Abstract
Background: Increased cancer incidence, particularly lymphoproliferative disease, is a complication of immunosuppression in organ transplantation. Non-Hodgkin’s lymphomas (NHLs) occur frequently during the first year after transplantation, more so in North America than in Europe.
Methods: This study audited and correlated the demographic, clinical, pathological, and outcome features of post-transplant lymphoproliferative disorders (PTLDs) in a large centre in Oxford, and assessed whether the time of onset fitted more with the European or North American pattern.
Results: There were 1383 renal transplants in the study period and 27 patients developed lymphoma: 26 NHLs and one Hodgkin’s disease (1.95%). Four of the patients never received cyclosporin. The mean time of diagnosis after transplant was 46 months. Most tumours (21/27) presented extranodally. Management included reduction of immunosuppression, surgical excision, antiviral treatment, radiotherapy, and chemotherapy. Three patients presented in the first post-transplant year—0.34% of cyclosporin managed patients—similar to the North American incidence, although the incidence of extranodal late PTLDs was also high (mean onset, 36 months v 15 months international mean). Post-transplant lymphomas were the most common malignancy associated with death in transplant patients.
Conclusions: PTLDs occurred in 2% of renal transplant patients, presenting both in the first year in association with cyclosporin use, as in North America, but also in subsequent years, giving an overall presentation time later than the international mean. The disease usually presented extranodally, accounting for the wide range of symptoms and signs. Despite awareness and active management, the disease contributed to death in more that 50% of patients with PTLDs.
Keywords: lymphoproliferative, disorders, renal, transplants
The risk of non-Hodgkin’s lymphoma (NHL) or post-transplant lymphoproliferative disease (PTLD) in organ transplant recipients has long been recognised to be high, and is a complication of immunosuppressive treatment.1 A multicentre study reported in 1993 that the NHL rate was especially high during the first post-transplant year among kidney transplant patients and that the first year incidence was higher in North America than in Europe, the major centres available for comparison in the study.2
Detailed clinicopathological studies, particularly from the USA,3,4 have described the location, clonality, biological nature (in particular, Epstein-Barr virus (EBV) status), and responsiveness to management of these lymphoproliferative disorders. Relatively few detailed studies of this transplant complication have been undertaken outside of the USA and in particular in the UK.
“A multicentre study reported in 1993 that the non-Hodgkin’s lymphoma rate was especially high during the first post-transplant year among kidney transplant patients and that the first year incidence was higher in North America than in Europe”
The aim of our study was to describe the essential demographic, clinicopathological, and outcome features of PTLDs in a European, and in particular a UK, transplant centre. We wanted to find out whether the UK experience of this disease was comparable to other descriptions and, in particular, whether our patients showed the European pattern as opposed to the prominent first year incidence found in the USA.2
MATERIALS AND METHODS
Patient population
The Oxford Transplant Centre undertook 1383 renal transplants from January 1975 until May 1996. From the start, the awareness of increased malignancy in transplant patients led to careful examination for, and the prospective documentation of, neoplastic complications.5 The prospectively maintained tumour register included 27 patients in whom the diagnosis of lymphoma or post-transplant lymphoid proliferation had been made. This included one patient with the diagnosis of Hodgkin’s disease, the remainder being categorised as non-Hodgkin’s lymphoma.
Histological evaluation
Formalin fixed, paraffin wax embedded histological sections from all 27 patients were available for review by three pathologists: WDB, MAD, and KCG. Immunocytochemical stains were performed to establish the lymphoid nature of the lesions (leucocyte common antigen); the type of cell—B cell (L26, JCB117) or T cell (CD3); the distinction between Hodgkin’s and non-Hodgkin’s disease using antibodies to CD15 (By87a) and CD30 (BerH2), respectively; and to establish the EBV status of the tumours (latent membrane protein; CS 1–4). In most cases κ and λ light chain staining was performed to help evaluate clonality but, like others, we found that these stains were seldom helpful and we have not included the results.
Clinical and demographic evaluation
A range of demographic, clinical, and outcome information was obtained from the patients’ transplant folders. In common with other centres, a variety of therapeutic interventions were applied to these patients over the time span of this retrospective study, reflecting in part the uncertainty regarding the natural history and response of these tumours.
RESULTS
Patient population and tumour incidence
There were 18 male and nine female patients (M : F ratio, 2 : 1). The age at first transplant ranged from 13 to 65 years, with a mean of 46 years and a median of 51 years (table 1).
Table 1.
