Abstract
Aims: Granulomatous mastitis (GM) is an uncommon breast lesion that mimics carcinoma. The fine needle aspiration cytological (FNAC) features of GM have rarely been discussed in the literature. These features are reported in eight histologically confirmed cases of GM.
Methods: A retrospective study was undertaken in which a diagnosis of GM had been made on histopathology, and the FNAC slides were reviewed and assessed for the presence of granulomas, necrosis, multinucleated giant cells, and inflammatory background cells. Polymerase chain reaction (PCR) for Mycobacterium tuberculosis was performed on the histological material to exclude tuberculosis.
Results: All cases were confirmed histologically and PCR for mycobacterial DNA was negative. In the FNACs, varying numbers of granulomas composed of epithelioid histiocytes were present in four cases. The same four cases showed giant cells of either foreign body or Langhan’s type. No necrosis was noted. Six cases showed many histiocytes, some plump and others epithelioid, in the background. The number of epithelioid histiocytes corresponded to the presence of granulomas. Neutrophils were the predominant background inflammatory cells in most cases (six).
Conclusions: The cytological diagnosis of GM is difficult because the features overlap with other aetiologies, including tuberculosis. Specific features are absent. The absence of necrosis and a predominantly neutrophilic infiltrate in the background favour a diagnosis of GM. This diagnosis should also be considered when abundant epithelioid histiocytes are seen in smears, even in the absence of granulomas. However, the definitive diagnosis of GM depends on histology from fine needle biopsies and negative microbiological investigations.
Keywords: breast, granulomatous mastitis, tuberculosis, granuloma
Granulomatous mastitis (GM) is an uncommon breast lesion that was first described by Kessler and Woolloch.1 The clinical features of GM are similar to carcinoma, thus generating some interest from various authors in this rare entity. In the literature, only a few large series have been reported, emphasising the histological,2–5 imaging,6–8 and cytological9–11 aspects, with series sizes ranging from six to 16 cases. The remaining cases were mostly single case reports dating back to 1990.12 The histological features of GM have been well described as consisting of non-caseating granuloma formation within the breast parenchyma and lobulitis with or without neutrophilic micro-abscess.13,14 In contrast, the cytological features have not been widely discussed. In our report, we describe a series of eight cases of GM, with emphasis on the cytological features including the cellularity, component cell types, granulomas, and background cells.
METHODS
The histology files from the Prince of Wales Hospital and Pamela Youde Eastern Hospital, Hong Kong were searched for granulomatous inflammation of the breast occurring between 1990 and 2002, and all the cases were retrieved and the slides reviewed. A total of 27 cases was found. Of these, 11 cases had fine needle aspiration cytology (FNAC) performed. In one case, the cytology slides were not found, and in two more cases the aspirate was of insufficient quantity. Therefore, eight cases were included in our report.
In both hospitals, the FNACs were performed either by radiologists under ultrasound guidance or by pathologists. When performed by radiologists, small 22 gauge needles attached to plastic tubing and 10 ml syringes were used. When performed by pathologists, 10 ml syringes in a holder were used with 22 to 23 gauge needles. Mild suction was applied after the needle penetrated the lesion. In most cases, direct smears were prepared from the material aspirated, and these were alcohol fixed and stained with either Papanicolaou (Pap) or haematoxylin and eosin (H&E), or with both stains. In some cases, cytospin preparations were made using the Shandon Cytospin III (Shandon, Runcorn, Cheshire, UK), at a centrifuge speed of 600 rpm for five minutes. In other cases, cell blocks were prepared from the remaining material and 4 μm H&E sections were prepared by routine paraffin wax embedding.
In all cases, the following cytological parameters were evaluated: the presence of granulomas; background necrosis; the relative proportion of component cells including epithelioid histiocytes, lymphocytes and neutrophils; and the presence and morphology of any multinucleated giant cells.
All the histological slides were reviewed, the diagnosis confirmed, and a Ziehl Neelsen stain was performed. In all cases, DNA was extracted from representative samples from the paraffin wax embedded material and was subjected to real time polymerase chain reaction (Taqman PCR) analysis for the IS6110 sequence of Mycobacterium tuberculosis and the samples were examined in triplicate. PCR products were examined for the presence of mycobacterial DNA. Tuberculosis was diagnosed when the cycle threshold was less than 40.
