Measurement of urine osmolality and urine sodium is often advocated in the evaluation of severe hyponatraemia. In a recent article in the Journal of Clinical Pathology, Saeed and colleagues documented the frequency with which these investigations were performed.1 However, the results of urine biochemistry obtained in the assessment of severe hyponatraemia are rarely reported.2
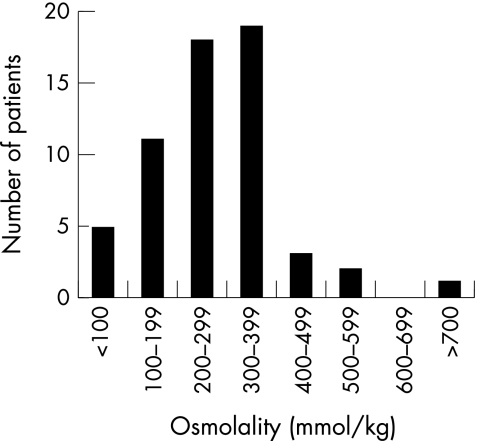
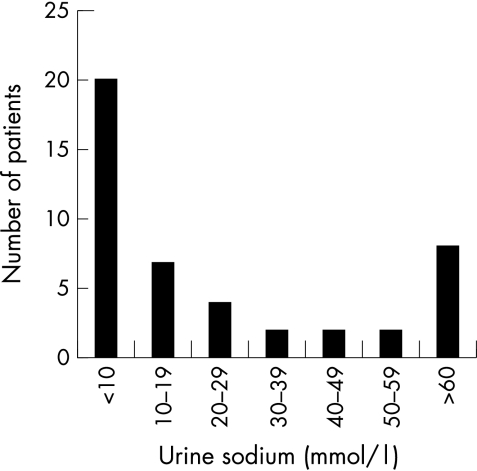
We examined the computer records of 59 patients (44 women, 15 men; age range, 22–93 years) found in 2002 to have a serum sodium of less than 120 mmol/litre, in whom a urine osmolality was requested at around the same time (the total number of patients with a serum sodium of less than 120 mmol/litre during the same period was 304). Case notes were available for 34 of these patients. Figures 1 and 2 show the results of urine osmolality and sodium measurement, respectively. Serum osmolality confirmed a hypo-osmolal state in 41 of the 45 patients in whom it was measured. Of the four patients in whom a hypo-osmolal state was not confirmed, three were uraemic and one was hyperglycaemic. Cortisol was measured, either randomly or as part of a short synacthen test, in 28 patients; it was greater than 560 nmol/litre in all but two, both of whom had secondary adrenal insufficiency, one as a result of treatment with high dose steroids, and the other because of failing to comply with steroid replacement after hypophysectomy. Thyroid stimulating hormone was in the hypothyroid range in eight of 36 patients, although hyponatraemia was attributed to hypothyroidism in only two of these. Clinical information sought included volaemic status (for example, dehydration and oedema), postural hypotension, clues from the history about the likely mechanism of hyponatraemia, and how the patient was treated (for example, fluid restriction, steroids, etc).
Figure 1.
Distribution of urine osmolality results.
Figure 2.
Distribution of urine sodium concentrations.
Urine osmolality was 100 mmol/kg or more in 54 of 59 patients, and was less than 600 mmol/kg in all but one patient, who had septic shock (fig 1). These data raise several issues relating to the usefulness of urine osmolality results in the assessment of hyponatraemia. First, the results obtained from the measurement of urine osmolality merely confirm the presence of impaired water excretion in most hyponatraemic patients. Formal diagnosis of the syndrome of inappropriate secretion of antidiuretic hormone (SIADH) may require the demonstration of a urine osmolality that is inappropriately high for the serum osmolality,3 but it should be obvious clinically when water excretion is not impaired; maximally dilute urine is associated with very high urine flow rates (in excess of 500 ml/hour). Second, impaired water excretion, however it is established, does not in itself establish the mechanism of hyponatraemia. It may signify inappropriate antidiuresis, but is equally consistent with sodium depletion (the hypovolaemia resulting from sodium and water loss is a powerful non-osmotic stimulus to antidiuretic hormone secretion). Thus, knowledge of the patient’s volaemic status is essential for the meaningful interpretation of urine osmolality results. Third, the ability of urine osmolality to discriminate between mechanisms of hyponatraemia may be limited, given the relatively narrow range of urine osmolality (100 to 600 mmol/kg) observed in all but six patients. However, this is speculative, and much larger numbers are required to assess whether this is the case; only two patients were identified with clear evidence of sodium depletion.
In 27 of 45 patients, urine sodium was less than 20 mmol/litre (fig 2). Only 12 patients had urine sodium concentrations in the range typically observed in SIADH (40 mmol/litre or more).4 The combination of impaired water excretion and sodium retention is characteristic of effective circulating volume depletion. Other causes of true hyponatraemia and impaired water excretion are associated with higher urine sodium concentrations (greater than 40 mmol/litre). What do these findings tell us about the prevalence of hypovolaemia in severely hyponatraemic patients? The clinical information we reviewed retrospectively (not shown) was incomplete, and it was often not possible unequivocally to attribute hyponatraemia to a specific cause or mechanism. These limitations also apply in some degree to previous surveys of hyponatraemia, including that of Saeed and colleagues.1,5 Nevertheless, it may come as a surprise that we did not find a greater number of higher urine sodium concentrations in this population. Our findings underline the need for complete relevant information to be collected if the prevalence of different causes and mechanisms of severe hyponatraemia is to be established with any degree of accuracy, and, just as importantly, if the clinical usefulness of urine biochemistry in the evaluation of severe hyponatraemia is to be better defined.
Acknowledgments
The authors would like to acknowledge the help of Mr I Kennedy in collecting the computer data.
References
- 1.Saeed BO, Beaumont D, Handley GH, et al. Severe hyponatraemia: investigation and management in a district general hospital. J Clin Pathol 2002;55:893–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thomas TH, Morgan DB, Swaminathan R, et al. Severe hyponatraemia. A study of 17 patients. Lancet 1978;i:621–4. [DOI] [PubMed] [Google Scholar]
- 3.Bartter F, Schwartz WB. The syndrome of inappropriate secretion of antidiuretic hormone. Am J Med 1967;42:790–806. [DOI] [PubMed] [Google Scholar]
- 4.Rose BD, Post TW. Clinical physiology of acid-base and electrolyte disorders, 5th ed. New York: McGraw-Hill, 2001.
- 5.Crook M, Velauthar U, Moran L, et al. Review of investigation and management of severe hyponatraemia in a hospital population. Ann Clin Biochem 1999;36:158–62. [DOI] [PubMed] [Google Scholar]