Patient population and tumour incidence
| Patient | Age at 1st transplant | Sex | CyA | ATG | OKT3 | Months to lymphoma |
| Alive | ||||||
| 1 | 13 | M | Yes | No | No | 43 |
| 2 | 51 | F | Yes | Yes | No | 42 |
| 3 | 42 | F | Yes | No | No | 12 |
| 4 | 60 | M | Yes | No | No | 17 |
| 5 | 38 | M | Yes | No | No | 33 |
| 6 | 25 | F | Yes | No | No | 5 |
| 7 | 29 | M | Yes | No | No | 39 |
| 8 | 49 | F | Yes | No | No | 12 |
| 9 | 26 | F | Yes | No | No | 52 |
| 10 | 41 | M | Yes | Yes (1+2 Tx) | No | 79 |
| Dead | ||||||
| 11 | 53 | M | Yes | No | No | 68 |
| 12 | 56 | F | Yes | Yes (1+2 Tx) | Yes | 7 |
| 13 | 51 | M | No | No | No | 14 |
| 14 | 60 | M | Yes | No | No | 67 |
| 15 | 26 | M | Yes | No | No | 70 |
| 16 | 62 | M | Yes | No | No | 72 |
| 17 | 52 | M | No | No | No | 93 |
| 18 | 53 | M | Yes | No | No | 17 |
| 19 | 54 | M | Yes | No | No | 105 |
| 20 | 47 | M | Yes | Yes (1 No 2Tx) | No | 16 |
| 21 | 39 | F | Yes | No | No | 13 |
| 22 | 64 | F | Yes | No | No | 8 |
| 23 | 34 | M | No | No | No | 232 |
| 24 | 65 | F | Yes | Yes | No | 50 |
| 25 | 57 | M | Yes | No | No | 38 |
| 26 | 57 | M | Yes | Yes | No | 37 |
| 27 | 54 | M | No | No | No | 15 |
ATG, antithymocyte globulin; CyA, cyclosporin; OKT 3, anti-CD3 monoclonal antibody; Tx, transplant.
Immunosuppressive protocols
Twenty three of the 27 patients received initial immunsuppression based on the use of cyclosporin (CyA), whereas four patients had never received CyA (table 1). (Before 1980, patients (498) were treated with an azathiaprine based protocol, after which CyA was gradually introduced, and by 1984 CyA was used routinely, often in combination with prednisolone. From 1995 onwards a uniform triple treatment regimen with CyA, azathiaprine, and prednisone was used.) Six patients had also been treated with antithymocyte globulin (ATG), two of these with both their first and second transplants, the lymphoma developing with the second transplant. One patient had ATG with the first transplant but not the second when the lymphoma presented. One patient had ATG with the first transplant and ATG in addition to OKT 3 (anti-CD3 monoclonal antibody) with the second transplant.
Time to tumour onset
The time interval between renal transplantation and lymphoma diagnosis ranged from five to 232 months, with a mean of 46 and a median of 38 (table 1). The fact that the earlier patients did not receive CyA meant that the patient with the longest interval (232 months), who received azathioprine and steroids, raised the overall mean of the non-CyA group (14, 15, 93, 232) to 88.5 months. Cases presenting within the first year of transplant only occurred after the introduction of CyA (three cases).
Year of diagnosis
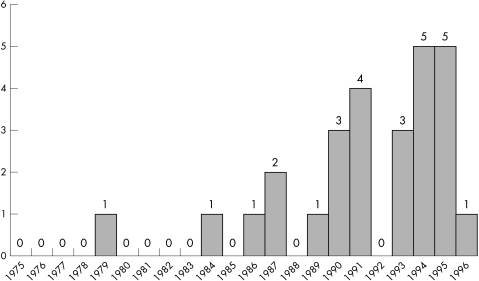
It can be seen that in the first decade of renal transplantation at Oxford during which time 479 transplants were carried out, only two patients presented with PTLD (fig 1). During the following 11 years, with naturally many more long term survivors, the disease presented more often, with five cases in both 1994 and 1995. Figure 1 shows the number of cases of lymphoma for each year.
Figure 1.
Lymphomas by year of diagnosis.
Clinical presentation
The presentations included a wide range of symptoms and signs, reflecting the range of tissues and organs involved by lymphoproliferative disease (table 2). The effects included constitutional symptoms, in addition to those linked more directly to the site of involvement (table 2).
Table 2.
