We read Dr Cserni’s review of nodal staging for colorectal cancer with interest.1 We have recently performed a multivariate analysis of factors affecting lymph node yield after resection of rectal cancer (unpublished data, 2003) and found positive predictors to be tumour size, pT stage, Dukes’s stage, number of involved lymph nodes, and examination by a histopathologist with a special interest in gastrointestinal malignancy. These are all mentioned by Dr Cserni in his excellent article. Interestingly, although 29 of our patients underwent neoadjuvant treatment (18 short course radiotherapy; 11 long course chemoradiotherapy) this did not appear to affect lymph node yield, despite previous publications to the contrary.2,3 Dr Cserni does not discuss this issue, although an increasing number of patients with rectal cancer are receiving preoperative treatment.
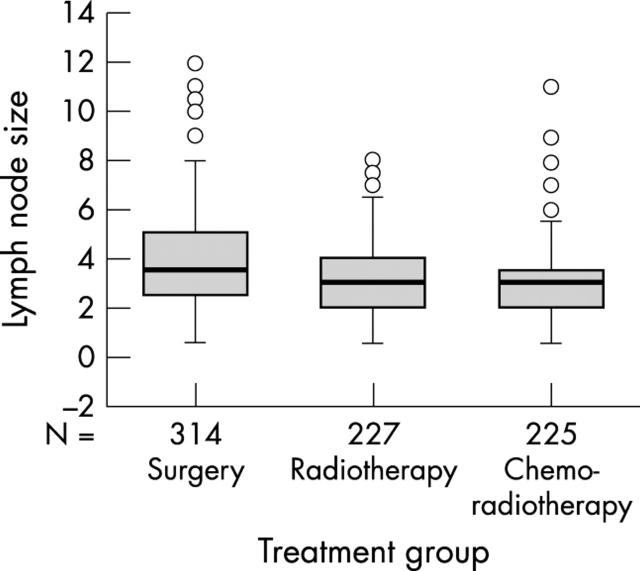
We decided to investigate this further by identifying 15 consecutive cases of rectal cancer resected without neoadjuvant treatment, 13 cases resected after short course radiotherapy (25 Gy in five daily fractions for five days), and 15 patients undergoing chemoradiotherapy before surgery (45 Gy in 25 fractions over five weeks with concomitant 5 fluorouracil based chemotherapy). These were matched for preoperative stage as far as possible (all were T3/T4; N0/N1). Postoperatively, all of the no treatment group were pT3 or pT4 (nine of 15 pN1/2), 11 of 13 short course radiotherapy cases were pT3/4 (five of 13 pN1/2), and 10 of 15 chemoirradiated cancers were pT3/4 (six of 15 pN1/2). The total numbers of lymph nodes found in each group were 314, 227, and 226, respectively. The median numbers of nodes found in each patient in the three groups were 17, 17.5, and 13.5, respectively (not significant; Mann-Whitney U test). The maximum diameter of each node was measured from the histological section on a glass slide with a ruler and expressed to the nearest 0.5 mm. Figure 1 shows the median diameters for each group (surgery only, 3.5 mm; short and long course radiotherapy, 3 mm). Nodes from the short and long course radiotherapy groups were significantly smaller than the surgery only group (p < 0.001; Mann-Whitney U test). Nodes from the chemoirradiated group also showed a tendency to be smaller than those harvested after short course radiotherapy (p = 0.07). Expressed as percentage of nodes < 5 mm in size, 68.7% of nodes from untreated cancers were < 5 mm in diameter compared with 87% of the short course and long course irradiated groups.
Figure 1.
Median diameters of the lymph nodes retrieved from patients treated with surgery only (3.5 mm), short course radiotherapy (3 mm), and long course radiotherapy (3 mm). The numbers of lymph nodes retrieved for each group are shown. The open circles represent outliers.
We conclude from this that both short course radiotherapy and chemoradiotherapy given over four to six weeks can significantly reduce the size of mesorectal lymph nodes, presumably as a result of apoptosis and involution. This will make nodes harder to find, but a careful dissection technique by an interested pathologist will still discover substantial numbers.
This is important because as Dr Cserni points out “small lymph nodes (usually defined as ⩽ 5 mm) may be the only sites of metastases in colorectal cancer specimens”.
References
- 1.Cserni G. Nodal staging of colorectal carcinomas and sentinel nodes. J Clin Pathol 2003;56:327–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wichmann MW, Muller C, Meyer G, et al. Effect of preoperative radiochemotherapy on lymph nodes retrieved after resection of rectal cancer. Arch Surg 2002;137:206–10. [DOI] [PubMed] [Google Scholar]
- 3.Marijnen CAM, Nagtegaal ID, Krandenburg EK, et al. No downstaging after short-term preoperative radiotherapy in rectal cancer patients. J Clin Oncol 2001;19:1976–84. [DOI] [PubMed] [Google Scholar]