Abstract
Aims: Uteri are among the most common surgical pathology specimens. Assessment of the endometrium is often difficult because of pronounced tissue autolysis. This study describes a simple method to prevent endometrial autolysis and aid in interpretation of the endometrium.
Methods: Sixty uteri were injected with formalin using a needle and syringe directed alongside a probe, which was inserted through the external cervical os into the endometrial cavity. Injection was performed on the same day as removal of the uterus. As controls, 60 uteri that were not injected with formalin were examined. The degree of endometrial autolysis was assessed on a four point scale (0–3), with a score of 0 representing no or minimal autolysis and a score of 3 representing extensive autolysis, such that histological interpretation of the endometrium was impossible.
Results: In the injected group, the number of cases with scores of 0, 1, 2, and 3 was 42, 13, four, and one, respectively. The corresponding values for the control group were 17, 23, eight, and 12, respectively. This was highly significant (p < 0.001)
Conclusions: There was significantly less endometrial autolysis in uteri injected with formalin. The use of this simple procedure should be encouraged in hysterectomy specimens.
Keywords: endometrium, uterus, autolysis, formalin fixation
Hysterectomies are commonly performed for a wide variety of benign and malignant conditions. Consequently, uteri are a common surgical pathology specimen in many laboratories. Particularly in large uteri, formalin fixation is often not adequate, and the endometrium may be greatly autolysed as a result of poor permeation of fixative into the endometrial cavity. This often results in difficulties in morphological examination of the endometrium, which in some cases is so autolysed that interpretation is impossible. This is important in all uteri, whether the hysterectomy has been performed for benign or malignant disease. It has been suggested that bisection of the uterus after surgery may improve fixation,1 but this often distorts the specimen, making the assessment of parameters such as the depth of myometrial invasion by tumour problematical. This short report describes a simple method whereby formalin is injected through the external os of the cervix into the endometrial cavity to aid fixation. The degree of endometrial autolysis in these cases was assessed and compared with a control group not injected with formalin.
“Particularly in large uteri, formalin fixation is often not adequate, and the endometrium may be greatly autolysed as a result of poor permeation of fixative into the endometrial cavity”
MATERIALS AND METHODS
Sixty uteri removed for benign reasons, which were received in the pathology department, Royal Group of Hospitals, Belfast, Northern Ireland on the day of surgery, were injected with 10–20 ml of 10% formalin using a needle and syringe that were directed alongside a probe, which had been inserted through the external os of the cervix into the endometrial cavity (fig 1). After 24 hours of fixation these specimens were cut and processed routinely. In general, sections for histological examination included two blocks to show the endometrium and underlying myometrium (unless a gross lesion was seen) and two blocks to show the transformation zone of the cervix, one from the anterior and one from the posterior lip. The degree of endometrial autolysis was measured by two pathologists (JPH and WGM) examining the cases over a double headed microscope. The degree of autolysis was assessed as shown in table 1. A further 60 uteri that had not been injected were randomly selected and this control group was also assessed for endometrial autolysis. A comparison between the degree of autolysis in the two groups was performed using the Pearson χ2 test.
Figure 1.
Method for injection of formalin through external cervical os into the endometrial cavity.
Table 1.
