Abstract
Background: The clinical and prognostic significance of “inadequate” cervical smear is unknown, even though women with repeated inadequate smears are referred for colposcopy in the National Health Service (NHS) Cervical Screening Programme.
Aim: To follow up a cohort of women with inadequate cervical smears over the following five years to examine outcomes, including detection of high grade cervical intraepithelial neoplasia (CIN).
Methods: The study comprised 1972 women with an inadequate cervical smear reported at Walsall Hospitals NHS Trust between 1 April 1995 and 31 March 1996. Results of cervical smears and biopsies taken over the following five years were reviewed to confirm the outcome.
Findings: Within five years, 2.2% of women with an inadequate cervical smear developed histologically confirmed high grade CIN, which was higher than the 1.3% seen among all women with cervical smear tests reported at the same laboratory over the same period, although the difference was not significant at the 95% level of confidence. Where inadequacy resulted from or was contributed to by “polymorphs obscuring”, the risk of subsequent development/detection of high grade CIN was 2.6%.
Conclusions: Women with inadequate cervical smears had an increased risk of detection of high grade CIN in the following five years compared with “all women”. This increased risk was not significant, although if a larger number of women had been studied significance may have been reached, so that further studies are needed. The increased risk appeared to be at least partially dependent on the reason for inadequacy.
Keywords: National Health Service Cervical Screening Programme, cervical intraepithelial neoplasia, inadequate cervical smears, Papanicolaou smear
The National Health Service Cervical Screening Programme (NHSCSP) aims to reduce mortality and morbidity from cervical cancer,1 and has achieved over 80% coverage since 1992.2 The incidence of cervical cancer fell by 26% between 1992 and 1997 and the death rate is falling by 7% each year.3,4 These figures suggest that the NHSCSP is having a successful impact.
“Our study was established to obtain robust follow up information on a large cohort of women with an inadequate smear to identify patterns in subsequent cytology over a five year period”
However, inadequate smears pose a major problem for the NHSCSP, constituting a large proportion of cervical smears. Many laboratories failed to meet the standard for inadequate smear rates in the original guidance from the NHSCSP,5 resulting in revised standards being issued, in which the acceptable range for inadequate smear rates was increased.6 The NHSCSP guidance requires referral for colposcopy for a woman with three consecutive inadequate smears,6 although no scientific basis for this guidance is yet available. A small number of UK studies have suggested that unnecessary colposcopy could be avoided for many patients if repeat smears were performed.7,8 However, these studies involved small numbers of women, and conclusions were drawn after colposcopy and/or biopsy without an appreciable follow up period. Other studies have linked smear quality with abnormality detection, suggesting that poorly taken smears might contribute to false negative results.9,10 Our study was established to obtain robust follow up information on a large cohort of women with an inadequate smear to identify patterns in subsequent cytology over a five year period.
METHODS
The cytology department of Walsall Hospitals NHS Trust serves a population of approximately 253 020 within the Walsall Metropolitan Borough. The laboratory received 25 446 cervical (Papanicolaou) smears between 1 April 1995 and 31 March 1996. These smears were mainly from women of cervical screening age (20–64 years), with a few outliers. All women who had a smear reported as “inadequate” in this period were included in our study group. Inadequate smears were classified according to the reason for inadequacy, using categories recommended by the NHSCSP at the time,5 as follows:
Insufficient cellularity (too few squames).
Poor fixation.
More than 50% of cellular material obscured by blood, polymorphs, or bacteria (these three groups were considered separately).
Too thickly spread smear.
Where more than one reason for inadequacy was found the smear was categorised as “multiple reason”.
All these women were followed up for five years. This was so that they had the opportunity of having two negative smears, because we operate three year recall intervals.
Follow up cytology and histology results were retrieved from the laboratory computer system. Where the laboratory computer system did not provide adequate information (that is, patients lost to follow up), the health authority computer system was used to obtain follow up information.
In accordance with the national guidelines, those with three consecutive inadequate smears, at least two low grade abnormal smears, and one high grade abnormal smear were referred for colposcopy, where biopsies and/or smears were taken.
