Abstract
Aims: The Mirena coil is a levonorgestrel releasing intrauterine device that is in widespread use. This study aims to document the endometrial morphology associated with this device.
Methods: Endometrial specimens from 75 women with the Mirena coil were reviewed and the histological features detailed.
Results: Morphological features found in most of the endometria were decidualisation of stroma (72 of 75 cases), atrophy of endometrial glands (65 of 75 cases), a surface papillary pattern (38 of 75 cases), and a stromal inflammatory cell infiltrate (59 of 75 cases). Additional common histological features were the presence of foci of stromal myxoid change (29 of 75 cases) and stromal haemosiderin pigment (24 of 75 cases). Reactive atypia of surface glands, glandular metaplastic changes, stromal necrosis, and stromal calcifications were found in small numbers of cases.
Conclusion: The endometrial features are characteristic and relatively constant and are in keeping with the effects of both a progestogenic compound and a mechanical device. Pathologists should be aware of these histological features because the Mirena coil is in widespread use.
Keywords: endometrium, Mirena coil, levonorgestrel releasing intrauterine device
The Mirena coil is a levonorgestrel releasing intrauterine device that is in widespread use in the UK and elsewhere. It is a progestogen containing device and is currently licensed for periods of treatment of five years.1
“Given the expansion in the clinical indications for Mirena coil usage we have reviewed the endometrial morphology in a large series of patients treated with this device”
The Mirena coil is a highly effective contraceptive and, compared with other intrauterine devices, reduces menstrual bleeding.2 The Mirena coil is also licensed for the management of idiopathic menorrhagia.3 Previous studies have shown the Mirena coil to compare well with endometrial resection for the management of menorrhagia.4 The system has also been used to deliver progestogen for endometrial protection in postmenopausal hormone replacement regimens.5 It has also been suggested that the Mirena coil can be used to prevent endometrial hyperplastic changes in patients taking tamoxifen or oestrogen only hormone replacement therapy.6
Despite its widespread use, our impression is that the effects of the Mirena coil on endometrial morphology are not well known, especially among general pathologists. These morphological features have been briefly alluded to previously.7,8 However, given the expansion in the clinical indications for Mirena coil usage we have reviewed the endometrial morphology in a large series of patients treated with this device.
MATERIALS AND METHODS
Patients (n = 75) were retrieved from the files of the departments of pathology, Royal Group of Hospitals Trust, Belfast, and John Radcliffe Hospital, Oxford. All available histological sections were reviewed by the authors, two of whom (SM, WGM) are gynaecological pathologists. The duration of coil placement was not known in these patients.
RESULTS
Clinical findings
The age of the patients ranged between 25 and 58 years, with a mean of 42. Eighteen patients underwent hysterectomy, one had a transcervical resection of the endometrium, and in 56 patients there was an endometrial curettage or pipelle biopsy.
Usually the indication for hysterectomy or endometrial sampling was irregular vaginal bleeding. Four patients had a history of endometrial hyperplasia (three simple hyperplasia and one atypical hyperplasia) diagnosed on previous endometrial sampling. In these cases, the Mirena coil had been inserted after the diagnosis of endometrial hyperplasia.
Pathological findings
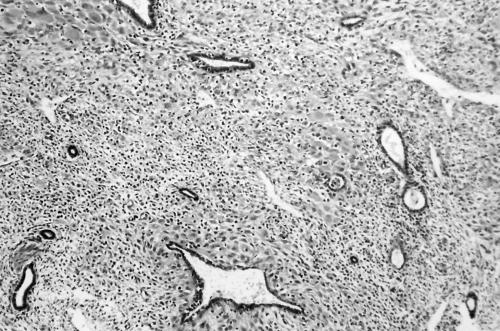
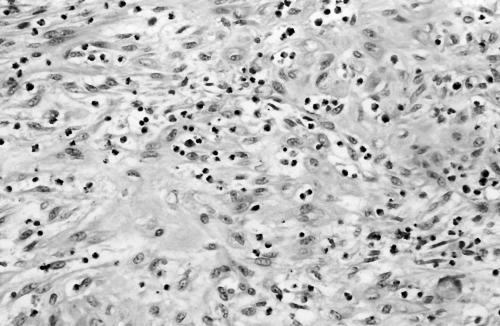
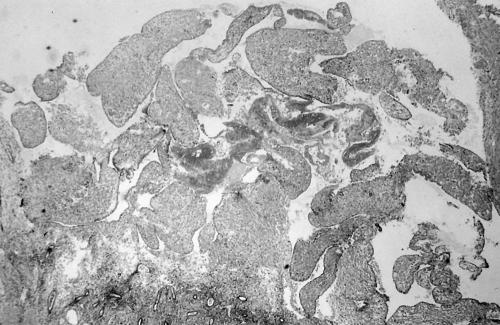
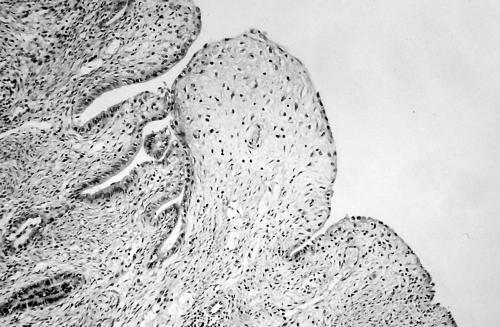