Method of scoring endometrial autolysis in specimens
| Autolysis score | Degree of autolysis |
| 0 | No autolysis or minimal autolysis |
| 1 | Mild autolysis (not affecting interpretation in any way) |
| 2 | Moderate autolysis (affecting interpretation but overall still interpretable) |
| 3 | Severe autolysis (interpretation not possible) |
RESULTS
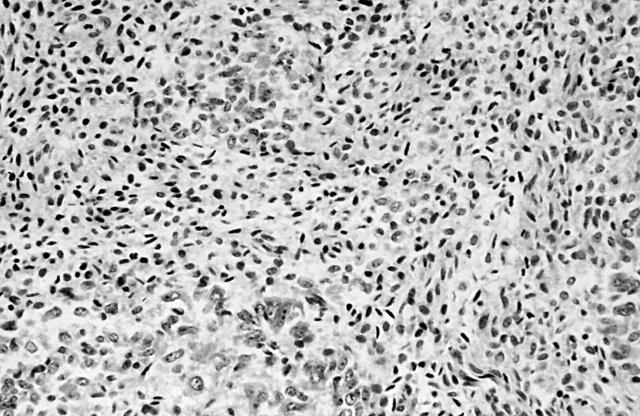
The age of the patients in the injected group ranged from 27 to 76 years (mean, 48) and in the control group from 30 to 79 years (mean, 47). The uterine weight in the injected group ranged from 29 to 886 g (mean, 147) and in the control group from 21 to 683 g (mean, 125). Table 2 shows the degree of autolysis in the injected and control groups. There was a highly significant difference between the two groups (p < 0.001; Pearson χ2 = 24.012). Figure 2 is an example of an autolysis score of 3. The cervical sections were examined in all cases and there was no evidence of artefact or denudation of the surface glandular epithelium.
Table 2.
Degree of autolysis in injected and control groups
| Autolysis score | Injected group | Control group |
| 0 | 42 | 17 |
| 1 | 13 | 23 |
| 2 | 4 | 8 |
| 3 | 1 | 12 |
Figure 2.
Autolysis score of 3, where the endometrium cannot be interpreted.
DISCUSSION
The results of our study indicate that formalin injection of the uterus soon after surgical removal is an effective method of preventing endometrial autolysis. This is a simple procedure, which should be encouraged in all surgically removed uteri. Optimal endometrial preservation is essential for correct interpretation, which impacts upon subsequent treatment and patient management. A degree of autolysis was found in 18 of 60 uteri that had been injected with formalin. Although this was significantly less than in the control group, this indicates that factors other than fixation may affect autolysis. In only five of 60 injected cases did the degree of autolysis affect morphological interpretation (autolysis score of 2 or 3).
Endometrial autolysis is often particularly pronounced in large uteri, where the penetration of formalin is suboptimal. In such uteri, even prolonged fixation in formalin may not improve endometrial morphology. Bisection of the uterus has been advocated to enhance fixation,1 but this may result in considerable distortion and difficulty in evaluating parameters such as depth of myometrial infiltration by tumour.
Take home messages.
We injected uteri with formalin and found that this was a simple method to prevent endometrial autolysis and aid in interpretation of the endometrium
Although endometrial autolysis still occurred in some samples, there was significantly less endometrial autolysis in uteri injected with formalin
The use of this simple procedure should be encouraged in hysterectomy specimens
A theoretical complication of injection through the cervix is artefactual denudation or stripping of the surface cervical glandular epithelium. However, this was not seen in our study, although only representative sampling of the cervix was undertaken. Possible denudation of the surface cervical glandular epithelium has two main implications: (1) when dealing with an endometrial cancer, spread of tumour along the cervical glandular epithelium upstages a tumour to stage 2A, which has implications for management and prognosis, and this may be missed; (2) an endocervical glandular lesion may be missed. In our study, only benign uteri were injected with formalin and clearly further study is necessary to evaluate possible endocervical glandular artefacts in uteri removed for malignant disease.
“A theoretical complication of injection through the cervix is artefactual denudation or stripping of the surface cervical glandular epithelium”
In our study, the uteri were injected in the pathology laboratory. This necessitates rapid transport of the specimen to the laboratory so that injection can be performed before the onset of autolysis. In laboratories where this is not possible—for example, where specimens are transferred from other hospitals—the gynaecologist can be instructed how to undertake the simple process of formalin injection.
REFERENCE
- 1.Rosai J. Appendix H. Guidelines for handling most common and important surgical specimens. In: Ackerman’s surgical pathology. St Louis: Mosby, 1996:2718.