (RU) | Benign breast change |
| Atypical lobular hyperplasia | Asymmetry (RU) | Benign breast change |
| Vascular lesion | 9 mm new mass (RB) | Haemangioma |
RB, radiologically benign; RS, radiologically suspicious; RU, radiologically indeterminate; US, ultrasound.
Only two patients had had an equivocal (C3) FNAC. In both, the final diagnosis was of an intraduct papilloma, although one of these contained a focus of atypical ductal hyperplasia (ADH). Both FNACs showed loss of cohesion and some cellular pleomorphism precluding a fully benign diagnosis.
Patients with inadequate/unrepresentative or benign histology or cytology (B1/B2 or C1/C2, respectively)
In 10 patients referred for excision, the initial biopsy or cytology findings were considered inadequate or insufficient (C1/B1) or benign (B2) (table 3). The radiological appearances in these patients were of sufficient concern to prompt referral for excision. There were three core biopsies reported as B1; two contained only a little normal breast tissue and were considered unrepresentative of the lesion (final histology revealing a fibroadenoma and radial scar in each case) and one did not contain the calcification that had been targeted. Three inadequate (C1) FNACs all contained blood stained fluid only; two derived from mixed solid cystic lesions, which subsequently proved to be intraduct papillomas, and one was from a postoperative haematoma, which had given rise to suspicious imaging appearances. In four patients a core biopsy had been reported as benign (B2). In three of these the core biopsy had suggested fibroadenoma but the problems of limited sampling and the difficulty of excluding phyllodes tumour in such cases had been discussed in the report. All three measured more than 2 cm in diameter and had increased in size since their previous screen. Two were confirmed as fibroadenomas and the other a benign phyllodes tumour on excision. The remaining B2 core contained part of a cyst wall but the radiological appearances were suspicious and the final histology revealed duct ectasia with a prominent associated granulomatous reaction. There were no patients with a previous benign (C2) FNAC.
Table 3.
Final diagnoses in 10 patients with previous inadequate/unrepresentative (B1/C1) or benign (B2/C2) histology or cytology and subsequent benign pathology
| CB/FNAC | Radiology | Final diagnosis | |
| B1 Insufficient | RS | Stromal deformity | Radial scar |
| B1 No calcification | RU | Calcification | Benign breast change |
| B1 Normal breast tissue | RB | Mass | Fibroadenoma |
| C1 Cyst fluid | RU | Complex cyst | Papilloma |
| C1 Bloody fluid | RU | Complex cyst | Papilloma |
| C1 Blood | RS | Stromal deformity | Haematoma |
| B2 Fibroadenoma | RU | Mass (↑ing in size) | Fibroadenoma |
| B2 Fibroadenomatoid change | RU | Mass (↑ing in size) | Phyllodes |
| B2 Cyst wall | RS | Asymmetry | Duct ectasia |
| B2 Fibroadenoma | RU | Mass (↑ing in size) | Fibroadenoma |
| NA Warfarin | RU | Calcification | Benign breast change and fibroadenoma |
| NA Patient declined | RU | Mass | Fibroadenoma |
CB, core biopsy; FNAC, fine needle aspiration cytology; NA, not available; RB, radiologically benign; RS, radiologically suspicious; RU, radiologically indeterminate.
Patients with B3 core biopsy and subsequent malignant histology
During the same year, four patients with an equivocal (B3) core biopsy were subsequently found to have malignancy after surgical excision (table 4).
Table 4.
Final diagnoses in four patients with equivocal (B3) histology and subsequent malignant pathology
| Reasons for B3 category | Final diagnosis |
| Atypical intraductal epithelial proliferation (×2) | (1) Widespread ADH/low grade micropapillary DCIS |
| (2) ADH/DCIS with multifocal invasive carcinoma | |
| Suggestive of radial scar | Radial scar with DCIS |
| Atypical epithelium with granulomatous inflammation | 6 mm invasive ductal carcinoma, grade 3 |
ADH, atypical ductal hyperplasia; DCIS, ductal carcinoma in situ.
In two patients the core biopsies contained an intraductal epithelial proliferation, which was difficult to classify, but of sufficient concern to warrant referral for surgery. One patient with widespread microcalcification was subsequently found to have widespread ADH merging with low grade micropapillary ductal carcinoma in situ (DCIS) and required mastectomy. The other was found to have a multifocal invasive carcinoma (mixed tubular and lobular), in addition to low grade DCIS, and also required mastectomy. One patient had a core biopsy suggesting radial scar and this was found to be associated with DCIS after excision. The remaining patient had a core biopsy containing an intense granulomatous reaction associated with atypical epithelium, which was difficult to assess, and this subsequently proved to derive from an adjacent 6 mm invasive ductal carcinoma of no special type, grade III.