RESULTS
The eight cases were obtained from eight patients. Six patients had one FNAC of the breast lesion before excision, and two had two FNACs. In these last two patients, only the more representative FNAC was reviewed.
All the patients were women, and the mean age was 35 years (range, 25–52). In five cases the lesions were on the right and three were on the left. The number of slides for each case ranged from two to six (mean, four).
Four cases had granulomas in the smears, one had many, two had some, and one had scanty granulomas. The granulomas were composed of aggregates of epithelioid histiocytes showing reniform to oval nuclei and a moderate amount of cytoplasm (fig 1); no caseous necrosis was seen. No granulomas were seen in four cases. In the background, six cases showed epithelioid histiocytes. The morphology of these epithelioid histiocytes was similar to those seen constituting the granulomas. Out of these six cases, four cases showed a moderate to high number of epithelioid histiocytes, whereas two showed scanty epithelioid histiocytes (fig 2). The cellularity of these epithelioid histiocytes correlated with the presence of granulomas, and the two cases devoid of epithelioid histiocytes did not have granulomas. In four cases, multinucleated giant cells were seen (fig 3). These four cases also had granulomas. The giant cells were found in the background rather than within the granulomas. The number of nuclei ranged from about five to 15 within each giant cell, and they were arranged either irregularly or in a horseshoe manner. With regard to the other inflammatory cells, neutrophils accounted for most of the inflammatory cells in six cases, whereas lymphocytes were the predominant inflammatory cell type in two cases.
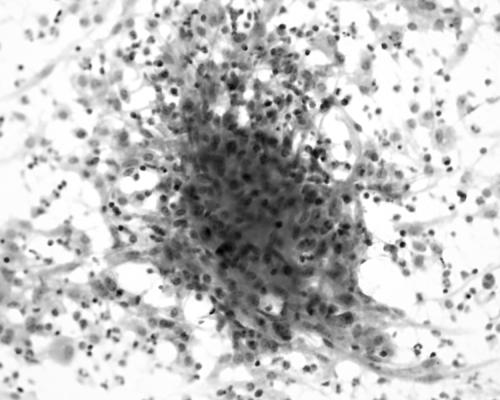
Figure 1.
Photomicrograph showing a granuloma in the cytology smear composed of epithelioid histiocytes in an inflammatory background (haematoxylin and eosin stain; original magnification, ×200).
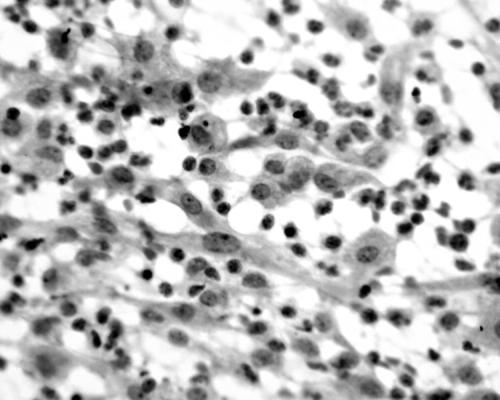
Figure 2.
Photomicrograph showing dense inflammatory cell infiltrate with many epithelioid histiocytes with reniform to oval nuclei and a moderate amount of cytoplasm (haematoxylin and eosin stain; original magnification, ×400).
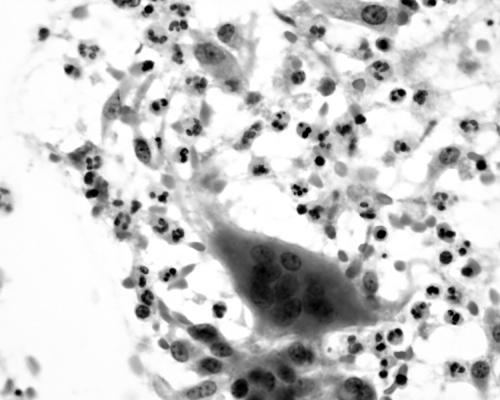
Figure 3.
Photomicrograph showing a multinucleated giant cell within a mixed inflammatory background (haematoxylin and eosin stain; original magnification, ×400).
Histological review of all the cases confirmed the diagnosis of granulomatous mastitis. For all the cases, Ziehl Neelsen staining for acid fast bacilli was negative, and Mycobacterium tuberculosis DNA was not detected by PCR in the histological specimens.