Clinical presentation
| Patient | Clinical presentation | Site | Group |
| Alive | |||
| 1 | Pyrexia/lymphadenopathy | Neck | LN |
| 2 | Ulcerating skin lesion | Behind ear | Skin |
| 3 | Headache/personality change | CNS | CNS |
| 4 | Abdominal pain/mass | Ileum, caecum | Abd |
| 5 | Weight loss/lymphadenopathy | Inguinal LN | LN |
| 6 | Soft tissue swelling | Neck | Skin/ST |
| 7 | Facial pain/nasal blockage | Nasal cavity | Head |
| 8 | Fever/night sweats | Lung | Lung |
| 9 | Skin/soft tissue swelling | Neck | Skin/ST |
| 10 | Haemoptysis/melaena | Small bowel | Abd |
| Dead | |||
| 11 | Enlarging lymph node | Neck | LN |
| 12 | Headache/visual and memory problems | CNS | CNS |
| 13 | Lung mass on routine chest x ray | Lung | Lung |
| 14 | Neck swelling | Laryngeal | Head |
| 15 | Enlarging lymph node | Neck | LN |
| 16 | Purple skin lesion | Forehead | Skin |
| 17 | Weight loss/diarrhoea | Small bowel | Abd |
| 18 | Fever/abdominal pain | Adrenal | Abd |
| 19 | Weight loss/epigastric pain | Para-aortic LN | LN |
| 20 | Necrotic skin lesion | Chest wall | Skin |
| 21 | Confusion/fever | CNS | CNS |
| 22 | Nerve deafness | CNS | CNS |
| 23 | Fever/abdominal mass | Sigmoid colon | Abd |
| 24 | Weight loss/confusion/pneumonia | Lung | Lung |
| 25 | Fatigue/lymphadenopathy | Neck | LN |
| 26 | Unwell/flank pain | Psoas muscle | Deep ST |
| 27 | Cough/wheeze | Lung | Lung |
Abd, abdominal; CNS, central nervous tissue; LN, lymph node; ST, soft tissue.
As recommended by Nalesnik,3 an attempt was make to categorise the patients according to the predominant site of the initial symptoms. The most striking finding, linked to the diversity of presentation, was that most of the lesions (21 of 27) were extranodal. Six of the lesions were in the skin and soft tissues, five in the abdomen (two each in small and large bowel), four in the central nervous system (CNS), four in the lung, and two in the head and neck area. The six nodal presentations comprised four in cervical nodes (including the Hodgkin’s disease case), one inguinal, and one para-aortic.
Pathological features of lesions
Gross pathology
These post-transplant lymphoid lesions may appear as a solid tumour, diffuse infiltrates of parenchymal organs, or enlargement of native lymphoid tissue.3 They are similar to lymphomas at a macroscopic level. Some lesions in this series were described as having fleshy white cut surfaces and in the larger lesions necrosis was frequently seen. The psoas tumour (case 26) was described as a “caseating mass”.
Microscopic pathology
The microscopic appearance of PTLD is that of a diffuse proliferation of lymphoid cells. Attempts have been made to characterise the lesion on the basis of the presence or absence of lymphocyte heterogeneity. In many lesions, the entire range of recognisable B cell forms is seen, in varying proportions. These can include small lymphocytes, small and large cleaved and non-cleaved lymphocytes, immunoblasts, plasmacytoid cells, and plasma cells.
Monomorphic PTLDs are composed of uniform lymphoid cells, overwhelmingly at one stage of differentiation, usually small or large non-cleaved lymphocytes. In general, plasma cell differentiation is not a feature of such lesions and the appearance is that of typical NHL.
We attempted to classify the lesions by the Pittsburgh3 and Minnesota6 systems, in addition to the revised European–American lymphoma (REAL) classification (table 3).7
Table 3.
Pathological classification
| Patient | REAL | Pittsburgh | Minnesota | B cell | EBV LMP-1 |
| Alive | |||||
| 1 | LC | MM | 5 | Positive | Positive |
| 2 | LC | MP | 5 | Positive | Positive |
| 3 | LC | MM | 4 | Positive | ? |
| 4 | LC | MP | 4 | Positive | Positive |
| 5 | LC | MP | 4 | Positive | Positive |
| 6 | LC | MP | 5 | Positive | Positive |
| 7 | LC | MM | 4 | Positive | Positive |
| 8 | LC | MP | 4 | Positive | Positive |
| 9 | LPC | P | 2 | Positive | Positive |
| 10 | LC | MM | 4 | Positive | Negative |
| Dead | |||||
| 11 | LC | MP | 4 | Positive | Positive |
| 12 | LC | MP | 4 | Positive | Positive |
| 13 | LC | MM | 4 | Positive | Positive |
| 14 | LC | MM | 4 | Positive | Positive |
| 15 | HD MC | HD MC | HD MC | Positive | Positive |
| 16 | LC | MP | 4 | Positive | Positive |
| 17 | Marginal zone | P | 2 | Positive | Positive |
| 18 | LC | MP | 4 | Positive | Positive |
| 19 | LC | MM | 5 | Positive | ? |
| 20 | LC | MP | 4 | Positive | Positive |
| 21 | HG ? type | MM | 4 | Positive | Positive |
| 22 | LC | MM | 4 | Positive | Positive |
| 23 | LC | MM | 5 | Positive | Positive |
| 24 | LPC | P | 2 | Positive | Positive |
| 25 | LPC | P | 2 | Positive | Positive |
| 26 | LC | MM | 5 | Positive | Positive |
| 27 | LC | MP | 4 | Positive | Positive |
REAL: HG ? type, high grade lymphoma of uncertain type; LC, large cell; LPC, lymphoplasmocytic. Pittsburgh: MM, monomorphous; MP, minimally polymorphous; P, polymorphous. Minnesota: 2, polymorphous diffuse B cell hyperplasia; 4, polymorphous B cell lymphoma; 5, immunoblastic sarcoma. EBV LMP-1, Epstein-Barr virus latent membrane protein 1; HD MC, Hodgkin’s disease, mixed cellularity subtype.