DISCUSSION
Here, we present an audit of the benign surgical biopsies performed on patients screened by the Leeds/Wakefield Breast Screening Unit during the year April 1999 to March 2000. The numbers of benign biopsies performed in this year increased in parallel with an increase in the number of core biopsies performed. In approximately one third of cases, referral rested on radiological suspicion, together with inadequate or unrepresentative core biopsies/FNAC findings. In another third, the radiological and core biopsy findings suggested radial scar (B3), and our current policy (in keeping with national recommendations) is to remove these lesions. In the remaining third, referral for surgery hinged on equivocal core biopsy (B3) or FNAC (C3) findings in which it was difficult to exclude more serious pathology.
“The potential disadvantage of an increase in benign biopsies should be weighed carefully against the reduced need for diagnostic surgical excision and a two stage operative procedure for patients with malignancy”
The core biopsies were classified according to national guidelines3 and the proportion classified as B3 increased from the 1998–9 to the 1999–2000 screening year. This increase was accompanied by an increase in the proportion of B1s and a relative reduction in the proportion of B2s. One purported advantage of core biopsy over FNAC is increased specificity, with the potential for a better characterised benign diagnosis.1 As increasing numbers of lesions are targeted, it is likely that the detailed information available from histological analysis will start to reveal more areas of uncertainty. It is difficult in these cases to exclude more serious pathology without complete excision, and this is perhaps the price that must be paid for a high non-operative diagnosis rate (now over 90% in our unit). However, the potential disadvantage of an increase in benign biopsies should be weighed carefully against the reduced need for diagnostic surgical excision and a two stage operative procedure for patients with malignancy.
The single most common reason for a B3 categorisation was the possibility of radial scar formation. The remaining cases were a heterogeneous mix of conditions, all of which have been highlighted previously as areas of recognised difficulty.2 We agree with Ibraham and colleagues4 that these essentially fall into two categories with a lesser and greater risk of associated malignancy. They suggest subdividing the category into B3a for benign lesions potentially associated with malignancy (for example radial scars and intraduct papillomas) and B3b for more worrisome atypical epithelial proliferations. The difficulties in assessing epithelial proliferation in limited amounts of material are emphasised here by those cases subsequently proving benign, but it is of note that three out of the four patients with a B3 core biopsy categorisation that subsequently proved malignant also presented with a diagnostically difficult intraepithelial proliferation. Others have reported a risk of malignancy varying from 18% to 83% when the core biopsy contains an atypical epithelial proliferation amounting to ADH at least,5–8 and prompt referral for excision is warranted in these circumstances.
We believe that the decision whether or not to excise papillary and fibroepithelial lesions should be considered on an individual case basis. At present, there are insufficient data to determine the risks of not removing lesions with a core biopsy diagnosis of intraductal papilloma, although the recent guidelines for non-operative assessment allow some papillary lesions to be classified as B2 if they are small and incidental.3 This may be safe if the radiological and clinical findings are also benign.9,10 Most follow up studies suggest that these lesions have a low precancerous potential, although heterogeneity is a concern, particularly if the lesions are large, multiple, or diffuse. Fibroepithelial lesions are a perennial problem and neither core biopsy nor FNAC can reliably distinguish fibroadenoma from phyllodes tumour. We adopt a pragmatic approach, taking into account the patient’s age, imaging findings, and the size of the lesion (and any recent increase), in addition to an assessment of the histological features of increased cellularity and mitotic activity. However, we recognise that this approach runs a small risk of leaving some phyllodes tumours in the breast.
“Our audit of benign biopsies for the year 1999–2000 has highlighted the challenges of core biopsy diagnosis when limited sampling fails to provide certainty of diagnosis”
Other lesions, such as vascular lesions, stromal mucin, and lobular neoplasia, occur less frequently and may have to be considered individually until the associated risks become clearer. The most appropriate management of patients with lobular neoplasia diagnosed on core biopsy is controversial, although a recent report of screen detected lobular carcinoma in situ (LCIS) in Cambridge reported associated DCIS or invasive malignancy in three of seven cases.11 The analysis of large series from the USA suggests that lesions associated with calcification or a mass radiologically may be potentially of more importance,12 and that excision is particularly important if there is an associated risk lesion, such as radial scar or ADH.13 Excision is also warranted if the lesion shares features with DCIS. The well recognised difficulties of defining where on the spectrum atypical lobular hyperplasia becomes LCIS and in distinguishing LCIS from low grade DCIS are exacerbated in core biopsy material. The challenge presented by stromal mucin pools in a biopsy are fortunately rare, but as with the presence of mucin in an FNAC,14,15 excision may be necessary to exclude mucinous carcinoma or mucocele-like tumour.
Take home messages.