DISCUSSION
GM is an uncommon breast lesion that is well known for its worrisome clinical presentation as a hard breast lump, particularly in younger women. The aetiology of most cases is idiopathic, to be distinguished from the rare specific granulomatous conditions including tuberculosis, sarcoidosis, and Wegener’s granulomatosis. Clinically and radiologically, GM is difficult to distinguish from carcinoma. The disease usually occurs in women of reproductive age, and may be associated with lactation or may occur in the postpartum period. The course of the disease is characterised by slow resolution, which is often punctuated by abscess or discharging sinus formation, particularly after large core needle biopsies.
With the increasing use of FNAC as the initial investigation for breast lesions, more cases will probably be encountered by the cytopathologist, necessitating an increased awareness of this disease entity.
Among the only three large series describing the FNAC features of GM in the literature, the usefulness of FNAC in GM has been debated, with some authors confirming the useful role of FNAC,10,11 whereas others have concluded that the various causes of granulomatous inflammation cannot be confidently differentiated by FNAC.9
The diagnostic cytological criteria for GM remain poorly defined, and the common features that have been evaluated include necrosis, giant cells, epithelioid histiocytes, granulomas, and neutrophils present in the background.
In our study, most cases showed single epithelioid histiocytes present within the smears and this should alert the cytopathologist to the possibility of a granulomatous inflammation. The appearance of these histiocytes was distinct, with reniform to plump nuclei and a moderate to abundant pale pink cytoplasm. This appears to be a common feature, having been reported in all cases of GM in the literature.9–12,15–18 Most studies reported aggregates of epithelioid histiocytes or granulation tissue fragments, probably representing granulomas which are characteristic of GM. In our series, granulomas were present in only half of the cases, and their presence is therefore suggestive but not pathognomonic for GM.
Take home messages.
The cytological diagnosis of granulomatous mastitis (GM) is difficult because the features overlap with other aetiologies, including tuberculosis, and there are no specific features
The absence of necrosis and a predominantly neutrophilic infiltrate in the background favour a diagnosis of GM
A diagnosis of GM should also be considered when high numbers of epithelioid histiocytes are seen in smears, even in the absence of granulomas
The definitive diagnosis of GM relies on histology of fine needle biopsies and negative microbiological investigations
The presence of other inflammatory cells was more variable. In our series, there was an overwhelming predominance of neutrophils over lymphocytes. This finding was similar to that of another study of nine cases, which demonstrated moderate to abundant numbers of neutrophils in the FNAC preparations.10 Most other reports have described a mixed inflammatory cell infiltrate.
Another characteristic FNAC feature was the absence of caseous necrosis in the background. This is particularly important in the differentiation from an infective cause of granulomatous inflammation.
“In our series, granulomas were present in only half of the cases, and their presence is therefore suggestive but not pathognomonic for granulomatous mastitis”
The single most important differential diagnosis of GM is tuberculosis, which remains endemic in many regions. Treating tuberculosis with steroids would aggravate the infection, whereas giving unnecessary antituberculosis drugs may cause numerous side effects. In tuberculosis mastitis, the common features include epithelioid histiocytes, Langhan’s giant cells, granulomas, and caseous necrosis. The presence of neutrophils is not a common feature unless there is concomitant suppuration. Thus, there is considerable overlap because epithelioid histiocytes, giant cells, and granulomas are common to both entities. The presence of predominantly neutrophils in the background, and the lack of caseous necrosis may favour a diagnosis of GM rather than tuberculosis. Other differential diagnoses are rare specific causes of granulomatous inflammation, including fungal infection or non-infectious causes, such as sarcoidosis or Wegener’s granulomatosis. Because GM is essentially a diagnosis of exclusion, all causes of granulomatous inflammation must be actively excluded. An FNAC diagnosis of GM cannot be made easily, and a confident diagnosis may require histological samples, negative microbiological investigations, and clinical correlation.
In our study, we found that the most common cytological feature of GM was the presence of epithelioid histiocytes, followed by the presence of predominantly neutrophils in the background, multinucleated giant cells, and granulomas. The absence of caseation was also important. Although there is considerable overlap with tuberculosis, the absence of caseation and the presence of mostly neutrophils may favour a non-infective aetiology. It is also of interest to note that the presence of granulomas and giant cells tends to correlate with the cellularity of the epithelioid histiocytes in the FNAC preparation. Thus, in a suboptimal or low cellularity aspirate, granulomas or giant cells may be absent, and the cytopathologist should be alerted to the possibility of GM if epithelioid histiocytes are seen.