The subsequent worst abnormality detected was subdivided into three categories, as follows:
Smear abnormality only without colposcopic biopsy/histological confirmation.
Low grade cervical intraepithelial neoplasia (CIN; colposcopically and histologically confirmed CIN I).
High grade CIN (colposcopically and histologically confirmed CIN II, III, or worse).
FINDINGS
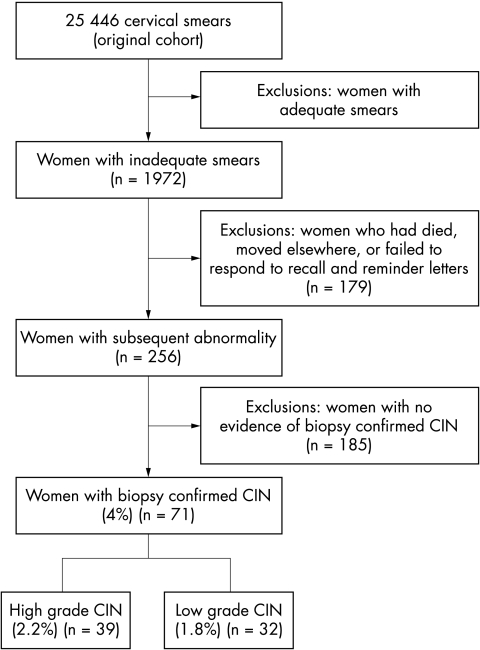
Between 1 April 1995 and 31 March 1996, 25 446 cervical smear reports were issued by the laboratory. Of these, 2150 (8.5%) were reported as inadequate, a rate within the national standard range (5–9%).5 Of the 2150 inadequate reports, 68 were for non-cytological reasons, including request forms received without a smear, or slides that were broken beyond repair being received. Excluding these, 2082 inadequate smears were reported from a total of 25 378 (8.2%). These included a mixture of first, second, and third consecutive inadequate smears, and these related to 1972 women (fig 1). Table 1 categorises the reasons for inadequacy. In the study population, there were 14 women who had a high grade abnormal smear (moderate dyskaryosis or worse) immediately following an inadequate smear (0.7%). In these cases, all the preceding inadequate smears were reviewed by senior cytology staff, and were confirmed to contain no abnormal (dyskaryotic) cells.
Figure 1.
Schematic overview of study design. Outcome of women with inadequate cervical smears followed up for five years in the Walsall district.
Table 1.
Categories of inadequate smears, their mean age and subsequent cervical pathology detected within 5 years
| Inadequate category | Number (A) | Mean age (in years) | No. (%) of abnormal smears, without confirmed CIN at colposcopy and histology | No. (%) of CIN I at colposcopy and histology | No. (%) of CIN II and CIN III at colposcopy and histology | No. lost to follow up (B) | No. of inadequates corrected for non-responders (A−B) | No. (%) reaching CIN II or more at colposcopy and histology (corrected for lost to follow up) |
| Multiple reasons | 305 | 38 | 32 (10.49) | 7 (2.30) | 8 (2.62) | 28 | 277 | 8 (2.89) |
| Poor fixation | 389 | 40.4 | 31 (7.97) | 4 (1.03) | 9 (2.31) | 42 | 347 | 9 (2.59) |
| Obscured by blood | 265 | 38.46 | 35 (13.2) | 3 (1.13) | 6 (2.26) | 21 | 244 | 6 (2.46) |
| Obscured by polymorphs | 290 | 38.2 | 34 (11.72) | 9 (3.1) | 6 (2.07) | 21 | 269 | 6 (2.23) |
| Too few squames | 383 | 40.65 | 28 (7.31) | 4 (1.04) | 6 (1.57) | 30 | 353 | 6 (1.70) |
| Too thick | 210 | 36.16 | 13 (6.19) | 3 (1.43) | 3 (1.43) | 14 | 196 | 3 (1.53) |
| Cytolysis/obscured by organisms | 130 | 31.8 | 12 (9.23) | 2 (1.54) | 1 (0.77) | 23 | 107 | 1 (0.93) |
| Total | 1972 | 37.67 | 185 (9.38) | 32 (1.62) | 39 (1.98) | 179 | 1793 | 39 (2.18) |
CIN, cervical intraepithelial neoplasia.
