Abstract
Background: Lymphovascular space invasion (LVSI) is an important step in the complex process of tumour metastasis. Various methods have been used in the past to improve the histological detection of LVSI.
Aims: To develop a sensitive immunohistochemical method for the detection of LVSI.
Methods: Paraffin wax blocks from 108 patients who had undergone hysterectomy for stage I endometrial cancer were retrieved. Dual immunostaining for pancytokeratin and the CD31 endothelial cell marker was carried out on 4 μm sections cut from these bocks and compared with conventional haematoxylin and eosin staining.
Results: The detection rate for LVSI increased threefold compared with conventional haematoxylin and eosin staining in the test group.
Conclusion: This finding suggests that LVSI is a much more common phenomenon than previously thought and questions current understanding of tumour metastasis.
Keywords: CD31, cytokeratin, invasion, lymphatic, vascular
Cells that have acquired invasive potential must invade the host stromal tissue before local invasion. This is followed by sequestration through endothelial paracellular clefts into lymphovascular spaces. Theoretically, once lymphovascular space invasion (LVSI) has occurred, tumour cells have the potential to metastasise to regional lymph nodes or distant sites. The histological detection of LVSI has been shown to correlate positively with regional lymph node metastasis, higher recurrence rate, and decreased survival time.1
Currently, the standard method for assessing LVSI is light microscopic examination of haematoxylin and eosin (H&E) stained sections. Microscopic detection of LVSI depends on identifying tumour cells within a confined space lined by endothelial cells and has three important limitations. First, tumour cells within lymphovascular spaces may evade detection on H&E staining if they are present in very small numbers, surrounded by a greater number of circulating cells, or have been trapped within a fibrin clot (fig 1). Second, it is often difficult to differentiate tumour cells that completely fill up a lymphovascular space from stromal invasion. Finally, artifactual tissue retraction around tumour islands complicates the identification of true LVSI. Immunostaining for various endothelial cell markers has been used in the past to overcome the last two problems in the detection of LVSI. The limited ability of H&E staining to identify isolated tumour cells has also been overcome by using immunohistochemistry (IHC) for various markers, including epithelial cell constituents, such as cytokeratins. However, this has only been reported in sites other than lymphovascular spaces.2
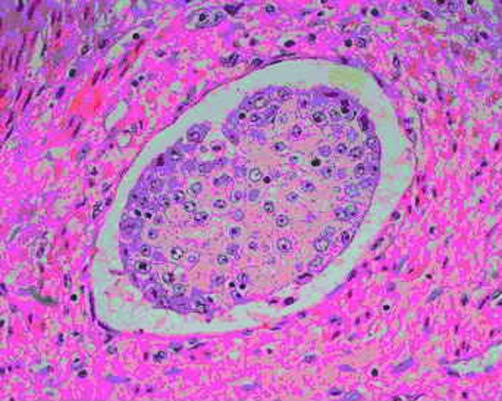
Figure 1.
Tumour cells within confined vascular space; endothelial cells are inconspicuous (haematoxylin and eosin stained; original magnification, ×40).
“The histological detection of lymphovascular space invasion has been shown to correlate positively with regional lymph node metastasis, higher recurrence rate, and decreased survival time”
We hypothesised that adenocarcinoma cells within lymphovascular spaces could be readily identified if epithelial and endothelial cell markers were used simultaneously. Therefore, we examined whether dual staining for cytokeratin and an endothelial marker, CD31, improved the detection of LVSI in comparison with conventional H&E staining in a group of patients with stage I endometrial cancer (EC). We used EC as a model because LVSI is an important prognostic feature in this cancer.