Abbreviations
FNAC, fine needle aspiration cytology
GM, granulomatous mastitis
H&E, haematoxylin and eosin
PCR, polymerase chain reaction
REFERENCES
- 1.Kessler E, Woolloch Y. Granulomatous mastitis: a lesion clinically simulating carcinoma. Am J Clin Pathol 1972;58:642–6. [DOI] [PubMed] [Google Scholar]
- 2.Fletcher A, Magrath IM, Riddell RH, et al. Granulomatous mastitis: a report of seven cases. J Clin Pathol 1982;35:941–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Going JJ, Anderson TJ, Wilkinson S, et al. Granulomatous lobular mastitis. J Clin Pathol 1987;40:535–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Galea MH, Robertson JF, Ellis IO, et al. Granulomatous lobular mastitis. Aust N Z J Surg 1989;59:547–50. [DOI] [PubMed] [Google Scholar]
- 5.Bhaskaran CS, Prasad KR, Rao G, et al. Chronic granulomatous mastitis: review of 26 cases with special reference to chronic lobular mastitis. Indian J Pathol Microbiol 1992;35:38–43. [PubMed] [Google Scholar]
- 6.Engin G, Acunas G, Acunas B. Granulomatous mastitis: gray scale and color Doppler sonographic findings. J Clin Ultrasound 1999;27:101–6. [DOI] [PubMed] [Google Scholar]
- 7.Han BK, Choe YH, Park JM, et al. Granulomatous mastitis: mammographic and sonographic appearances. AJR Am J Roentgenol 1999;173:317–20. [DOI] [PubMed] [Google Scholar]
- 8.Yilmaz E, Lebe B, Usal C, et al. Mammographic and sonographic findings in the diagnosis of idiopathic granulomatous mastitis. Eur Radiol 2001;11:2236–40. [DOI] [PubMed] [Google Scholar]
- 9.Martinez-Parra D, Nevado-Santos M, Melendez-Guerrero B, et al. Utility of fine-needle aspiration in the diagnosis of granulomatous lesions of the breast. Diagn Cytopathol 1997;17:108–14. [DOI] [PubMed] [Google Scholar]
- 10.Kumarasinghe MP. Cytology of granulomatous mastitis. Acta Cytol 1997;41:727–30. [DOI] [PubMed] [Google Scholar]
- 11.Yip CH, Jayaram G, Swain M. The value of cytology in granulomatous mastitis: a report of 16 cases from Malaysia. Aust N Z J Surg 2000;70:103–5. [DOI] [PubMed] [Google Scholar]
- 12.Macansh S, Greenberg M, Barraclough B, et al. Fine needle aspiration cytology of granulomatous mastitis. Report of a case and review of the literature. Acta Cytol 1990;34:761–2. [PubMed] [Google Scholar]
- 13.Page DL, Anderson TJ. Diagnostic histopathology of the breast. Edinburgh: Churchill Livingstone, 1987.
- 14.Ellis IO, Elston CW, Goulding H. Inflammatory conditions. In: Elston CW, Ellis IO, eds. Systemic pathology, Vol. 13, 3rd ed. The breast. Edinburgh: Churchill Livingstone, 2000:192–5.
- 15.Poniecka AW, Krasuski P, Gal E, et al. Granulomatous inflammation of the breast in a pregnant woman: report of a case with fine needle aspiration diagnosis. Acta Cytol 2001;45:797–801. [DOI] [PubMed] [Google Scholar]
- 16.Kaur AC, Dal H, Muezzinoglu B, et al. Idiopathic granulomatous mastitis. Report of a case diagnosed with fine needle aspiration cytology. Acta Cytol 1999;43:481–4. [DOI] [PubMed] [Google Scholar]
- 17.Kobayashi TK, Sugihara H, Kato M, et al. Cytologic features of granulomatous mastitis. Report of a case with fine needle aspiration cytology and immunocytochemical findings. Acta Cytol 1998;42:716–20. [DOI] [PubMed] [Google Scholar]
- 18.Anastasiadis P, Koutlaki N, Liberis V, et al. Cytomorphologic features of nonspecific granulomatous mastitis diagnosed by imprint cytology. Acta Cytol 2001;45:887–9. [DOI] [PubMed] [Google Scholar]