The mean age of women with inadequate smears was 37.7 years, and there were no obvious age differences across the different inadequate categories. A total of 256 women (12.9%) developed abnormalities during follow up. One hundred and eighty five (9.4%) had a smear abnormality only (borderline smear or worse), without histologically confirmed CIN. Seventy one (3.6%) developed histologically confirmed CIN, 32 with low grade CIN (1.6%), and 39 (1.9%) with high grade CIN. High grade CIN for each of the categories of inadequacy varied from 0.8% to 2.6%. Of the 1972 patients with inadequate smears, 179 were lost to follow up, including women who had moved elsewhere, had died, or had failed to respond to repeated recall and reminder letters (fig 1). After correction for “lost to follow up” patients, 2.2% of women with inadequate smears developed histologically confirmed high grade CIN within the five year follow up period. Although higher than the overall rate of detection of high grade abnormalities for the laboratory, which was 1.3%, this difference failed to reach significance.
There was variation in the likelihood of reporting a high grade CIN depending on the reason for inadequacy, from 2.6% for “multireason” to 0.8% for “cytolysis/obscured by organisms”. The category “multiple reason for inadequacy” was subcategorised according to the constituent reasons, and each subcategory considered together with the related single reason category (table 2). Within the “multiple reason” category, where reasons included “obscured by polymorphs” there was a high rate of development of high grade CIN (3.25%). Overall, 23.2% of inadequate smears were associated with obscuring by polymorphs, and these cases had a 2.6% risk of development of high grade CIN within five years. Once again, this higher rate was not significantly different from the overall high grade abnormality rate of 1.3%.
Table 2.
Subcategorisation within the multiple reasons category, and the subsequent risks of development/detection of high grade CIN, considered in conjunction with related single reason categories
| Category | Number in category (A) | % Of total inadequate smears (of 1972) | No. of high grade CIN at colposcopy and histology | % Of high grade CIN at colposcopy and histology within each category | No. lost to follow up (B) | No. of inadequates corrected for non-responders (A−B) | Number (%) high grade CIN at colposcopy and histology within each category corrected for lost to follow up |
| Multiple reasons | 305 | 15.47 | 8 | 2.62 | 28 | 277 | 8 (2.89%) |
| Multiple reasons, including obscured by polymorphs | 168 | 8.52 | 5 | 2.98 | 14 | 154 | 5 (3.25%) |
| Obscured by polymorphs (single reason) | 290 | 14.71 | 6 | 2.07 | 21 | 269 | 6 (2.23%) |
| Multiple reasons (including obscured by polymorphs) and single reason category obscured by polymorphs combined | 458 | 23.23 | 11 | 2.40 | 35 | 423 | 11 (2.60%) |
| Multiple reasons (including obscured by blood) | 105 | 5.32 | 1 | 0.95 | 10 | 95 | 1 (1.05%) |
| Obscured by blood (single reason category) | 265 | 13.44 | 6 | 2.26 | 21 | 244 | 6 (2.46%) |
| Obscured by blood (single reason category) and multiple reasons (including obscured by blood) | 370 | 18.76 | 7 | 1.89 | 31 | 339 | 7 (2.06%) |
| Multiple reasons (with polymorphs or blood) (single reason) obscured by blood − (single reason) obscured by polymorphs combined | 764 | 38.74 | 17 | 2.23 | 60 | 704 | 17 (2.41%) |
CIN, cervical intraepithelial neoplasia.
DISCUSSION
The NHSCSP recommends a detection rate for high grade CIN of between 1.2% and 2.0%. It appears that inadequate smears caused by “multiple reason”, “obscured by blood”, or “obscured by polymorphs” had a higher rate of high grade CIN than would be expected. Those inadequate smears with “cytolysis/obscured by organisms” had a lower incidence. Overall, 1.3% of all smears reported at Walsall Hospitals NHS Trust in the study period were found to have high grade abnormalities. All the inadequate categories, with the exception of the “cytolysis/obscured by organisms” category, exceeded this figure. Inadequates caused by “poor fixation” were excluded from further analysis, because this is an avoidable technical problem, unlike other causes for inadequacy.