Table 1 shows the morphological features of the endometria. In 72 of 75 cases there was decidualisation of the stroma (fig 1), 65 of 75 samples contained atrophic small tubular endometrial glands (in occasional cases there was focal weak secretory activity of some glands), and in 59 of 75 samples there was a stromal inflammatory cell infiltrate, usually with a mixture of lymphocytes, neutrophils, histiocytes, and eosinophils (fig 2). In 20 of these cases, plasma cells were identified. The stromal decidualisation and glandular atrophy generally involved the whole of the superficial endometrium but not the endometrial basalis. The surface had a localised undulating papillary pattern (fig 3) in 38 of 75 cases (best seen in hysterectomy specimens where the endometrium was present in its entirety). Foci of stromal myxoid change were present in 29 of 75 cases (fig 4). Twenty four of 75 cases contained small amounts of haemosiderin pigment within the stroma, in two cases there was stromal necrosis, and in one case there were stromal calcifications. In three cases there was significant reactive atypia of the surface endometrial glands and in seven cases focal glandular metaplastic changes (hobnail, clear cell, or ciliated) were present. Stromal granulomas were not seen.
Table 1.
Endometrial morphological features associated with Mirena coil
| Morphological feature | Number of cases |
| Decidualisation of stroma | 72 (96%) |
| Atrophy of glands | 65 (87%) |
| Stromal inflammatory cell infiltrate | 59 (79%) |
| Stromal inflammatory cell infiltrate, including plasma cells | 20 (27%) |
| Surface papillary formations | 38 (51%) |
| Stromal myxoid change | 29 (39%) |
| Stromal haemosiderin deposition | 24 (32%) |
| Glandular metaplasia | 7 (9%) |
| Stromal necrosis | 5 (7%) |
| Reactive atypia in surface glands | 3 (4%) |
| Stromal calcifications | 1 (1%) |
Figure 1.
Atrophic endometrial glands are present in a decidualised stroma.
Figure 2.
There is a mixed stromal inflammatory cell infiltrate.
Figure 3.
The surface of the endometrium has a papillary appearance.
Figure 4.
Area of stromal myxoid change.
Of the four patients with a history of endometrial hyperplasia, the three with simple hyperplasia showed no evidence of persisting hyperplasia and the other showed a small focus of persisting atypical hyperplasia.
Coexisting pathology in the hysterectomy specimens included leiomyomas in eight cases and adenomyosis in one. There was one case of cervical intraepithelial neoplasia (CIN) I and one of CIN III. In one case there was cervical microglandular hyperplasia (MGH) associated with focal decidualisation of the cervical stroma.
DISCUSSION
The aim of this report is to describe the histological appearances of endometria associated with the Mirena coil. This device is in common usage and pathologists should be aware of the associated morphological features. These have not been described extensively in the literature and it is our impression that many general pathologists reporting gynaecological specimens are not aware of them.
The glandular atrophy and stromal decidualisation, which were found in most cases, are exactly those expected with a progestogen containing device. The endometrial basalis, as expected, did not show these features because this layer is not hormone responsive. In one case, there was cervical MGH and stromal decidualisation, suggesting that the progestogenic effects may extend beyond the body of the uterus. Other features such as the surface undulations, the inflammatory cell infiltrate, and the stromal haemosiderin deposition can be attributed directly to the local effects of an intrauterine device. The presence of stromal plasma cells in many cases is indicative of an endometritis, these generally being considered necessary for a definitive diagnosis of endometritis because lymphocytes and neutrophils may be a normal component of the endometrium depending on the stage of the menstrual cycle. It may be that, in those cases with stromal plasma cells, this is indicative of a superimposed infectious process. One of the previously referred to studies detailing the morphological features of endometria associated with Mirena coil usage found a prominent infiltrate of CD56 positive large granular lymphocytes.7 We did not perform CD56 staining in our study. Stromal myxoid change was found in 39% of cases. This is analogous to the myxoid change that can occasionally occur in normal endometrial stroma and in the stromal component of endometriosis, especially when associated with decidual stromal change.9–11 Reactive atypia of surface endometrial glands secondary to the intrauterine device was not a prominent feature, with pronounced atypia only being found in three cases. A variety of epithelial metaplastic changes were found in seven cases. These were usually focal in distribution. Stromal granulomas were not identified.
“The glandular atrophy and stromal decidualisation, which were found in most cases, are exactly those expected with a progestogen containing device”
Take home messages.