METHODS
The H&E sections of 108 patients who underwent total abdominal hysterectomy as their initial treatment for clinically staged stage I EC were reviewed. A single representative paraffin wax block containing the deepest portion of the tumour and the underlying myometrium was selected from each patient. Sections (4 μm thick) were cut from each block and adjacent sections were stained with standard H&E and dual immunohistochemical staining for cytokeratin and CD31. Pancytokeratin staining was by the streptavidin–biotin peroxidase method using a 1/50 dilution of mouse monoclonal antikeratin clone AE1/AE3 (0.165 μg/ml) (Zymed Laboratories, San Francisco, California, USA) and the Vectastatin ABC system (Vector Laboratories, Burlingame, California, USA). The colour was developed using 3,3-diaminobenzidine tetrahydrocholoride in phosphate buffered saline. Endothelial cells on the same section were immunostained with a 1/50 dilution of monoclonal mouse antihuman CD31 endothelial cell marker (0.45 μg/ml) (Dako Corporation, Carpenteria, California, USA) and the colour was developed using the VIP substrate kit (Vector Laboratories). The section was then counterstained with methyl green (Vector Laboratories). All the slides were examined independently by two pathologists and their findings were in concordance (κ = 1). On H&E sections, LVSI was considered positive when tumour emboli were noted within a space clearly lined by endothelial cells. In dually stained sections, LVSI was recorded as present when any number of tumour cells was noted within a lymphovascular space delineated by CD31 positive endothelial cells (fig 2).
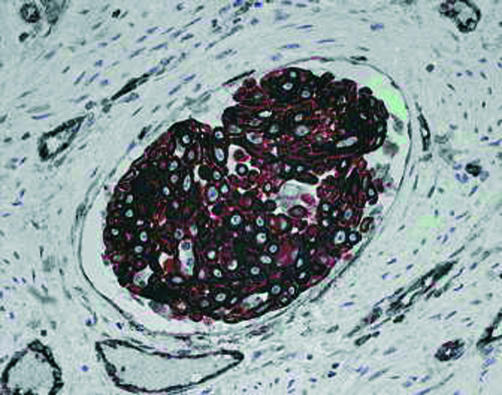
Figure 2.
Tumour lymphovascular space invasion detected after pancytokeratin and CD31 immunostaining (immunohistochemistry; original magnification, ×40)
RESULTS
LVSI was present in 17 of 108 cases (16%) by H&E, of which 15 were confirmed by IHC and two were found to be negative by IHC. This incidence rate is consistent with the reported rate in the literature.3 In four cases, LVSI was deemed “probable” on H&E sections, but this was only confirmed by IHC in two cases (table 1). In the remaining 87 cases (80%) H&E detected no evidence of LVSI. However, IHC showed the presence of LVSI in 41 (38%) of these 87 H&E negative cases. Overall, LVSI was present in 58 cases (54%) and absent in 50 cases (46%) on IHC, as compared with 21 (17%) and 87 (81%) cases, respectively, on H&E (table 1). The detection rate of LVSI by dual IHC significantly exceeds the conventional H&E method (Fisher exact test, p < 0.001).
Table 1.
The frequency of lymphovascular space invasion identified by conventional H&E staining compared with dual immunostaining for CK and CD31
| CD31 and CK staining | |||
| H&E staining | Present | Absent | Total |
| Present | 15 (14%) | 2 (1.8%) | 17 (16%) |
| “Probable” | 2 (2%) | 2 (2%) | 4 (4%) |
| Absent | 41 (38%) | 46 (43%) | 87 (80%) |
| Total | 58 (54%) | 50 (46%) | 108 |
CK, pancytokeratin; H&E, haematoxylin and eosin.
Take home messages.