Cervical smear inadequate rates are higher in the UK than elsewhere.11 This may be a result of the different criteria used by the NHSCSP, and may also reflect the longer screening interval in the UK.12 The NHSCSP recognises inadequate smears as a major problem, being one of the main reasons for piloting liquid based cytology for primary screening in England and Wales. The clinical and prognostic significance of inadequate cervical smears is uncertain, and the NHSCSP guidance requiring women with repeated inadequate cervical smears to be referred for colposcopy has been questioned.7,8 Colposcopy departments across the UK are struggling to meet the nationally recommended colposcopy waiting times, and referrals for repeated inadequate smears contribute to this problem.
Our study demonstrated an increased risk of detection of high grade CIN within five years of an inadequate smear. However, this increased risk was not significant, although it is possible that had a larger cohort of women been studied, significance would have been reached, and further studies should be carried out to explore this issue. We used a five year follow up period for our study because this is the current recommended minimum screening interval for women aged 20–64 in the UK, even though many health authorities including our own operate three year recall system. Our findings are supportive of current national guidelines requiring repeated inadequate cervical smears to be referred for colposcopy. However, these guidelines do not take into consideration the reason for inadequacy. Our results suggest that there may be an association between the reason for inadequacy and the subsequent risk of detection of high grade CIN. Although the NHSCSP requires cytology laboratories to report the reason for inadequacy,6 this is purely to serve the audit and educational requirements of the smear takers.
“Our study supports the current guidelines for colposcopy in women with repeated inadequate smears by demonstrating a higher risk of detection of high grade cervical intraepithelial neoplasia”
Our findings suggest that the increased risk was partially dependent on the reason for inadequacy. There is no increased risk of development of high grade CIN if the inadequacy results from “cytolysis/obscured by organisms”. However, if the inadequacy of the smear is caused by other reasons, the risk of detection of high grade CIN appears to be higher than that seen in the general population. This risk appears to be highest when the inadequacy is caused by or contributed to by “obscured by polymorphs”. A limitation of our study is the subjective nature of identifying smear adequacy, which may vary from one screener to another and from one laboratory to the next. However, a European multicentre study showed a high level of agreement among cytologists as to what constitutes an inadequate smear.13
Another limitation of our study was the inability to correlate the clinical signs and symptoms (if there are any) with colposcopic findings. This is because such findings are not consistently recorded or are not given to the cytology laboratory.
Although our study was performed in a single centre, the findings are probably applicable to other cytology laboratories in England and Wales. Despite initial optimism that liquid based cytology would significantly reduce inadequate smear rates, there is little evidence to support this. There are some concerns that liquid based cytology might falsely label inadequate smears as negative, and such an adverse effect would take several years to become evident in a programme with a three to five year screening interval.12 Health technology assessment reports from New Zealand and Australia also concluded that the introduction of liquid based cytology was not justified by current evidence.14,15 Thus, the problem of “inadequate cervical smear” will probably stay with us for some time, and it is important to understanding fully its clinical and prognostic significance.
In conclusion, our study supports the current guidelines for colposcopy in women with repeated inadequate smears by demonstrating a higher risk of detection of high grade CIN. It also suggests that colposcopy may not be necessary in a subset of inadequate cervical smears. Because we are required to practice evidence based medicine, the way forward in our opinion would be for the NHSCSP to study the outcome (if possible nationally) of inadequate cervical smears, and to formulate its guidelines for further management based upon the evidence.
Take home messages.