The case of Hodgkin’s disease, initially diagnosed elsewhere, was confirmed both by haematoxylin and eosin morphology, and by the positive staining in Reed-Sternberg type cells for CD15 and CD30. It was viewed as the mixed cellularity form.
The remaining 26 cases were all B cell positive (either or both of L26 and JCB117) and in 24 of the 27 cases, including the Hodgkin’s disease case, tumour cells were positive for EBV. Most of the NHLs (21 of 26) were large cell lymphomas according to the REAL classification; when the Pittsburgh classification was used, 11 were monomorphous, 11 minimally polymorphous, and four were polymorphous, whereas using the Minnesota categorisation 16 were polymorphous B cell lymphomas, six were immunoblastic sarcomas, and four were polymorphous diffuse B cell hyperplasia.
Analysis of tumour clonality
Although staining for κ and λ light chains was carried out in all cases, the results were seldom unequivocal and have therefore been excluded. It would be of value and interest to pursue the clonality of these lesions by more reliable techniques. (It should be emphasised that this is not easy and the results thus far are not clear cut or of obvious clinical value.)3
Clinicopathological correlation: clinical presentation, and extent of tumour
The manner of presentation of each individual patient provided a guide to the site of predominant pathology. The presence of constitutional symptoms and the difficulty of excluding infections in locations such as the lung complicated these correlations and sometimes led to delays. It was not clear from our data whether any location was better or worse than others, but factors such as time of presentation and extent of disease may have complicated the issue.
Management
Table 4 details the management of the patients. Of the 27 patients, four had resections of the lesions (in three cases bowel and one lung wedge resection), one had the diagnosis made on initial pleural cytology, followed by necropsy, whereas the remainder had biopsies which in some cases were also excisions. In 20 patients, immunosuppression was initially reduced, usually as the first line of treatment, and in four patients immunsuppression was stopped. (In one patient it was later started again.) Acylovir (an antiviral drug) was used in 13 patients, and it was attempted in one other patient, who was unable to tolerate it. Radiotherapy was used in 13 patients and various forms of polychemotherapy in nine, including three patients who also had radiotherapy. Of those alive in September 1996, our end point, only three had not had specific antilymphoma treatment; namely, patient 2 with a small skin lesion that was excised, patient 4 with ileum and caecum resected, and patient 9 with neck skin/soft tissue/lymph node lesions.
Table 4.
Management
| Patient | Bx excision | Decreased immunosuppression | Acyclovir | RT/ Chemotherapy |
| Alive | ||||
| 1 | Ex Bx | Yes later stopped | Yes | C |
| 2 | Ex Bx | No | No | No |
| 3 | Bx | Yes | Yes | RT |
| 4 | Resection | Yes | Yes | No |
| 5 | Bx | Yes | Yes | RT+C |
| 6 | Bx | Yes | Yes | RT |
| 7 | Bx | Yes later stopped | Yes | RT |
| 8 | Wedge resection | Yes | Yes | RT |
| 9 | Ex Bx | Yes | Attempted | No |
| 10 | Resection | Yes | No | C |
| Died | ||||
| 11 | Ex Bx | Yes | Yes | RT+C |
| 12 | Bx | Yes | No | RT |
| 13 | Bx | Yes stopped+No | Yes | C |
| 14 | Bx+PM | Yes | Yes | RT |
| 15 | Bx+PM | ? | ? | RT |
| 16 | Bx | No | No | RT |
| 17 | Resection | Yes ?not initially | No | No |
| 18 | Bx | Yes | Yes | C |
| 19 | Bx | Yes | Yes | C |
| 20 | Bx | No | No | RT |
| 21 | Bx | Yes | No | RT+C |
| 22 | Bx | Yes | No | RT |
| 23 | Bx | Stopped | Yes | No |
| 24 | Cytology+PM | No | No | No |
| 25 | Bx | Yes | No | C |
| 26 | Bx | Yes | No | No |
| 27 | Bx+PM | No | No | No |
Bx, biopsy; C, chemotherapy; Ex, excision; PM, postmortem examination; RT, radiotherapy.