In our audit of benign biopsies for the year 1999–2000, the initial core biopsy categorisation was B3 in 22 of 36 benign biopsies
The current system of core biopsy categorisation results in a diversity of lesions being designated as of “uncertain malignant potential” (B3) because the technique provides insufficient tissue for full histological assessment
The use of this category may increase the number of benign biopsies if all such cases are referred for surgery
Newer vacuum assisted techniques, such as the Mammotome, provide larger amounts of tissue and may help reduce this increase in the benign biopsy rate
In summary, our audit of benign biopsies for the year 1999–2000 has highlighted the challenges of core biopsy diagnosis when limited sampling fails to provide certainty of diagnosis. This report highlights areas of diagnosis where a specific benign diagnosis is difficult to achieve with confidence. Difficulties in histological diagnosis stem largely from the limited amount of material available in a core and uncertainties over whether this is representative. Newer vacuum assisted techniques, such as the Mammotome,16 which remove larger amounts of tissue, will probably prove helpful in this area, avoiding the need for open biopsy in some patients.
Acknowledgments
We would like to acknowledge the careful typing of P Cudmore and to thank Professor A Hanby for his helpful comments on the manuscript.
Abbreviations
ADH, atypical ductal hyperplasia
DCIS, ductal carcinoma in situ
FNAC, fine needle aspirate cytology
LCIS, lobular carcinoma in situ
REFERENCES
- 1.Britton PD, McCann J. Needle biopsy in the NHS Breast Screening Programme 1996/97: how much and how accurate? The Breast 1999;8:5–11. [Google Scholar]
- 2.Humphreys S. Appropriate use and evaluation of the needle core biopsy in breast disease. CPD Bulletin Cellular Pathology 2000;2:57–108. [Google Scholar]
- 3.Guidelines for non-operative diagnostic procedures and reporting in breast cancer screening, NHSBSP Publication No 50. Sheffield: NHS Cancer Screening Programmes, June 2001.
- 4.Ibrahim AEK, Bateman AC, Theaker JM, et al. The role and histological classification of needle core biopsy in comparison with fine needle aspiration cytology in the pre-operative assessment of impalpable breast lesions. J Clin Pathol 2001;54:121–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jackman RJ, Nowels KN, Shepard MJ, et al. Stereotaxic large-core needle biopsy of 450 non-palpable breast lesions with surgical correlation in lesions with cancer or atypical hyperplasia. Radiology 1994;193:91–5. [DOI] [PubMed] [Google Scholar]
- 6.Liberman L, Cohen MA, Dershaw DD, et al. Atypical hyperplasia diagnosed at stereotaxic core biopsy of breast lesions: an indication for surgical biopsy. AJR Am J Roentgenol 1995;164:1111–13. [DOI] [PubMed] [Google Scholar]
- 7.Darling ML, Smith DN, Lester SC, et al. Atypical ductal hyperplasia and ductal carcinoma in situ as revealed by large-core needle breast biopsy: results of surgical excision. Am J Roetgenol 2000;175:1341–6. [DOI] [PubMed] [Google Scholar]
- 8.Brown TA, Wall JN, Christensen ED, et al. Atypical hyperplasia in the era of stereotactic core needle biopsy. J Surg Oncol 1998;67:168–73. [DOI] [PubMed] [Google Scholar]
- 9.Philpotts LE, Shaheen NA, Jain KS, et al. Uncommon high-risk lesions of the breast diagnosed at stereotactic core-needle biopsy: clinical importance. Radiology 2000;216:831–7. [DOI] [PubMed] [Google Scholar]
- 10.LibermanL, Bracero N, Vuolo MA, et al. Percutaneous large-core biopsy of papillary breast lesions. Am J Roentgenol 1999;172:331–7. [DOI] [PubMed] [Google Scholar]
- 11.O’Driscoll D, Britton P, Bobrow L, et al. Lobular carcinoma in situ on core biopsy—what is the clinical significance? Clin Radiol 2001;56:216–20. [DOI] [PubMed] [Google Scholar]
- 12.Ber WA, Mrose HE, Loffe OB. Atypical lobular hyperplasia or lobular carcinoma in situ at core-needle breast biopsy. Radiology 2001;218:503–9. [DOI] [PubMed] [Google Scholar]
- 13.Liberman L, Sama M, Susnik B, et al. Lobular carcinoma in situ at percutaneous breast biopsy: surgical biopsy findings. Am J Roentgenol 1999;173:291–9. [DOI] [PubMed] [Google Scholar]
- 14.Wong NL, Wan SK. Comparative cytology of mucocele-like lesion and mucinous carcinoma of the breast in fine needle aspiration. Acta Cytol 2000;44:765–70. [DOI] [PubMed] [Google Scholar]
- 15.Kim Y, Talatsuka Y, Morinao H. Mucocele-like tumour of the breast: a case report and assessment of aspirated cytological specimens. Breast Cancer 1998;5:317–20. [DOI] [PubMed] [Google Scholar]
- 16.Velanovitch V, Lewis FR, Nathansom SD, et al. Comparison of mammographically guided breast biopsy techniques. Ann Surg 1999;229:625–33. [DOI] [PMC free article] [PubMed] [Google Scholar]