Women with inadequate cervical smears had an increased risk of detection of high grade cervical intraepithelial neoplasia in the five years following the inadequate smear when compared with the total number of women screened (2.2% v 1.3%)
This increased risk was not significant, but if a larger number of women had been studied significance may have been reached, so that further studies are needed to clarify this issue
The increased risk appeared to be at least partially dependent on the reason for inadequacy, with the highest risk being seen when inadequacy is caused by or contributed to by “obscured by polymorphs”
Acknowledgments
We are grateful to Mrs A Turner and Miss S Morris for typing the manuscript; Ms P Pearmain, Deputy QA Director, West Midlands Cervical Screening QA office for her helpful comment on the manuscript; Dr C Livings, Information Manager, West Midlands Cancer Intelligence Unit and C Harris, Medical Student, University of Nottingham for their statistical advice and analysis; Mrs B Hill for generating relevant data from the computer system; and also Mrs J Brown for reviewing smears. The study was funded by the West Midlands Cervical Screening Quality Assurance Reference Centre. It has no involvement in study design, data collection and analysis, in the writing of the report, or in the decisions to submit the paper for publication.
Abbreviations
CIN, cervical intraepithelial neoplasia
NHSCSP, National Health Service Cervical Screening Programme
REFERENCES
- 1.Patnick J, ed. Cervical Screening Programme: review 1998. A national priority. Sheffield: NHSCSP, 1998.
- 2.Department of Health. Department of Health Statistical Bulletin, Cervical Screening Programme, England: 1995–96. London: Department of Health, 1996, 1997, 1998, 1999, 2000.
- 3.Office for National Statistics. Estimates of newly diagnosed cases of cancer England and Wales 1993–97. London: Office for National Statistics. 1998 ONS Monitor MB1 98/2.
- 4.Sasieni P, Cuzick J, Farmery E. Accelerated decline in cervical cancer mortality in England and Wales. Lancet 1995;346:1566–7. [DOI] [PubMed] [Google Scholar]
- 5.Herbert A. Achievable standards. Benchmarks for reporting and criteria for evaluation cervical cytopathology. Sheffield: NHSCSP, 1995. [DOI] [PubMed]
- 6.Johnson J, Patrick J. Achievable standards. Benchmarks for reporting and criteria for evaluation cervical cytopathology, 2nd ed. Sheffield: NHSCSP, 2000.
- 7.Sen C, Brett MT. Outcome of women referred to colposcopy for persistently inadequate smears. Cytopathology 2000;11:38–44. [DOI] [PubMed] [Google Scholar]
- 8.Hollingworth J, Koteeha K, Dobbs SP, et al. Cervical disease in women referred to colposcopy following inadequate smears. Cytopathology 2000;11:45–52. [DOI] [PubMed] [Google Scholar]
- 9.Henry JA, Wadehra V. The influence of smear quality on the rate of detection of significant cervical cytological abnormalities. Acta Cytol 1996;40:529–35. [DOI] [PubMed] [Google Scholar]
- 10.Williamson SLM, Hair T, Wadehra V. The effects of different sampling techniques on smear quality and the diagnosis of cytological abnormalities in cervical screening. Cytopathology 1997;8:188–95. [DOI] [PubMed] [Google Scholar]
- 11.National Institute for Clinical Excellence. Guidance on the use of liquid-based cytology for cervical screening. Technology appraisal guidance No. 5. London: National Institute for Clinical Excellence, 2000.
- 12.Herbert A, Johnson T. Personal view. Is it reality or an illusion that liquid-based cytology is better than conventional cervical smears? Cytopathology 2001;12:383–9. [DOI] [PubMed] [Google Scholar]
- 13.Ciatto S, Carvogop MP, Minuti AP, et al. Interlaboratory reproducibility in reporting inadequate cervical smears—a multi-centre multinational study. Cytopathology 1996;7:386–90. [DOI] [PubMed] [Google Scholar]
- 14.Broadstock M. New Zealand health technology assessment (NZHTA) report, Vol. 3, No. 1: Effectiveness and cost-effectiveness of automated and semi-automated cervical screening devices. 2000. (available from http://nzhta.chmeds.ac.uk).
- 15.Australian Health Technology Advisory Committee. Review of automated and semi-automated cervical screening devices. Canberra: Development of Health and Family Services, 1998.