Four of the five patients who survived less than one month did not really have the opportunity for planned management. In patients 24 and 27 the diagnosis was made when they were in a terminal condition, patient 23 was known to have extensive lymphoma intra-abdominally postoperatively, and patient 26 was also too ill for specific treatment. Patient 25 was given a short course of chlorambucil in addition to decreasing immunosuppression.
Response to treatment and outcome
Table 5 details the response to treatment and outcome in the 27 patients. At the end point of this study (September 1996), 10 of the patients were still alive, nine with functioning grafts and eight with no evidence of residual disease. Two patients had suffered graft failures as a result of reduced immunosuppression; one was on dialysis, whereas the other had undergone a second transplant 60 months after the first had been allowed to fail. The second transplant was still working well. (Since the end of the study period, in November 1996, a further patient lost his graft as a result of reduced immunsuppression.)
Table 5.
Response to treatment and outcome
| Patient | Follow up post-transplant (months) | Outcome | Follow up (months) | Response to treatment |
| Alive | ||||
| 1 | 152 | NED | 108 | RES |
| 2 | 122 | NED | 80 | RES |
| 3 | 46 | NED CaB | 34 | RES |
| 4 | 46 | NED | 29 | RES |
| 5 | 61 | ? | 28 | PTR |
| 6 | 31 | NED | 26 | RES |
| 7 | 61 | NED GF | 22 | RES |
| 8 | 31 | NED | 19 | RES |
| 9 | 62 | NED | 10 | REG |
| 10 | 85 | ? | 6 | PTR |
| Died | ||||
| 11 | 125 | T 91 | 57 | PTR |
| 12 | 55 | T 94 | 48 | PTR |
| 13 | 50 | ?87 | 36 | PTR |
| 14 | 91 | 95 | 24 | RES |
| 15 | 92 | T 93 | 22 | PTR |
| 16 | 89 | 92 | 17 | RES |
| 17 | 106 | T 88 | 13 | PTR |
| 18 | 24 | T 95 | 7 | NR |
| 19 | 110 | T 94 | 5 | NR |
| 20 | 18 | T 90 | 2 | NR |
| 21 | 15 | T 93 | 2 | NR |
| 22 | 9 | T 91 | 1 | NR |
| 23 | 232 | T 95 | 0 | NT |
| 24 | 50 | T 95 | 0 | NT |
| 25 | 38 | T 91 | 0 | NT |
| 26 | 37 | T 90 | 0 | NT |
| 27 | 15 | T 79 | 0 | NT |
Outcome: CaB, carcinoma of breast; GF, graft failure; NED, no evidence of disease; T 94 (other number), patient died in 1994 (other year) of/or with lymphoma; ?87, not clear about role of lymphoma in death of patient. Response to treatment: NR, no response; NT, necropsy or terminal diagnosis; PTR, partial tumour resolution; REG, regression; RES, resolution.
Of the 17 patients who had died, 14 were assessed to have died of their lymphoma, or at least with their lymphoma still clinically relevant. In eight patients, the time interval from diagnosis to death was less than two months, despite awareness of this disease and careful and regular patient follow up.
The Starzl group categorised the response of 43 PTLDs into groups showing regression with reduced immunosuppression, resolution, no evaluable response, no response, and postmortem diagnosis only. There are many uncertainties involved in trying to categorise our patients into such broad response categories. Only one of our 27 patients has shown regression (case 9), nine have shown resolution, seven showed partial or temporary resolution or response, five showed little or no response, whereas five were essentially terminal or postmortem diagnoses (table 5).
Oxford post-transplant malignancy experience
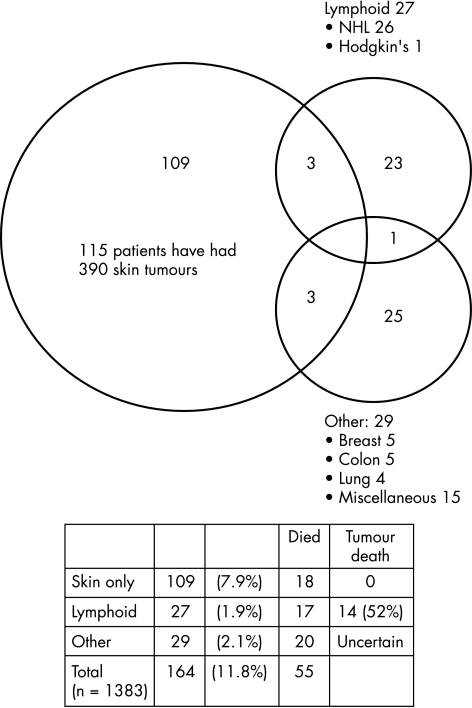
To place the frequency and mortality of the post-transplant lymphomas in perspective the available data on the tumour registry with regard to other malignancies were analysed. The data confirm that even in the relatively northern latitude of Oxford, skin malignancy is the most frequent form, with 115 patients having had 390 skin tumours by April 1996 (fig 2). Most of these were squamous cell carcinomas, with fewer basal cell carcinomas and in situ carcinomas.5 All the patients had at least one squamous or basal cell carcinoma. Eighteen of the 115 patients who had skin malignancies had died, but none was considered to have died of the skin malignancy.