The endometrial features associated with the use of the levonorgestrel releasing Mirena coil are characteristic and relatively constant
These features are in keeping with the effects of both a progestogenic compound (for example, glandular atrophy and stromal decidualisation) and a mechanical device (for example, surface undulations, inflammatory cell infiltrate, and stromal haemosiderin deposition)
Pathologists should be aware of these histological features because the Mirena coil is in widespread use
Only one previous study has described in detail the endometrial morphology associated with levonorgestrel releasing intrauterine devices.8 The morphological features noted in that study were broadly similar to those we describe. In the previous study, foci of stromal calcification were present in a small proportion of cases where the intrauterine device had been in situ for three years or more. In our study, as already stated, stromal calcifications were only present in a single case and we have no information regarding the duration of treatment with the Mirena coil.
Of the four patients with a history of endometrial hyperplasia, persisting hyperplasia was only identified in subsequent endometrial sampling in one patient. This was the case with atypical hyperplasia. It is, of course, well recognised that progestogenic agents may result in reversal of endometrial hyperplasia and even well differentiated endometrioid adenocarcinomas.12–15 Indeed, recently intrauterine progesterone containing devices have been used, with some success, for the treatment of low grade, early stage endometrioid adenocarcinomas in women who are a poor operative risk.16
In conclusion, our study describes the endometrial morphological features associated with the Mirena coil, a progestogen containing device. Pathologists should be aware of these features because this device is increasingly being used as a contraceptive and for the management of abnormal uterine bleeding.
Abbreviations
CIN, cervical intraepithelial neoplasia
MGH, microglandular hyperplasia
REFERENCES
- 1.Mansour D, Guillebaud J. Data support extended use of levonorgestrel intrauterine systems. BMJ 1998;316:1671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nilsson CG. Comparative quantitation of menstrual blood with a d-norgestrel-releasing IUD and a Nova T-copper device. Contraception 1977;15:379–87. [DOI] [PubMed] [Google Scholar]
- 3.Levonorgestrel intrauterine system for menorrhagia. Drug Ther Bull 2001;39:85–7. [DOI] [PubMed] [Google Scholar]
- 4.Istre O, Trolle B. Treatment of menorrhagia with the levonorgestrel intrauterine system versus endometrial resection. Fertil Steril 2001;76:304–9. [DOI] [PubMed] [Google Scholar]
- 5.Suvanto-Luukkonen E, Kauppila A. The levonorgestrel intrauterine system in menopausal hormone replacement therapy: five year experience. Fertil Steril 1999;72:161–3. [DOI] [PubMed] [Google Scholar]
- 6.Gardner FJ, Konje JC, Abrams KR, et al. Endometrial protection from tamoxifen-stimulated changes by a levonorgestrel-releasing intrauterine system: a randomised controlled trial. Lancet 2000;356:1711–17. [DOI] [PubMed] [Google Scholar]
- 7.Critchley HOD, Wang H, Jones RL, et al. Morphological and functional features of endometrial decidualization following long-term intrauterine levonorgestrel delivery. Hum Reprod 1998;13:1218–24. [DOI] [PubMed] [Google Scholar]
- 8.Silverberg SG, Haukhamaa M, Arko H, et al. Endometrial morphology during long term use of levonorgestrel-releasing intrauterine devices. Int J Gynecol Pathol 1986;15:235–41. [DOI] [PubMed] [Google Scholar]
- 9.McCluggage WG, Kirk SJ. Pregnancy associated endometriosis with pronounced stromal myxoid change. J Clin Pathol 2000;53:241–2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clement PB, Granai CO, Young RH, et al. Endometriosis with myxoid change. A case simulating pseudomyxoma peritonei. Am J Surg Pathol 1994;18:849–53. [DOI] [PubMed] [Google Scholar]
- 11.Nogades FF, Martin F, Linares J, et al. Myxoid change in decidualised scar endometriosis mimicking malignancy. J Cutan Pathol 1993;20:87–91. [DOI] [PubMed] [Google Scholar]
- 12.Wang C, Wang C, Huang H, et al. Fertility-preserving treatment in young patients with endometrial adenocarcinoma. Cancer 2002;94:2192–8. [DOI] [PubMed] [Google Scholar]
- 13.Thornton JG, Brown LA, Wells M, et al. Primary treatment of endometrial cancer with progestagen alone. Lancet 1985;2:207–8. [DOI] [PubMed] [Google Scholar]
- 14.Randall TC, Kurman RJ. Progestin treatment of atypical hyperplasia and well differentiated carcinoma of the endometrium in women under age 40. Obstet Gynecol 1997;90:434–40. [DOI] [PubMed] [Google Scholar]
- 15.Figueroa-Casas PR, Ettinger B, Delgado E, et al. Reversal by medical treatment of endometrial hyperplasia caused by estrogen replacement therapy. Menopause 2001;8:420–3. [DOI] [PubMed] [Google Scholar]
- 16.Montz FJ, Bristow RE, Bovicelli A, et al. Intrauterine progesterone treatment of early endometrial cancer. Am J Obstet Gynecol 2002;186:651–7. [DOI] [PubMed] [Google Scholar]