The detection rate for lymphovascular space invasion (LVSI) increased threefold compared with conventional haematoxylin and eosin staining in patients with stage I endometrial cancer
LVSI may be a much more common phenomenon than previously thought and this questions our current understanding of tumour metastasis
Further studies are needed to establish the clinical relevance of this finding
DISCUSSION
Metastasis is fundamentally an embolic process. It may be viewed as a series of events that occur sequentially, with invasion of lymphovascular channels as an important early stage. Once the malignant cells have accessed the lymphovascular space they can grow along the lumen and permeate the lymphatic drainage in that area, or disseminate more widely. Therefore, LVSI has been regarded as an important predictive factor of nodal metastases and recurrent disease in various solid tumours.4,5
“We noted a significant rise amounting to a threefold increase in the detection rate of lymphovascular space invasion by using the dual immunostaining technique”
Ours is the first study to report the use of dual immunostaining to identify tumour cells within the lymphovascular space using pancytokeratin and endothelial cell markers. There have been many attempts in the past to improve the detection rate of LVSI. Single immunostaining for factors including factor VIII, CD31, and podoplanin have all led to an increase in the detection rate of LVSI, but have failed to reach significance.6–8 In addition, combinations of the above factors have also been used to improve the detection of LVSI and to distinguish lymphatic from blood vessel invasion. In cervical carcinoma, Birner et al reported an LVSI detection rate of 47% (46 of 98) using both factor VIII and podoplanin immunostaining. However, the detection rate (47% v 34%) was not significantly different from that with H&E staining.8 More specifically, in endometrial cancer immunostaining with antibodies for von Willebrand factor and blood group isoantigens was used by Tsuruchi et al.9 They similarly reported no significant increase in the detection rate in comparison with conventional H&E. In only two of 62 of their cases where H&E had failed to detect LVSI did IHC positively identify LVSI. In contrast, in our study we noted a significant rise amounting to a threefold increase in the detection rate of LVSI (54% v 18%) by using the dual immunostaining technique (p < 0.001). Although this increased detection rate establishes the improved sensitivity of IHC over H&E staining in the detection of LVSI, further studies are needed to establish the clinical relevance of this finding. The high percentage of LVSI detected by this technique suggests that it may be overly sensitive in picking up either very low levels of circulating tumour cells or those that are carried over into vascular spaces during specimen handling and sectioning, neither of which may have the same adverse implications as LVSI detected by conventional methods. Certainly, the technique is recommended for identifying cases of LVSI that are doubtful on H&E staining.
We hope that these preliminary results will encourage further application of this inexpensive, readily available technique on other solid tumours to corroborate the clinical value of LVSI.
Abbreviations
EC, endometrial cancer
H&E, haematoxylin and eosin
IHC, immunohistochemistry
LVSI, lymphovascular space invasion
REFERENCES
- 1.Inoue Y, Obata K, Abe K, et al. The prognostic significance of vascular invasion by endometrial carcinoma. Cancer 1996;78:1447–51. [DOI] [PubMed] [Google Scholar]
- 2.Yabushita H, Shimazu M, Yamada H, et al. Occult lymph node metastases detected by cytokeratin immunohistochemistry predict recurrence in node-negative endometrial cancer. Gynecol Oncol 2001;80:139–44. [DOI] [PubMed] [Google Scholar]
- 3.Gal D, Recio FO, Zamurovic D, et al. Lymphovascular space involvement, a prognostic indicator in endometrial adenocarcinoma. Gynecol Oncol 1991;42:142–5. [DOI] [PubMed] [Google Scholar]
- 4.Comerci G, Bolger BS, Flannelly G, et al. Prognostic factors in surgically treated stage IB–IIB carcinoma of the cervix with negative lymph nodes. Int J Gynecol Cancer 1998;8:23–6. [DOI] [PubMed] [Google Scholar]
- 5.Paladini D, Cross P, Lopes A, et al. Prognostic significance of lymph node variables in squamous cell carcinoma of the vulva. Cancer 1994;74:2491–6. [DOI] [PubMed] [Google Scholar]
- 6.Obermair A, Wanner C, Bilgi S, et al. The influence of vascular space involvement on the prognosis of patients with stage IB cervical carcinoma: correlation of results from hematoxylin and eosin staining with results from immunostaining for factor VIII-related antigen. Cancer 1998;82:689–96. [PubMed] [Google Scholar]
- 7.Schoppmann SF, Birner P, Studer P, et al. Lymphatic microvessel density and lymphovascular invasion assessed by anti-podoplanin immunostaining in human breast cancer. Anticancer Res 2001;21(4A):2351–5. [PubMed] [Google Scholar]
- 8.Birner P, Obermair A, Schindl M, et al. Selective immunohistochemical staining of blood and lymphatic vessels reveals independent prognostic influence of blood and lymphatic vessel invasion in early-stage cervical cancer. Clin Cancer Res 2001;7:93–7. [PubMed] [Google Scholar]
- 9.Tsuruchi N, Kaku T, Kamura T, et al. The prognostic significance of lymphovascular space invasion in endometrial cancer when conventional hematoxylin and eosin staining is compared to immunohistochemical staining. Gynecol Oncol 1995;57:307–12. [DOI] [PubMed] [Google Scholar]