Figure 2.
Oxford post-transplant malignancies. NHL, non-Hodgkin’s lymphoma.
The other major group of cancers was non-skin, non-lymphoid cancer, where a total of 29 were registered. Breast, colon, and lung were the main types, accounting for half of the malignancies (table 6). Of the 29 patients in this group, 20 had died by September 1996. The overall mortality rate in this group of 20 of 29 (69%) is similar to the lymphoma group of 17 of 27 (63%).
Table 6.
Non-skin, non-lymphoid malignancies
| Type | N |
| Breast | 5 |
| Colon | 5 |
| Lung | 4 |
| Hepatocellular carcinoma | 1 |
| Seminoma | 1 |
| Melanoma | 1 |
| Haemangioendothelioma | 1 |
| Prostatic adenocarcinoma | 1 |
| Sebaceous carcinoma | 1 |
| Anal carcinoma | 1 |
| Renal cell carcinoma (one recurrence of pretransplant tumour) | 2 |
| Ovarian cystadenocarcinoma | 1 |
| Oesophagus (adenocarcinoma) | 1 |
| Bladder | 1 |
| Adenocarcinoma metastases (primary uncertain) | 3 |
| Total | 29 |
DISCUSSION
One of the earliest reports of de novo malignancy after cadaveric renal transplantation was of two fatal extranodal lymphomas found in the liver and CNS.8 In a subsequent early multicentre report of post-transplant malignancies, lymphomas constituted approximately 40% of all non-skin tumours, with a predilection for the CNS.9 In time, the diagnosis of other non-skin malignancies, usually appearing later, reduced the proportion made up by lymphomas. By 1991, the Cincinatti transplant tumour registry was noting a lymphoma frequency of 21% compared with 5% in the general population when non-melanoma skin cancers and in-situ carcinoma of the cervix were excluded.10 In Australia and New Zealand, with a large comprehensive post-renal transplant tumour registry, the 54 lymphomas constituted 12% of the non-skin cancers by 1991.11 It is of interest that no Hodgkin’s disease had been diagnosed in this group of 459 malignancies and that 16 of the 54 lymphomas were cerebral. Sheil has emphasised that since the introduction of CyA a similar pattern of incidence in these new cohorts could occur, and a recent publication from the Oxford group, which specifically examined this point, was in broad agreement.12
In patients treated with CyA, lymphomas have again constituted almost 40% of non-skin malignancies. Because the proportion of lymphomas fell progressively in the pre-CyA era, it is possible that a similar reduction could occur in the CyA era.11
Penn noted that several features of the lymphomas in the overall CyA group were different from those seen in the azothiaprine group.10 Since the introduction of CyA, first Penn, and then Opelz, recorded an increased frequency of lymphoproliferative disease.2,10 Our group of 498 patients who had taken azothiaprine after transplantation included only four PTLD cases, despite a long follow up period (four of 498; 0.8%), in contrast with 22 of 885 (2.4%) since the introduction of CyA, with shorter follow up. In addition, the CyA group internationally showed earlier occurrence, at 15 versus 48 months post-transplantation. In Oxford, presentation within the first year after transplantation has only occurred since the introduction of CyA (patients presenting at five, seven, and eight months), with two further patients presenting at 12 months.
Three of 885 (0.34%) CyA managed patients developed PTLD in the first post-transplant year, similar to the incidence seen in North American. However, the relatively high incidence in subsequent years gave a later mean onset for the Oxford CyA group of 36 months versus the 15 month international mean.
In the CyA group studied by Penn, lymph nodes were more frequently involved (39% v 23%). The Oxford group of 26 B cell lymphomas included five nodal and 21 extranodal tumours. All four patients who had never received CyA presented extranodally, whereas five of the 22 in the CyA group had lymph node involvement only. In the CyA group described by Penn, the CNS was less frequently involved (15% v 38%). Our experience of four nodal lymphomas out of 22 B cell non-Hodgkin’s lymphomas fits well with the general CyA experience. It should be emphasised that one of the earliest multicentre reports on lymphomas found a high CNS frequency in patients treated with azathioprine.9
A central question is whether these lesions are really lymphomas and should be classified and managed as such. Although it was clear from the start that they could be fatal like other lymphomas, there has also been the suggestion, with some evidence, that they may be different with different management leading to a far better prognosis. An early paper from Starzl et al in 198413 suggested that these lesions usually had a good outcome with reduction or discontinuance of immunosuppression, strongly questioning whether they needed to be viewed as seriously as normal lymphomas. However, many of their initial patients had other treatments, including surgery, cytotoxic drugs, and radiotherapy, making it difficult to ascribe improvement only to the reduction in immunosuppression.13 The clinical advisory committee of the new World Health Organisation classification of neoplastic diseases of the haemopoeitic and lymphoid tissues maintains that although a separate classification is not needed for immunodeficiency associated lymphomas, a separate classification of PTLDs would be useful, because of their distinctive biological and clinical features.14 This classification of PTLDs has four groups:
Early lesions such as reactive plasmacytic hyperplasia.
PTLD—polymorphic.
PTLD—monomorphic (which they suggest should be classified according to current lymphoma classification—for example, the REAL classification system).
Other types, such as Hodgkin’s disease.
As a good illustration of the evolution of understanding of these lymphoid lesions and the management of these patients, it interesting that in subsequent publications from the Starzl group,3 a broader, more complex perspective had developed, and of 43 PTLDs only nine were categorised as regressing in response to reduction of immunosuppression only, with or without acyclovir. They had also decided to preclude patients from this category if there had been surgical resection of all grossly evident tumour (as in five of eight of the original series of renal transplant patients),13 or if they had received chemotherapy or radiotherapy. These patients were placed in a group termed tumour resolution (including the above mentioned cases)—a large and encouraging group of 20 of 43. The remaining patients were in the categories of no evaluable response and no response (eight of 43) or postmortem diagnosis only (six of 43).
It can be seen from table 5 that follow up of the lymphoma was only longer than 36 months in two patients who were still alive in September 1996. Therefore, it seems appropriate to be cautious about the apparent resolution or regression of disease in patients 3 to 10. It can be seen that two of those who died of lymphoma survived more than 36 months after that diagnosis.
“All involved with possible tumours in the post-transplant context should have a high index of suspicion for lymphoma”
Two of these cases were not diagnosed as lymphoid proliferations on initial histological examination, the diagnosis being altered during this review. One was the first Oxford patient who presented preterminally with respiratory symptoms and in whom a small bronchial biopsy was diagnosed as undifferentiated carcinoma. The patient died away from Oxford a few days later and at necropsy a widespread lymphoma affecting the lungs was diagnosed. In this case, the correct diagnosis would probably have made little or no difference to management and outcome.
In the second patient, a small bowel lesion was resected and diagnosed as Crohn’s disease 11 months before presentation with documented lymphoma in the vicinity of the submandibular gland. In retrospect and with lymphoid and EBV markers the earlier small bowel lesion was PTLD. This diagnosis may well have altered management, with possible immunosuppression reduction after the surgical excision and greater clinical suspicion of subsequent recurrence or lymphoma development.
It seems clear that all involved with possible tumours in the post-transplant context should have a high index of suspicion for lymphoma. In our experience—for example, this diagnosis is as likely as all the other non-skin malignancies together in a patient who has undergone renal transplantation. Although this may be a temporary situation and many other centres have a lower proportion of lymphomas it remains a frequent and important diagnosis with considerable morbidity and mortality.
Two UK studies have described the overall experience of post-renal transplant malignancy at the Hammersmith Hospital in London and in Leeds.15,16 Our series comprised more patients and documented more lymphoproliferative disorders, which constituted a larger proportion of the non-skin malignancies (49%), compared with 18% and 27% in the other two series. The median time of appearance of 38 months was also shorter in our group.
We report a relatively high overall tumour incidence and an apparently high lymphoma frequency, in particular, in relation to non-skin, non-lymphoid lesions. In contrast to the Australian and New Zealand transplant cancer registry of 459 non-skin malignancies, where the 54 lymphomas were 12% of the total,11 our 27 lymphomas constitute almost half of the total number of malignancies (27 of 55). These figures were noticeably affected by the appearance of 10 lymphomas in 1994 to 1995, at least eight or nine years after the initial routine use of CyA. Whether these patients represent an unfortunate statistical variation or a real alteration in frequency or response is not yet clear. It is also uncertain to what extent the prospectively maintained tumour registry and careful follow up may contribute to the apparently high overall tumour figures at Oxford. It should be noted that the Leeds group emphasised how difficult it was to gather retrospective clinical and pathological records of malignancies in transplant patients.16
In the home country of the first author, South Africa, lymphoid tumours appear to be a less frequent risk of transplant immunosuppression. Uterine cervical neoplasms and Kaposi’s sarcoma are two malignancies not seen in our group, which are relatively frequent in South African renal transplant patients.17,18
PTLDs are relatively infrequent, but because of uncertainty regarding their most appropriate management and their contribution to transplant recipient morbidity and mortality, they constitute an important ongoing challenge in transplantation.
Take home messages.
In Oxford, the overall incidence of post-transplant lymphoproliferative disorders (PTLDs) in renal transplant patients was 2%
PTLDs presented both in the first year in association with cyclosporin use, as in North America, but also frequently in subsequent years, giving an overall presentation time later than the international mean
Tumours usually presented extranodally, which accounts for the wide range of symptoms and signs encountered
Despite awareness and active management, the disease contributed to death in more that half of patients with PTLDs.
Acknowledgments
Thanks to S Biddolph and G Flack for much of the immunohistochemical staining. In addition, thanks to Dr RW Simpson from Exeter for the referral of material and Exeter Hospital for the initial diagnosis of Hodgkin’s disease in patient 15.
Abbreviations
CNS, central nervous system
CyA, cyclosporin
EBV, Epstein-Barr virus
NHL, non-Hodgkin’s lymphoma
PTLD, post-transplant lymphoproliferative disease
REAL, revised European American lymphoma
REFERENCES
- 1.Penn I, Hammond W, Brettschneider L, et al. Malignant lymphomas in transplantation patients. Transplant Proc 1969;1:106–12. [PMC free article] [PubMed] [Google Scholar]
- 2.Opelz G, Henderson R. Incidence of non-Hodgkin lymphoma in kidney and heart transplant recipients. Lancet 1993;342:1514–16. [DOI] [PubMed] [Google Scholar]
- 3.Nalesnik MA, Jaffe R, Starzl TE, et al. The pathology of posttransplant lymphoproliferative disorders occurring in the setting of cyclosporin A–prednisone immunosuppression. Am J Pathol 1988;133:173–92. [PMC free article] [PubMed] [Google Scholar]
- 4.Harris NL, Ferry JA, Swerdlow SH. Posttransplant lymphoproliferative disorders: summary of Society for Hematopathology workshop. Semin Diagn Pathol 1997;14:8–14. [PubMed] [Google Scholar]
- 5.Liddington M, Richardson AJ, Higgins RM, et al. Skin cancer in renal transplant recipients. Br J Surg 1989;76:1002–5. [DOI] [PubMed] [Google Scholar]
- 6.Frizzera G, Hanto DW, Gajl-Peczalska KJ, et al. Polymorphic diffuse B-cell hyperplasias and lymphomas in renal transplant recipients. Cancer Res 1981;41(11 Pt 1):4262–79. [PubMed] [Google Scholar]
- 7.Harris NL, Jaffe ES, Stein H, et al. A revised European–American classification of lymphoid neoplasms: a proposal from the international lymphoma study group. Blood 1994;84:1361–92. [PubMed] [Google Scholar]
- 8.Doak PB, Montgomerie JZ, North JD, et al. Reticulum cell sarcoma after renal homotransplantation and azathioprine and prednisone therapy. BMJ 1968;4:746–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schneck SA, Penn I. De-novo brain tumours in renal-transplant recipients. Lancet 1971;1:983–6. [DOI] [PubMed] [Google Scholar]
- 10.Penn I. The changing pattern of posttransplant malignancies. Transplant Proc 1991;23(1 Pt 2):1101–3. [PubMed] [Google Scholar]
- 11.Sheil AG, Flavel S, Disney AP, et al. Cancer development in patients progressing to dialysis and renal transplantation. Transplant Proc 1985;17:1685–8. [PubMed] [Google Scholar]
- 12.Libertiny G, Watson CJ, Gray DW, et al. Rising incidence of post-transplant lymphoproliferative disease in kidney transplant recipients. Br J Surg 2001;88:1330–4. [DOI] [PubMed] [Google Scholar]
- 13.Starzl TE, Nalesnik MA, Porter KA, et al. Reversibility of lymphomas and lymphoproliferative lesions developing under cyclosporin–steroid therapy. Lancet 1984;1:583–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harris NL, Jaffe ES, Diebold J, et al. The World Health Organisation classification of neoplastic diseases of the haematopoietic and lymphoid tissues: report of the clinical advisory committee meeting, Airlie House, Virginia, November 1997. Histopathology 2000;36:69–86. [DOI] [PubMed] [Google Scholar]
- 15.Gaya SB, Rees AJ, Lechler RI, et al. Malignant disease in patients with long-term renal transplants. Transplantation 1995;59:1705–9. [DOI] [PubMed] [Google Scholar]
- 16.London NJ, Farmery SM, Will EJ, et al. Risk of neoplasia in renal transplant patients. Lancet 1995;346:403–6. [DOI] [PubMed] [Google Scholar]
- 17.Margolius L, Stein M, Spencer D, et al. Kaposi’s sarcoma in renal transplant recipients. Experience at Johannesburg Hospital, 1966–1989. S Afr Med J 1994;84:16–17. [PubMed] [Google Scholar]
- 18.Moosa MR, McBryne A. The development of malignancies in renal allograft recipients: the Tygerberg Hospital experience. S Afr J Surg 1997;35:156–64. [Google Scholar]